Cartilage damage in the area of the knee joint is a very common clinical picture. There are many causes and numerous symptoms up to chronic pain. For accurate cartilage diagnosis, modern imaging techniques provide the best basis for an exact diagnosis. This provides a good estimate of the type and extent of changes in the articular cartilage.
Osteoarthritic changes of the knee joint are detectable in over 95% of patients in the 6th decade of life on radiographic examination, of which approximately 20% are symptomatic. Overview 1 lists the causes for this [3].
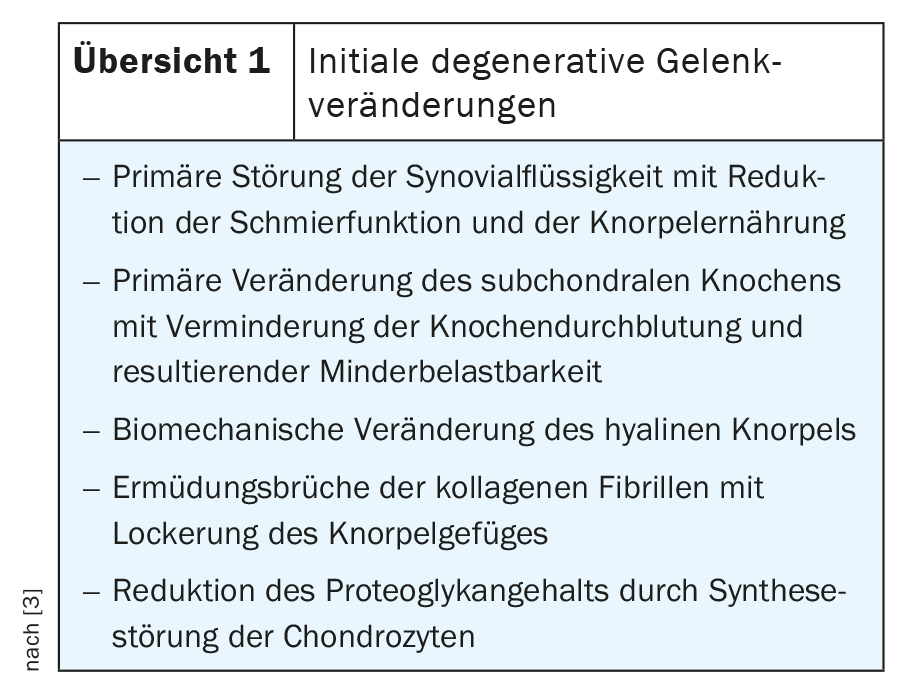
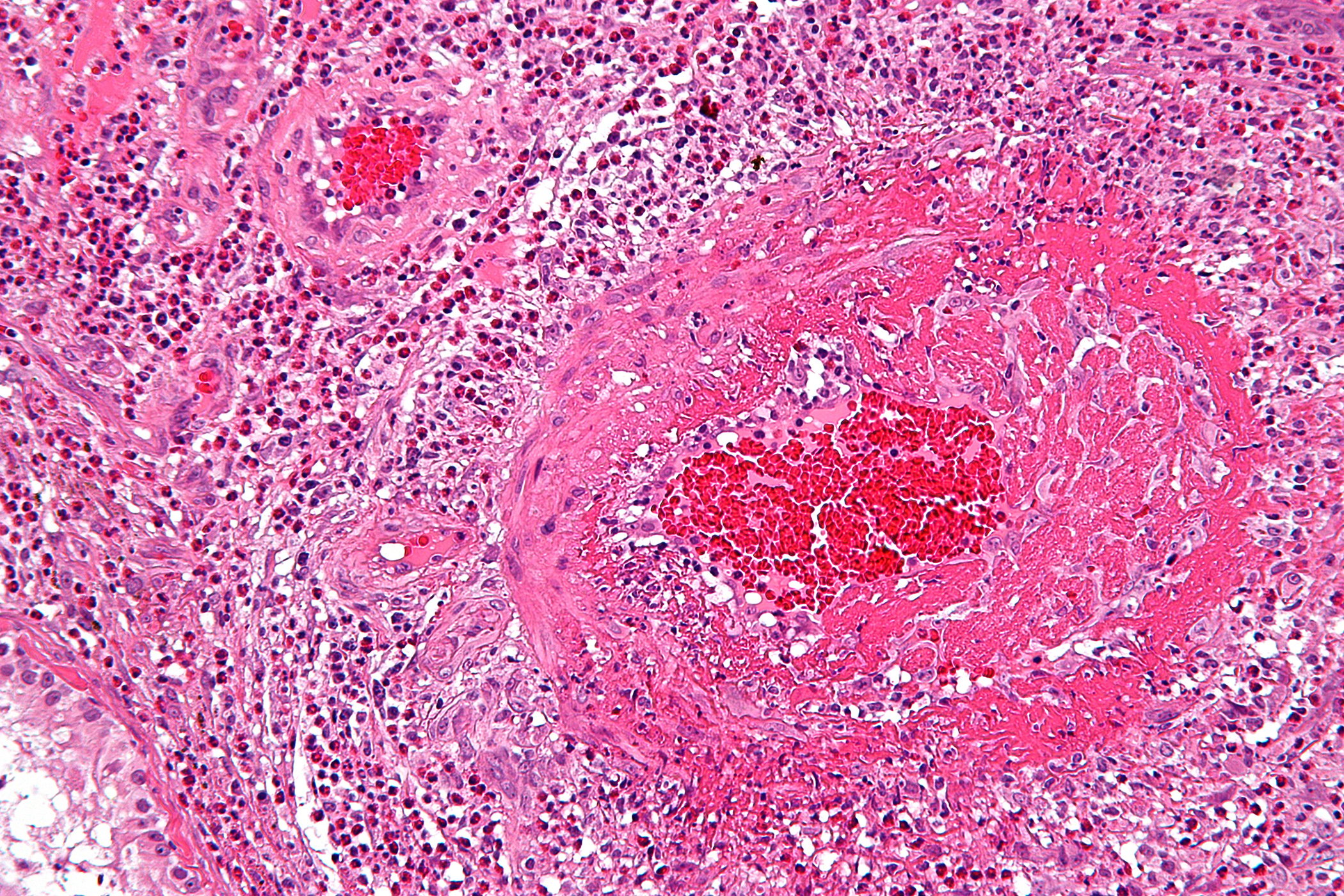
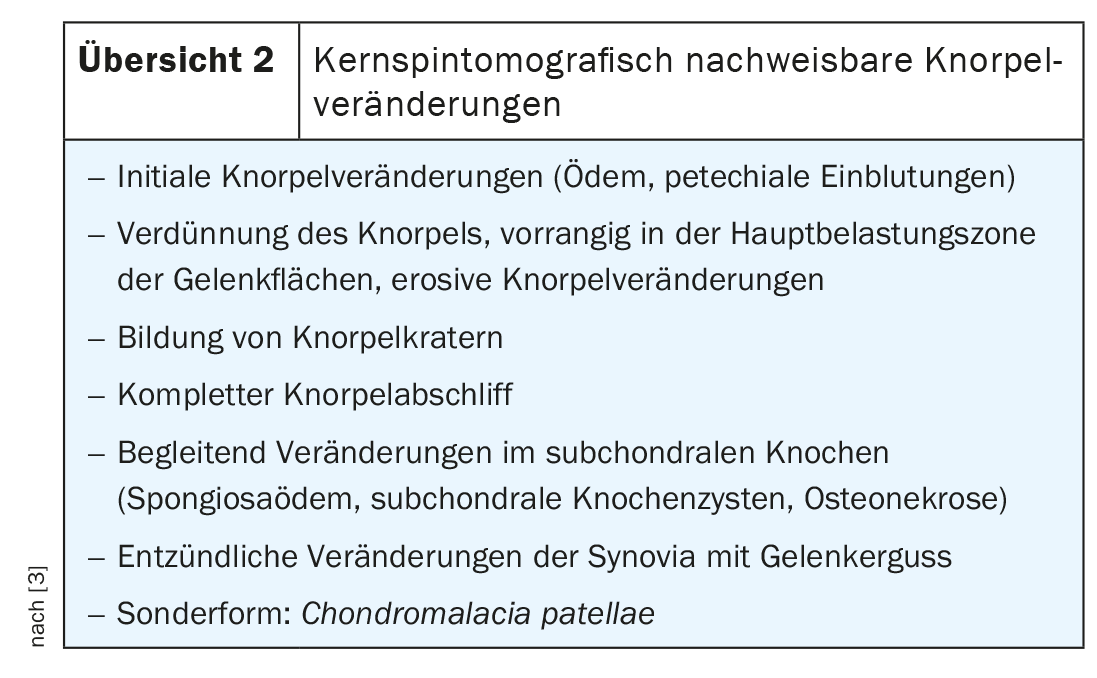
The initial degenerative changes thus take place primarily in the cartilage structures of the joint. The method of choice for imaging, non-invasive diagnosis of cartilage and also meniscus damage is magnetic resonance imaging. Overview 2 lists the cartilage changes that can be detected by imaging.
