At the Swiss Family Docs Congress, André Seidenberg, MD, Zurich, and Philip Bruggmann, MD, Zurich, presented a workshop on addiction medicine. The focus was not on addiction per se, but on the somatic concomitant diseases from which many addiction patients suffer. Diseases such as COPD, liver cirrhosis and chronic infections often limit the life expectancy of patients.
(ee) At the beginning of his presentation, Dr. Philip Bruggmann, MD, Arud, Centers for Addiction Medicine, Zurich, a question: Which substance has the greatest long-term toxicity – alcohol, cocaine, CrystalMeth or cannabis? Opinions in the audience were divided, but ultimately alcohol (along with tobacco) turned out to be the most harmful “drug.” In the public’s perception, hard drugs such as heroin or cocaine are considered particularly dangerous, but the speaker put this into perspective, saying that only 10-20% of people who use illegal substances also develop an addiction.
COPD and liver disease
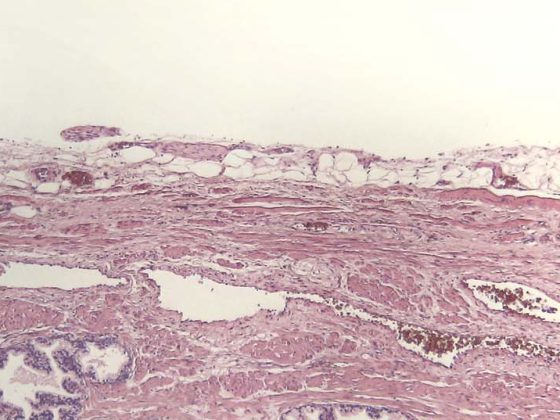
For the long-term course of addicts receiving substitution treatment, the liver and lungs are the limiting organs. 98% of these patients smoke, and many develop COPD, which is often poorly noticed and diagnosed too late, in addition to other health problems. The speaker advocated addressing the topic of “quitting smoking” with these patients as well and motivating them to do so. Liver failure is one of the most common causes of death among individuals receiving care at addiction medicine centers. The liver is stressed by many factors in addicts: Alcohol, HIV and hepatitis C infections, smoking, intravenous drugs, medications and obesity as a side effect of drug therapies. Smoking cannabis further promotes cirrhosis of the liver.
Hepatitis C
Among methadone users, the prevalence for HCV infection is 50% and for HIV infection is 10%. Heterosexual transmission of hepatitis C virus (HCV) is very rare – this information may reassure patients who fear infection because of sexual contact with an HCV-positive person. Transaminase levels are a very poor indicator of possible HCV infection because the majority of HCV patients already have detectable liver damage (fibrosis) despite normal transaminases. Therefore, antibodies should be determined when looking for chronic HCV infection. In Switzerland, about 50% of all chronic infections with HBV and HCV are undetected, so it is worthwhile to have an appropriate clarification if there is a corresponding suspicion. Common symptoms of hepatitis C include fatigue, depression, weakness and pain around the liver.
What to do in case of accidental stab wounds?
“Your practice assistant pricked herself with a needle 20 minutes ago. The index patient has been using intravenous heroin for years, he is cachectic, his serology regarding HIV and HCV is unknown – how do you proceed?” Dr. Bruggmann used this practical example to explain the procedure for accidental stab wounds. In principle, HBV is ten times more contagious than HCV, and HIV is the least contagious. Nevertheless, if a needlestick injury occurs with a high-risk HIV infected patient (as in the case presented), it is important to begin HIV postexposure prophylaxis (PEP) immediately, because every hour counts in this situation. If the index patient is known, he or she can be tested for HIV, and if the text is negative, PEP is stopped. With regard to HBV risk, vaccinated individuals are likely to be protected from infection for life if their anti-HBs titer has been 100 IU/l at least once >. Therefore, checking the titer one month after vaccination is important. To diagnose possible HCV infection, baseline serology should be performed on both the MPA and the index patient after a stab wound. Subsequently, an HCV RNA test is performed every four weeks for six months to exclude a possible acute hepatitis C or to detect a possible acute hepatitis C infection. to diagnose. It is also important to report the stabbing injury to the accident insurance company.
