At the annual congress of the Swiss Society for Medical Laser Applications, which took place as every year at the Hilton Airport Hotel Zurich, one could attend lectures on nevus flammeus, tattoo removal and PRP supportive therapy, among others. The speakers addressed the current standard in therapy and diagnosis and discussed new developments and studies.
“Nevus flammeus is one of the (slow-flow) capillary vascular malformations,” said Nathalie Dietrich, MD, of Zurich, Switzerland, by way of introduction. “Vascular malformations exist at birth and never spontaneously regress.” The nevus flammeus lateralis (“port-wine stains”) is relatively common, highly stigmatizing for the affected, 75% in the head and neck area and may involve the eyelid, which should prompt an ophthalmologic workup for glaucoma. In frontotemporal distribution, Sturge-Weber syndrome is suspected.
What is the therapy for port-wine stains? The gold standard and well known is the pulsed dye laser (PDL). In about two-thirds of cases, this achieves a lightening of 50-70%. However, a good 20% of port-wine stains are resistant to PDL, i.e. do not respond to it at all. And 16-50% may subsequently darken again (neoangiogenesis after laser). Other treatment options besides the pulsed dye laser (585/595 nm) are:
- Potassium titanyl phosphate (KTP) laser (532 nm)
- Frequency doubled Nd:YAG (532 nm)
- Alexandrite (755 nm)
- Nd:YAG (1064 nm)
- Pulsed intense light (IPL)
- Photodynamic therapy (PDT).
“We can improve the result by combining multiple wavelengths, for example,” she said. One example is Cynergy™, which combines dye (595 nm) and Nd:YAG (1064 nm) lasers. The so-called MultiPlex pulsing enables sequential pulsing of both wavelengths. The treatment protocol for “port-wine stains” is summarized in Table 1.

Resistance mechanisms
Factors that decisively influence success are: Patient age, lesion size and localization. “You should treat as early as possible,” Dr. Dietrich advised. According to studies, an average reduction of 63% is achieved in patients under one year of age, and only 43% in patients up to six years of age (after five treatments). Lesions over 40 cm2 respond 23%, while smaller ones (under 20 cm2) regress 67%. A good response is generally expected with localization to the central forehead, temple, lateral to the cheek, neck and chin, V1 and V3 – a poor response with centrofacial lesions, V2. “A poorer response is expected from deeper-lying vessels (appearance purple and pink),” the spokeswoman said. Via dermatoscope, the characteristics of superficial vessels (papillary dermis) are characterized by dots and globules, while those of deep vessels are characterized by their ring structure.
The number of treatments also plays a role with regard to resistance: in the first five, a decrease of up to 55% can be expected, while further treatments show less and less effect (decreases of 18% with five more sessions).
Tattoo removal – what is important?
“A tattoo is a keepsake made to last a lifetime,” said Heike Heise, MD, Düsseldorf, Germany. “The inks used for this vary, as does the particle size of the ink. Basically, it is placed deep into the skin. All of this makes laser tattoo removal challenging.” Q-switched nanosecond lasers are standard, but require a high number of treatments and often don’t allow for complete removal.
“You consequently reach a limit with these systems (Q-switched nanosecond lasers such as ruby laser 694 nm, neodymium:YAG 1064/532 nm or alexandrite 755 nm) at some point, which increases the need for new devices. The picosecond lasers that came on the market in 2014 represented one such innovation.” Indicated, in principle, for the removal of tattoos and permanent makeup on all skin types and many colors such as black, dark blue, brown, purple, red, orange and yellow. For different particle sizes, different pulse durations also work best: large “pigment chunks” respond better to longer pulse durations, while as treatment progresses, the “chunks” become more and more like “crumbs” and can then be addressed very well with shorter wavelengths.
Myths and their elucidation
“However, one must also dispel various myths in connection with the new devices,” the expert explained.
