The heterogeneous group of acquired clonal diseases of the hematopoietic stem cells of the bone marrow (myelodysplastic syndromes) are associated with an increased risk of acute myeloid leukemia or bone marrow failure with cytopenia. Myeloproliferative neoplasms, on the other hand, are diseases of the hematopoietic stem cell that persist for life. Their etiology is not known. The majority of cases are diagnosed in a chronic phase of the disease. It should not come to that.
Myelodysplastic syndromes (MDS) are clonal hematopoietic stem cell diseases characterized by cytopenia and a tendency to leukemic development. The maintenance of telomeres, which protects cells from proliferation arrest and senescence, depends on high telomerase activity in cancer cells. Imetelstat, a 13-mer oligonucleotide, binds specifically to the template region of the RNA component of human telomerase and acts as a competitive inhibitor of the enzymatic activity of telomerase. In a Phase II clinical trial, 37% and 23% of 57 highly transfused lower-risk MDS patients achieved 8-week and 24-week transfusion independence (TI), respectively, with a median TI duration of 65 weeks. 65% achieved a hematological improvement of the erythrocytes. A subgroup has now been analyzed in more detail to identify biological pathways associated with clinical response [1].
Twenty-four BM MNC samples from 10 patients, including six 1-year TI responders (TIR) and four 8-week TI non-responders (TINR) at baseline and after 4-7 months, were analyzed for transcriptomes by RNA sequencing. Transcriptome analysis identified 1185 DEGs (35 upregulated and 1150 downregulated in TIR versus TINR). Using GSEA, pathways involved in the positive regulation of innate immunity, type I/II IFN response and T and NK cell-mediated cytotoxicity were downregulated in TIR; using IPA, the canonical pathways TREM1, CREB and NFκ-B were downregulated, suggesting that innate immunity and inflammation were suppressed in TIR. Accordingly, the baseline levels of the proinflammatory chemokines IL-18 and CXCL9 were lower in TIR. Compared to baseline, 4-7 months of imetelstat treatment resulted in upregulation of signaling pathways involved in T cell activation, B cell proliferation and negative regulation of IL-6 and IL- 1β production in TIR.