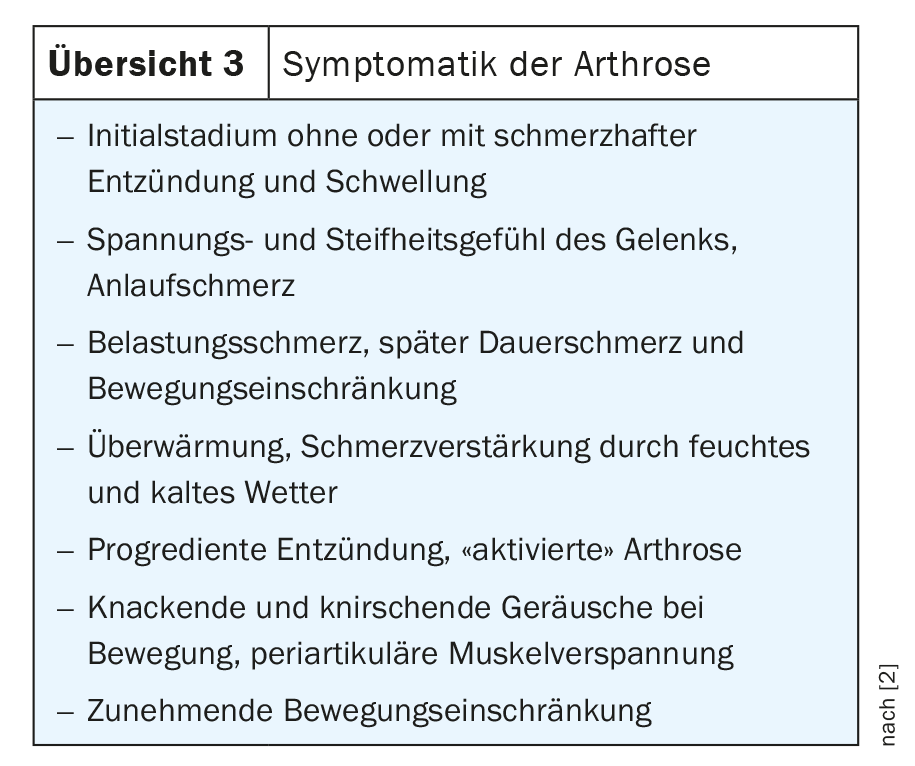
Osteoarthritis in general has significant medical and socioeconomic importance. In Germany, for example, 7 billion euros were spent on the therapy of degenerative joint diseases in 2002 [1]. Overweight, long-term mechanical stress on the joints and malalignment of the axes promote the development of osteoarthritis with all the changes in the joint structures, as do traumas that have taken place and increasing age. Genetic components are also suspected [2]. Clinical symptoms are varied, mild and inconstant in the early stages, and show a progression during the course that varies from individual to individual, in many cases also correlates with imaging findings, and can lead to significant functional limitations (overview 3).
