DPP4 inhibitors are often used to control blood glucose levels. An increasing number of papers have reported the risk between DPP4 inhibitors and acute pancreatitis (AP); however, the evidence is limited and mixed with other common causes of AP. In particular, linagliptin and its association with AP has not been thoroughly investigated. US physicians describe a case of linagliptin-induced AP that resolved after discontinuation of the drug.
Although the mechanism of DPP4 inhibitor-induced AP is not definitively known, one theory is that prolongation of GLP1 half-life induces alpha cell proliferation with subsequent tubular projection, ductal cell hyperproliferation and obstruction. This leads to increased congestion and inflammation in the pancreas. Only three cases of linagliptin-associated AP have been published in the literature. However, some of these reports are limited and contradictory.
A 60-year-old African-American female presented to the team of Dr. Husam El Sharu, ECU Health Medical Center/Brody School of Medicine, Greenville, North Carolina, USA, with the chief complaint of progressively worsening acute epigastric pain radiating to the back that persisted for a day, associated with nausea, vomiting and decreased oral food intake [1]. She took the proton pump inhibitor pantoprazole without any relief. In the medical history, she did not report fever, chills, previous similar pain, a recent illness, abdominal trauma, alcohol consumption or the use of illegal drugs.
The woman had insulin-dependent type 2 diabetes, hypertension, stage 4 chronic kidney disease, coronary artery disease, a coronary bypass graft and a cholecystectomy. Her diabetes medications included insulin detemir and lispro as well as linagliptin, which she had started 2 months prior to presentation. Other drugs included amlodipine, ASA, atorvastatin, carvedilol, bumetanide, duloxetine, hydralazine, isosorbide mononitrate and lisinopril.
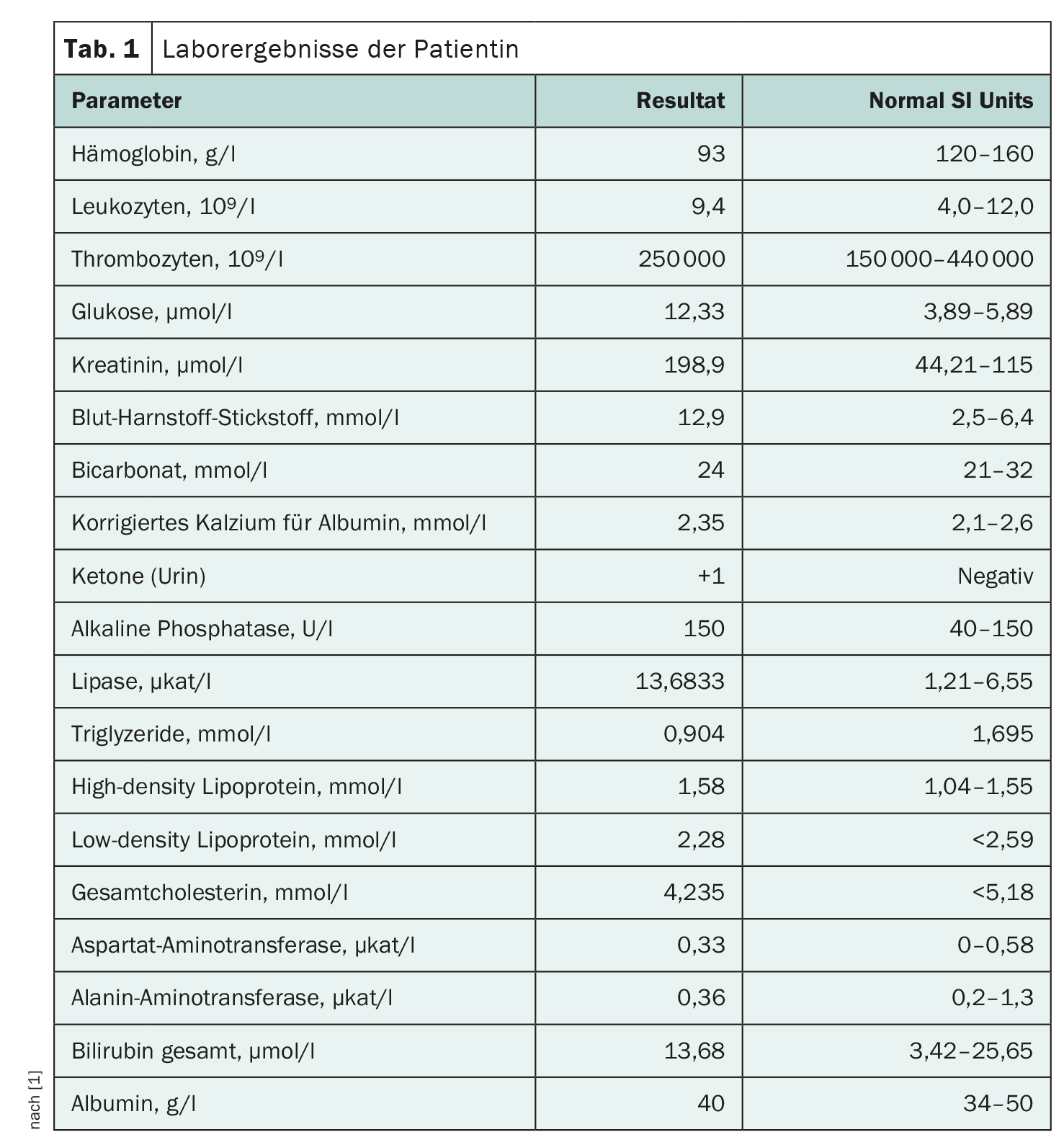
On admission, the patient’s vital signs were within the normal range. She was in acute distress with dry mucous membranes and reduced skin turgor. No rash or jaundice was detected. Abdominal examination revealed only general tenderness, which was most pronounced in the epigastrium, without rebound or guarding, and no palpable organomegaly. The lipase value was 13.6833 µkat/l, and the triglycerides were 80 mg/dl and 0.9 mmol/l respectively. The other laboratory results are listed in Table 1 .
The AP disappeared with the discontinuation of linagliptin
