When acute exacerbations occur in COPD patients, antibiotics are often the first-line treatment. However, their use is always associated with the risk of potentially unfavorable effects. Researchers have investigated the possibility of using CRP measurement before the possible start of antibiotic administration to reduce its necessity.
According to the GOLD recommendations, antibiotics (according to the Anthonisen criteria) should be used either in patients with the three cardiac symptoms of increase in dyspnea, sputum volume, and purulent sputum, or in patients with two of these symptoms if the increase in purulent sputum is one of them. If a patient is so severely impaired that he or she must be treated in the intensive care unit, antibiotics should be used as a matter of principle, regardless of the clinical constellation.
A general practitioner-level study [1] addressed the question of the extent to which C-reactive protein (CRP) can be used as a biomarker for or against the use of antibiotic therapy. 653 patients from England and Wales diagnosed with COPD were randomized into two groups: The first group underwent a so-called point-of-care test in GP practices with an immediate response after 10 minutes. Based on this result, a recommendation pro or contra antibiotics was made. In contrast, the control group was treated with standard therapy according to the usual criteria. The recommendations given to colleagues were divided according to CRP level
- <20 mg/l: no recommendation on antibiotics, as the probability of efficacy is considered low.
- 20-40 mg/l: antibiotic use may be considered (purulent sputum is mentioned here as an additional decision criterion).
- >40 mg/l: Antibiotic use is very likely to be helpful
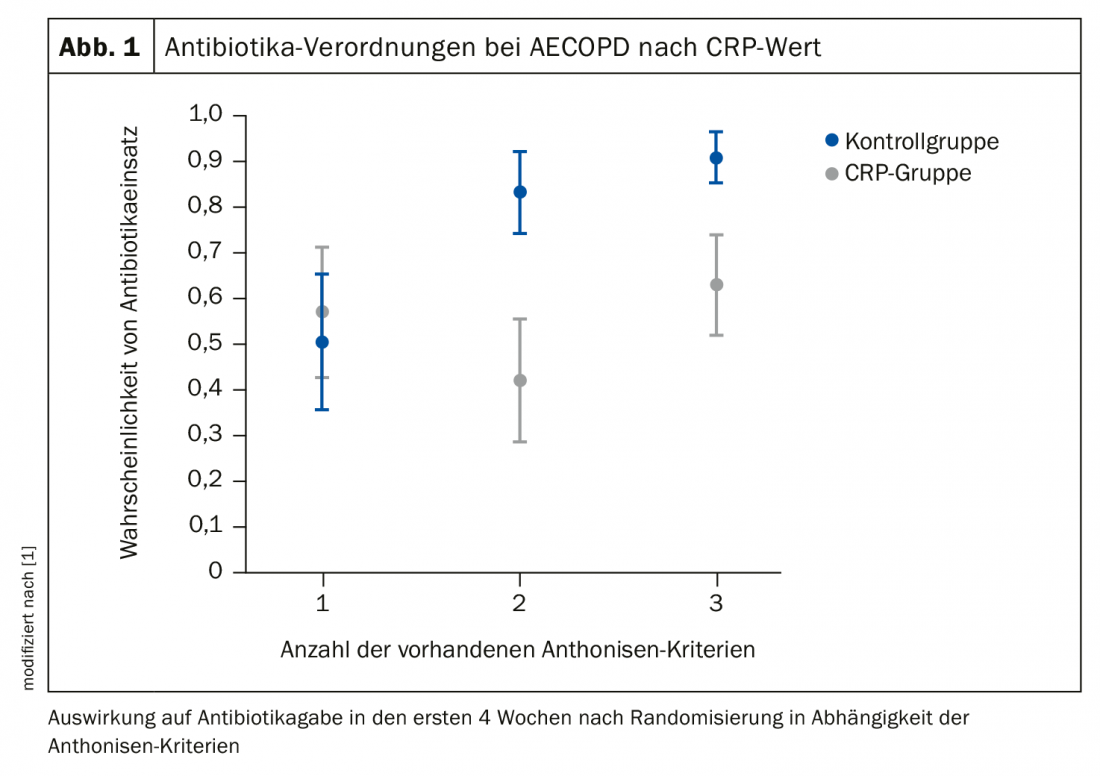
The result of the evaluation: using the described CRP algorithm, patients in the CRP group received significantly fewer antibiotics (57%) compared to the control (77.4%) (Fig. 1) . The probability of antibiotic prescription was thus reduced by 31%.
The second study [2] had a similar approach, but included only patients (n=220) who presented with acute COPD exacerbations and were hospitalized. Again, CRP was measured and either the GOLD strategy was used or a CRP value ≥50 mg/l was taken as an indicator of antibiotic use. Endpoints included antibiotic use in the first 24 hours, rate of 30-day treatment failure, duration of hospitalization, and time to next exacerbation.
This study also found that significantly fewer patients received antibiotics in the CRP-guided group (n=101), 31.7%, than in the GOLD group (n=119), 46.2% (p=0.028). The 30 day treatment failure rate was nearly identical (44.5% CRP vs. 45.5% GOLD, p=0.881). Thus, it has also been shown that there is no harm to the patient and there is no increase in therapy care when the CRP strategy has been followed.
In summary, despite the different settings of the two studies (different countries of origin, different severity of disease in patients), the effect of CRP testing was approximately the same. The use of the protein as a biomarker thus appears to work and be worthwhile in that it can be used to significantly and clinically relevantly reduce the use of antibiotics. There is also no evidence that this strategy is associated with risks to the patient.
Source: Pneumo-Update, Mainz (D)
Literature:
- Butler CC, et al: N Engl J Med 2019; 381: 111-120.
- Prins HJ, et al: Eur Respir J 2019; 53(5).