Immunoprofiling by mass cytometry identified 32 clusters and UMAPs captured the heterogeneity of the samples. At the start of treatment, there were no differences in the proportions of B, T and NK cells, but the proportion of CD4+ effector memory T cells and HLA-DR-CD14+ monocytes was higher with TIR than with TINR. After two cycles of treatment, IL-4, the B-cell stimuli IL-5 and IL-27 increased independently of the response and the S100A8/A9 heterodimer decreased in TIR. After 4-7 months of treatment, an increase in B cells, CD8+ terminal effector T cells and a decrease in HLA-DR monocytes was observed in TIR, while TINR showed an inflammatory signature with increased TNFα levels and a decrease in anti-inflammatory IL-1RA.
Serum lactate dehydrogenase as a prognostic factor
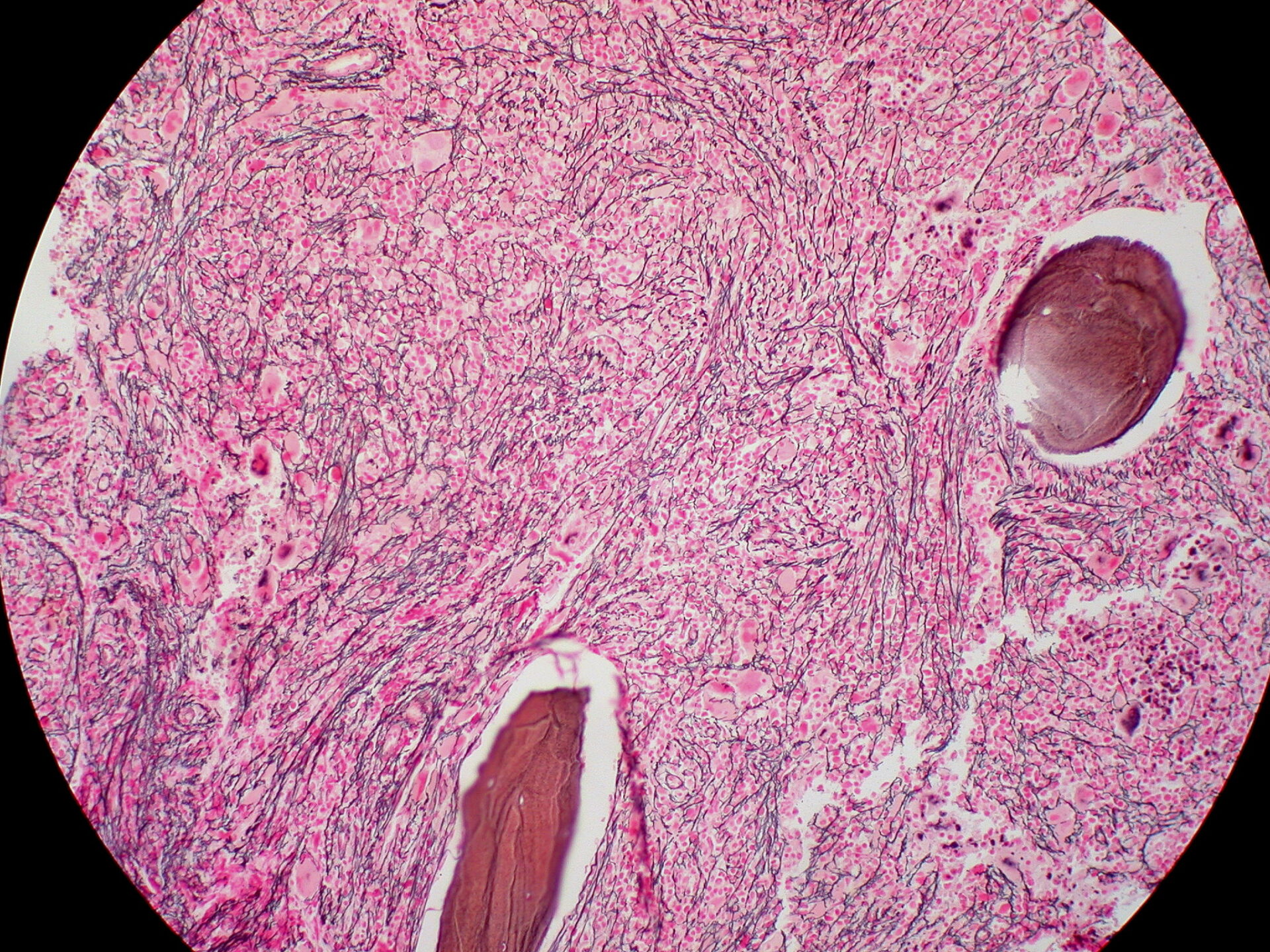
Primary myelofibrosis (PMF) is a myeloproliferative neoplasm that is usually associated with an unfavorable prognosis, as the most threatening complication of PMF is that it can develop into acute myeloid leukemia. The latest evidence suggests that elevated serum lactate dehydrogenase (LDH) levels at the time of initial diagnosis of PMF have a significant correlation with poor prognosis and leukemic progression (LP). However, a precise cut-off value for the use of LDH in serum for the prognosis of PMF has never been established.
One study aimed to characterize a cohort of patients with PMF – diagnosed in a central hospital between 2010 and 2017 and followed up until 2022 – and investigate a possible association between elevated serum LDH levels and LP as an early event, within the first five years after initial diagnosis of PMF [2]. The optimal cut-off value for clinical practice should then be determined. A total of 53 patients met the criteria, with a mean age of 68 years, 62.3% men, a mean LDH serum level of 414 U/L. LP occurred in 15.1% of patients within five years. In the univariate analysis, the probability of LP within 5 years increased by 0.6% with each increasing U/L of serum LDH. In the multivariate analysis, which only considered the variables of the Dynamic Prognostic Scoring System (DIPSS), serum LDH retained its significance. A cut-off value for serum LDH was calculated at 522 U/L, with a sensitivity and specificity of 75% and 80%, respectively.
Congress: European Hematology Association (EHA)
Literature:
- Chapuis N, et al.: Modulation oft he immune landscape in lower.risk myelodysplastic syndromes with imetelstat-induced transfusion independency. HemaSphere, 2023;7(S3): 158–159.
- Moura P, et al.: Primary myelofibrosis: serum lactate dehydrogenase as a predictor of early leukemic progression. HemaSphere, 2023;7(S3): 4147.
InFo ONKOLOGIE & HÄMATOLOGIE 2023; 11(6): 32
Cover picture: Ed Uthman, Wikimedia