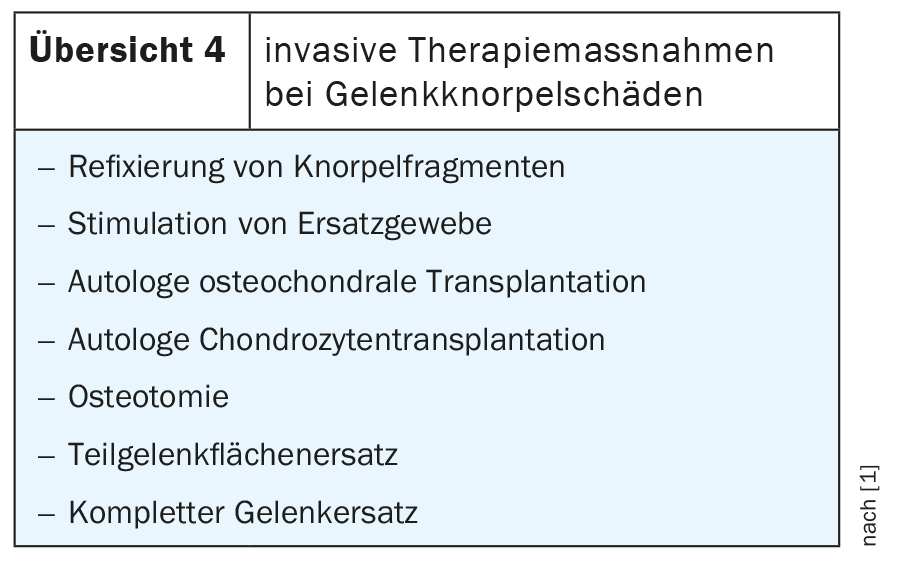
The main strategy of therapy aims to maintain or establish mechanically stable joint congruency and physiological load transmission in the joint. Conservative treatment measures are favored in cases of cartilage that appears intact on imaging, minor superficial changes, and absent or minor articular surface depression. This includes drug therapy with NSAID preparations, physical and physiotherapeutic treatments and relieving measures. In advanced cartilage lesions, various therapeutic options are available for discussion (overview 4).
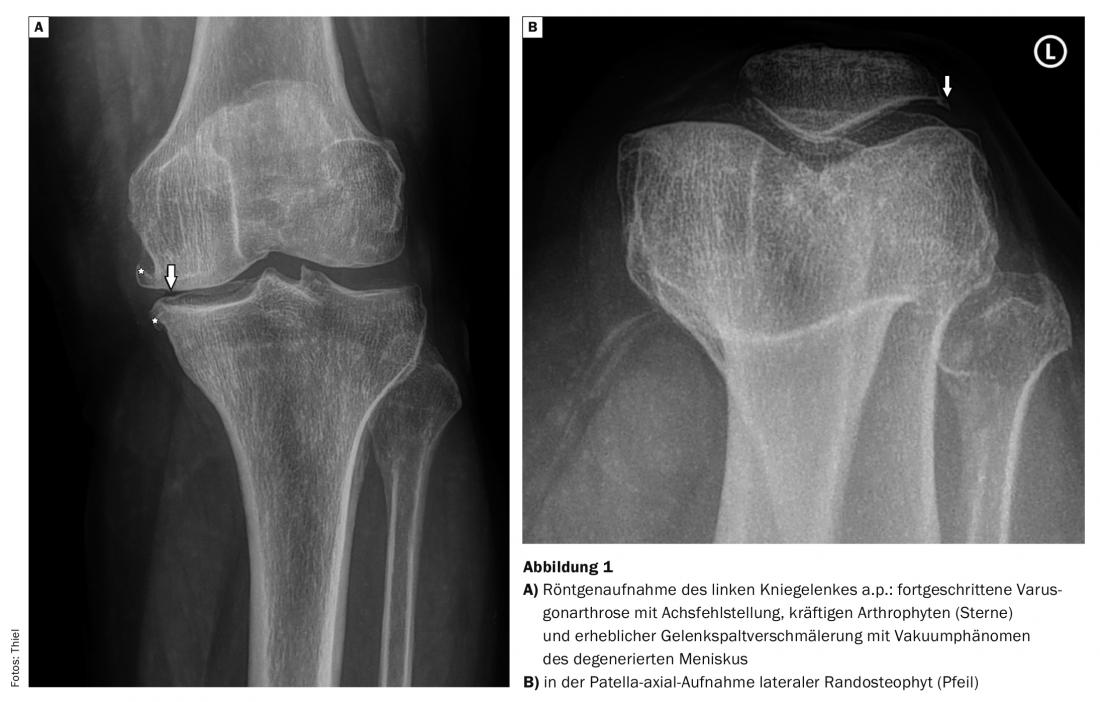
Radiographs initially show narrowing of the joint space in degenerative joint changes, followed by subchondral sclerosis and arthrophytes (Fig. 1A and B) . In the later stage, cysts of the bones in the part near the joint are also visible, occasionally also calcifications within the cartilage structures or meniscal air inclusions, the so-called vacuum phenomenon. If marginal osteophytes larger than 2 mm are detectable in the patella-axial image, there is a 100% probability of ulceration of the retropatellar cartilage.