Myth – All colors can be treated with a picosecond laser
Clarification:
- Until now, no picosecond laser system has had three wavelengths
- There is no option of treating all colors or all skin tones with one device
- Treatment of all colors possible in the presence of the alexandrite laser Picosure® (755 nm) and the Nd:YAG laser Enlighten™ (1064 and 532 nm, covers the most common tattoo colors)
- But: Generally somewhat worse response with colored tattoos
Myth – Picosecond laser also leaves scars and hypopigmentation
Clarification:
- Significantly lower incidence of permanent hypopigmentation, especially in skin type IV and V with picosecond laser compared with nanosecond laser (especially at 1064 nm).
Myth – The new picolaser is a cold laser and therefore less painful
Clarification:
- Wrong: Patients tolerate the treatment, but many still find the laser more painful than tattooing itself (especially in sensitive areas)
- Pain management is thus required (local anesthetics, lidogel, NSAIDs, cooling).
Myth – With the picolaser you need a third of the sessions
Clarification:
- Wrong: This statement is usually too optimistic.
- The fact is that you need fewer sessions than with the Q-switched systems, but the number of sessions is very variable individually, especially with multicolor tattoos.
What is the conclusion?
“Picosecond lasers are actually more effective in clinical experience and expand the application options (plus separately paid for technical enhancements such as attachments/upgrades etc.). The capital cost is very high. These are high-end devices with high maintenance and repair costs. For these reasons, acquisition is reserved for specialty practices and clinics. This leads to a need for studies and exchange of experience: comparisons between the previous and the new systems still take place too rarely, which is certainly also due to the cost situation,” the speaker concluded.
PRP and ablative fractional laser
Platelet-rich plasma (PRP) is an autologous blood product with increased platelet content (it contains growth factors and cytokines that have anti-inflammatory and proliferation-stimulating effects, among others). “The key is to separate PRP from erythrocytes and leukocytes as much as possible,” explained Hanno Pototschnig, MD, of Munich, Germany. “Because this threatens undesirable effects due to released/activated proteases and oxygen radicals.”
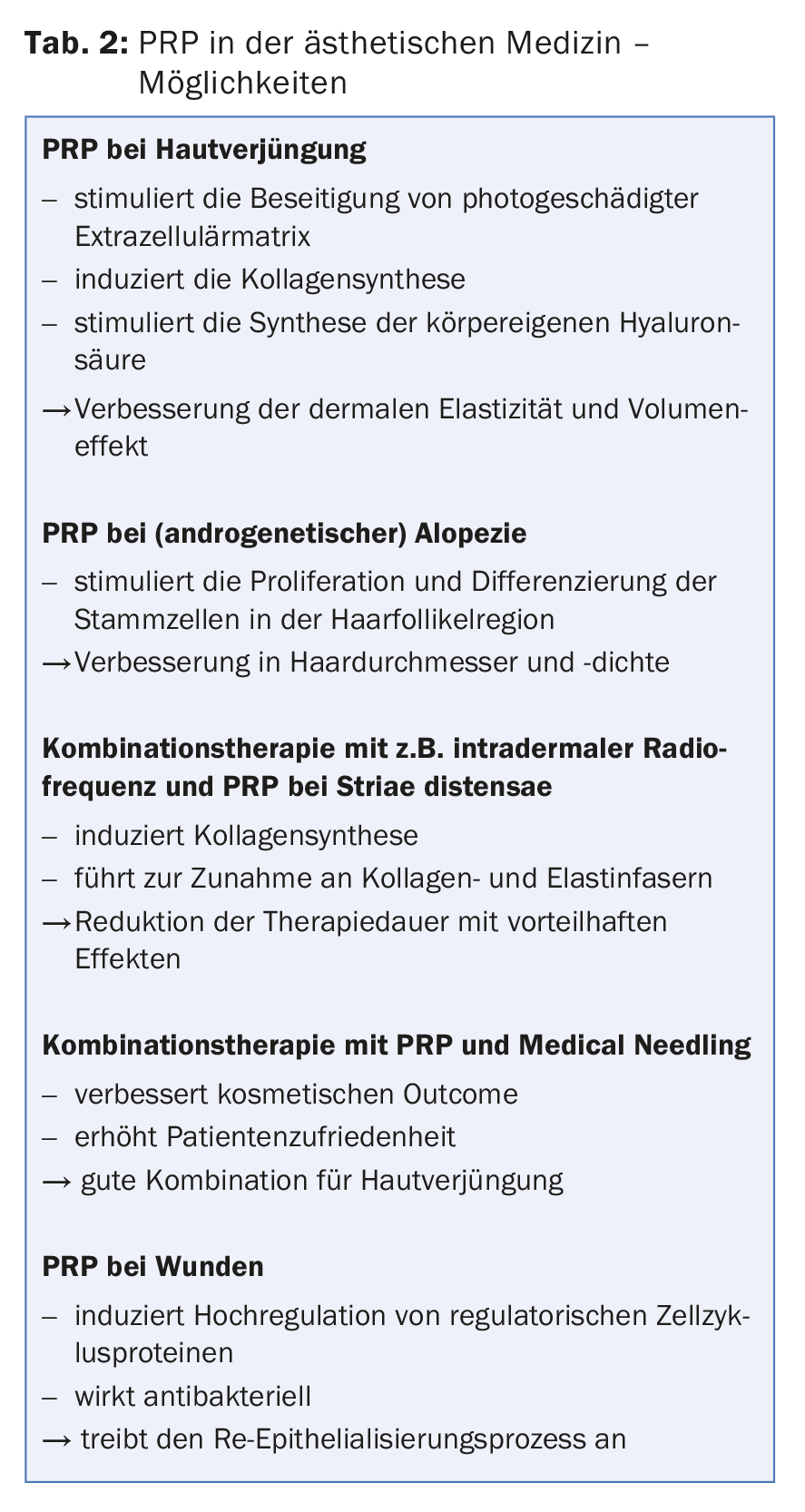