An unusual death
Dr. med. André Seidenberg, Capitol Practice, Zurich, introduced his presentation with an impressive case. A 29-year-old patient with years of drug dependence (opioids, alcohol, cocaine, benzodiazepines, substitution with morphine) and a host of other diagnoses (including personality disorder, depression, contagious impetigo, rhinopathy, chronic hepatitis C, contact allergy to rubber and soot) presented to the practice for a cut on his foot. The patient was agitated, impatient, sweating, had episodes of fever, nodded off and abruptly startled back up, urine sample was positive for opiates, cocaine, benzodiazepines, and methadone (the latter not prescribed). None of this was unusual in this patient, who had been known in the practice for a long time. Two days after wound care, the medical officer phoned to say the patient had been found dead in his apartment. Immediately the question arose as to the cause of death: overdose? If so, by what substance? Suicide? Cardiac arrest? Brainstem insult caused by cocaine? Sepsis? Murder (the patient moved in dealer circles)? Ultimately, it turned out that the patient had died of undiagnosed malaria, with which he had contracted during a stay in Nigeria – presumably in the course of his dealing activities.
Early age diseases
This case study shows well that drug use masks, mimics, and causes many diseases. Treatment is complicated by several factors: decreased adherence, behavioral problems, violence, and financial problems.
In Switzerland, the heroin epidemic was at its peak in 1992-94. At that time, 750-1000 people died per year because of illegal drug use – the most common cause of death among middle-aged people! Of those addicted to opioids, less than 5% became permanently abstinent. Today, the majority of these individuals are around 50, and most are not only addicted to opioids (often in substitution treatment) but also use cocaine and other stimulants. Mixed use with benzodiazepines and/or alcohol is also common. Many suffer prematurely from the effects of old age and drug use. Almost any organ can be affected by the drugs, including CNS (paralysis, epilepsy, abscesses), vessels (vasculitis, phlebothrombosis, infected ulcers) and heart (endocarditis, arrhythmias). Often the teeth and gums of drug addicts are in poor condition (gingivitis, caries) due to insufficient hygiene.
Damage due to unfavorable consumption circumstances
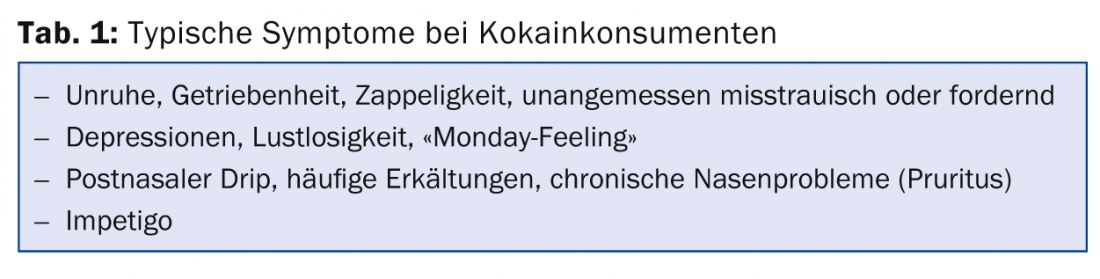
Cocaine users also often show typical symptoms (tab. 1) . However, psychiatric codiagnoses are rarer in cocaine users than in opioid addicts, and cocaine users can often hide their problems for a long time. At least 80% of persons receiving methadone in a specialized addiction center have a psychiatric diagnosis such as personality disorder, borderline syndrome, ADHD, etc. In contrast, methadone users who are cared for in family doctor’s offices are not particularly conspicuous psychiatrically.
It is important to note that the physical harm caused directly by the substance is greater with cocaine than with opioids. In the case of opioids, the majority of damage to the body is caused by the adverse circumstances of use, not by the substance itself. The speaker emphasized that forced opioid abstinence is unfavorable and not something to strive for. The risk is great that drug users will begin to use again after abstinence, at doses that they previously tolerated but that may lead to death from overdose after abstinence.
Source: Swiss Family Docs Conference, August 28-29, 2014, Zurich
GP PRACTICE 2014; 9(10): 37-38