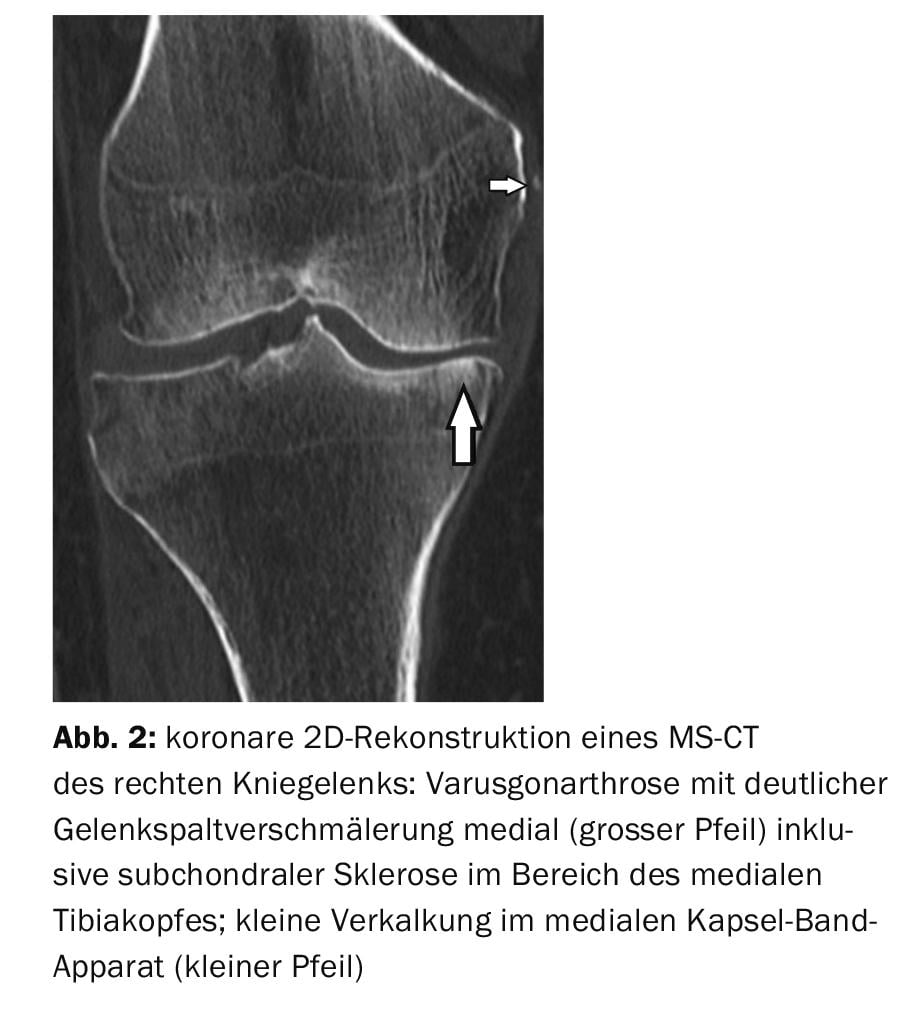
Computed tomographic examinations are rarely requested in the primary diagnosis of degenerative joint changes, also as CT arthrography in contraindications to MRI. Decisive assessment of the cartilage and meniscus structures is not possible (Fig. 2). However, the importance of detecting small calcified or bone-dense corpora libera remains unchanged. After re-ruptures of the anterior cruciate ligament, CT provides accurate information on the width of the drill channels in the distal femur and tibial head for re-operative planning.