The possible field of application of PRP is large, both as a combination therapy and as a monotherapy. Dr. Pototschnig named some of these areas of application from aesthetic medicine (Tab. 2) and referred to a comprehensive review on the topic by Leo MS et al. published in 2015 [1]. There are also corresponding indications of a positive additive effect of PRP in wound care [2].
Bettina Rümmelein, MD, SGML President, Kilchberg, went into more detail about the combination with laser therapy – and in particular ablative fractionated lasers (AFXL). A distinction must be made between two techniques: In so-called “laser-supported drug delivery”, PRP is introduced into the skin via fractional laser therapy instead of by injection. After laser treatment, it can also be reinjected and used supportively to improve wound healing or reduce downtime (e.g. with the aid of a double syringe). The following treatment steps are followed in the latter process:
- Blood is drawn during the pre-anesthetic phase (disinfection, gloves, sterile drape).
- Syringe centrifugation
- Carefully remove the syringe and draw up the autologous conditioned plasma (ACP) into the inner plunger of the double syringe
- Inner syringe is now ready for PRP application.
- After laser treatment, PRP leads to a proliferation-increasing effect as well as a better cosmetic, histological and subjectively perceived result and it reduces downtime.
“By drawing and preparing the blood during the pre-anesthetic phase, you don’t waste any time, and after the fractional laser treatment, PRP is applied in just a few minutes. I reinject two-thirds of the PRP and massage the remaining third into the skin,” she says. “Our experience is good, both from the physician and patient side. So PRP and fractional laser are a good combination for skin rejuvenation.”
A publication comparing injection and topical application of PRP (for atrophic acne scars) was by Gawdat HI et al. [3]. It concludes that the positive effects of both types of application are comparable, but the patient burden with topical application is lower (significantly lower pain scores).
Source: Laser Congress SGML 2017, January 19, 2017, Zurich
Literature:
- Leo MS, et al: Systematic review of the use of platelet-rich plasma in aesthetic dermatology. J Cosmet Dermatol 2015 Dec; 14(4): 315-323.
- Picard F, et al: The growing evidence for the use of platelet-rich plasma on diabetic chronic wounds: A review and a proposal for a new standard care. Wound Repair Regen 2015 Sep; 23(5): 638-643.
- Gawdat HI, et al: Autologous platelet rich plasma: topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg 2014 Feb; 40(2): 152-161.
DERMATOLOGIE PRAXIS 2017; 27(1): 30-32