Computed tomography of the abdomen and pelvis with intravenous contrast showed no acute pancreatic abnormalities and a surgically absent gallbladder without significant biliary dilatation. According to the revised Atlanta criteria, the diagnosis of AP was made on the basis of a typical clinical picture and a lipase that exceeded three times the upper limit of the norm.
The patient was given adequate intravenous fluids and painkillers. Linagliptin, bumetanide and lisinopril were initially discontinued, but hydralazine, carvedilol and atorvastatin were continued. As the patient’s condition improved, her diet was gradually resumed. Her stay was complicated by acute kidney injury with a peak creatinine level of 3.73 mg/dl, which improved to 2.91 mg/dl on discharge. The laboratory values normalized steadily. The patient’s abdominal pain disappeared during her hospital stay, which lasted 5 days. At the follow-up examination in hospital, the patient was again treated with medication, with the exception of linagliptin, which did not lead to any further episodes of pancreatitis. One month later, the lipase was measured again and was within the normal range.
Linagliptin is excreted via the liver, in contrast to DPP4 inhibitors, which are excreted via the kidneys. Interestingly, relatively few cases of AP are associated with linagliptin. This observation could be due to the unique elimination mechanism or the relatively lower use compared to other DPP4 inhibitors, Dr. El Sharu and his colleagues write. In addition, this observation could be affected by the higher prevalence of CKD in patients with diabetes, leading to other DPP4 inhibitors being reported more frequently. Nevertheless, further studies are needed to confirm these results, the authors emphasize.
Incretin-based drugs are well-known active ingredients that are used for glycemic control in patients with type 2 diabetes. Of these drugs, glucagon-like peptide 1 agonists are known to be associated with pancreatitis. However, a similar connection with dipeptidyl peptidase-4 inhibitors is controversial. Linagliptin in particular has not been sufficiently documented in the available literature. It is therefore important to take this connection into account when prescribing these drugs in clinical practice.
Literature:
- El Sharu H, Hidri S, Peltz J, Alqaisieh M: Linagliptin-Induced Pancreatitis. AIM Clinical Cases 2023; 2: e230316; doi: 10.7326/aimcc.2023.0316.
InFo DIABETOLOGY & ENDOCRINOLOGY 2024; 1(2): 36-37