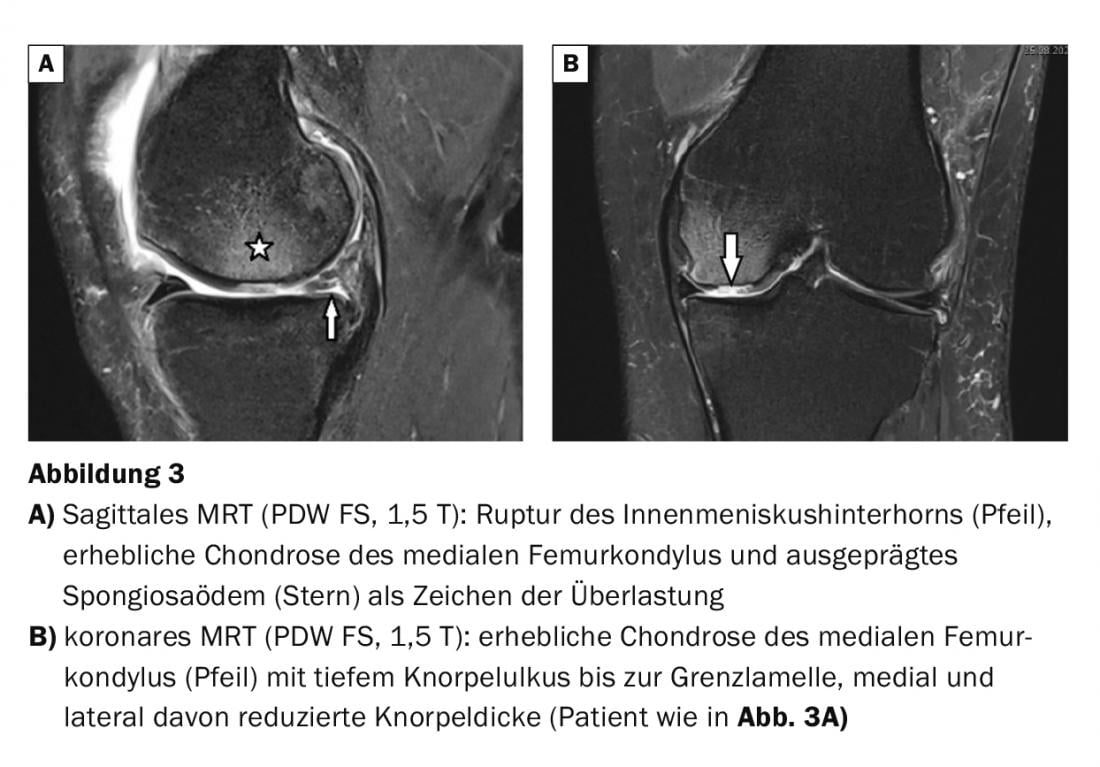
Magnetic resonance imaging provides excellent visualization of all joint structures. Significantly higher sensitivity (93.6 versus 66.6%) and specificity (92.5 versus 71.4%) favor noninvasive MRI compared with arthrography as an invasive imaging modality. In this context, indirect MR arthrography, which has been used for many years in knee joint diagnostics, has also lost importance as a non-invasive method. Cartilage and meniscal damage can be reliably detected (Fig. 3A and B, Fig. 4). Continuous software development and improvement of the hardware today guarantees excellent assessability of the cartilaginous and meniscal structures in addition to the ligamentous, osseous and muscular joint components.

Case studies
Case report 1 demonstrated medially emphasized gonarthrosis including femoropatellar arthrosis in an elderly patient with load-dependent pain and recurrent low-level swelling of the left knee joint (Fig. 1A and B). Case report 2 documents varus gonarthrosis and small ligamentous calcification medially on MS CT, which may be indicative of older trauma (Fig.2). Case studies 3 and 4 show advanced cartilage and meniscus damage in elderly patients without adequate trauma with reactive bony overloads (spongiosaedema) in the joint area (Fig. 3A and B, Fig. 4). Case study 5 reveals inconspicuous cartilage and meniscus conditions of the knee joint in comparison (Fig. 5) with normal cartilage thickness, smooth contour and homogeneous signal.

Take-Home Messages
- The knee joint is one of the most frequently affected joints in degenerative changes.
- Based on the information provided by X-ray diagnostics, MRI as an imaging technique is the method of choice for non-invasive comprehensive imaging of changes in the interior of the joint.
- MR tomography reliably depicts the initial overuse damage (irritant effusion, cartilage and bone edema).
- Computed tomography provides specific complementary information (e.g. intra-articular calcifications, corpora libera).
Literature:
- Thiel HJ: Cross-sectional diagnosis of the joints. Part III: Computer and magnetic resonance imaging diagnosis of degenerative changes of the knee joint. mta Spectrum 7, 2001: 308-310.
- Glaser C: Practicalities of preoperative cartilage imaging. Radiology up2date 2, 2009: 103-109.
- www.orthopaede-baer.de/beschwerden/arthrose, last call 12/14/2020
HAUSARZT PRAXIS 2021; 16(1): 38-40