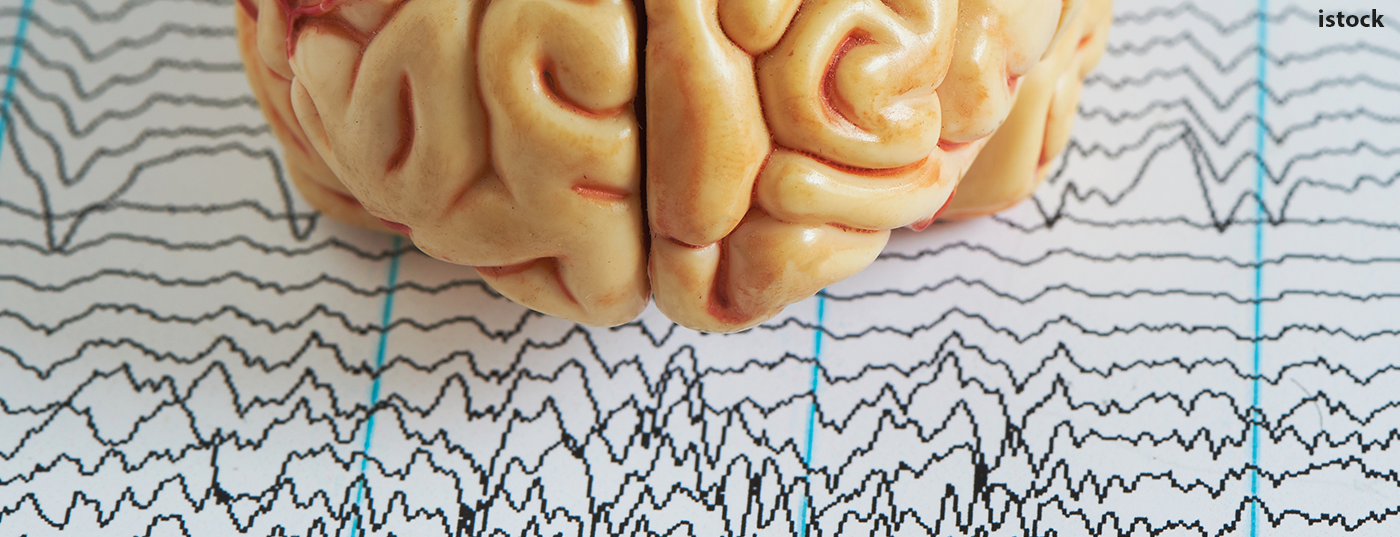
The range of therapies for generalized and especially focal epilepsies is constantly expanding, so that the treatment regime can now be individually adapted to the needs of those affected. However, in addition to pure efficacy, other aspects should also be taken into account in the treatment decision in order to detect the most effective approach in each case. The early use of monotherapy continues to play a major role.
In the therapeutic management of epilepsy, there has been a certain dogma since the 1970s that monotherapy should be given preference over combination treatments. The background lies in a proof provided at that time that the same efficacy can be achieved with monotherapy as with the polytherapies commonly used at that time, without the risk of sometimes considerable pharmacokinetic interactions, reported Prof. Andreas Schulze-Bonhage, MD, Freiburg (D). Due to strong enzyme inductions, there were always considerable losses in the efficacy of the combination treatments at that time. In addition, monotherapy facilitates adherence, which increases adherence. However, it cannot be postulated in principle that monotherapy has better efficacy or tolerability compared with preparations that can be combined well, the expert said.
- Monotherapy is induced mainly in three scenarios:
- In the initial treatment of newly diagnosed epilepsy,
- Switching from a pre-existing treatment that is not effective or not tolerated to another preparation,
- The reduction of a pre-existing combination therapy.
The advantages are the avoidance of complex pharmacokinetic and pharmacodynamic interactions and the reduction of side effect rates. Treatment is indicated according to the current epilepsy definition after two unprovoked seizures at an interval of >24 hours, one unprovoked seizure with a recurrence risk of >60% in the following ten years, and one seizure in the context of a diagnosable epilepsy syndrome. Relevant factors include previous, possibly misrecognized milder seizure types, prolonged seizures, focal tics, potentially epileptogenic lesions, and evidence of epileptic activity on EEG.
The right therapy for every patient
One of the major problems with monotherapy is the delayed approval of many antiepileptic drugs, even though they are already approved for combination therapy and are used in largely identical doses, the expert criticized. In this context, a clear superiority of monotherapeutics over placebo has been demonstrated since 2016 based on historical controls. In the meantime, fortunately, a selection of preparations for epilepsy treatment is nevertheless available. In order to select the appropriate therapeutic agent individually for each patient, criteria such as the epilepsy syndrome, intake and dosage, teratogenicity, mechanism of action, tolerability profile, and efficacy should be included in the considerations.
Old hat: generalized epilepsies
Unfortunately, the treatment of generalized epilepsies still shows a superiority of the old drugs, Schulze-Bonhage regretted. Several studies have shown that the new substances, such as valproate or ethosuximide, are more effective in preventing childhood absences in the long term than, for example, lamotrigine. Another study also demonstrated significantly greater efficacy in the treatment of generalized epilepsy for valproate and levetiracetam compared with lamotrigine. However, it has also been shown that the improved seizure freedom is associated with a higher risk of side effects. Accordingly, it should be weighed individually whether the use of a more potent preparation justifies the adverse effects that may occur, the expert noted. With regard to long-term retention, valproate showed significantly better results compared with topiramate and lamotrigine. Valproate was also clearly superior compared with levetiracetam. However, it should not be ignored that valproate carries by far the highest risk of malformations, the speaker emphasized. In addition, the cognitive risk on language and mathematical performance in children after intrauterine exposure has been known for some time.
Focal epilepsy treatment at current level.
When making treatment decisions regarding focal epilepsies, it has always been very difficult to show differences in the effectiveness of different preparations. Neither meta-analyses nor classic monotherapy study designs were able to detect relevant differences in efficacy. Only levetiracetam was shown to have better seizure control in long-term use for focal epilepsy in the elderly. Similar retention measures were also shown for lamotrigine compared with carbamazepine. Lamotrigine also scored well against levetiracetam and zonisamide in terms of best long-term retention.
Now there is a new player in the epilepsy treatment armamentarium in eslicarbazepine. This prodrug can be administered as a single dose and does not induce serum peaks. This significantly reduced the risk of side effects and improved tolerability accordingly. Over a 24-month period, administration of eslicarbazepine as monotherapy resulted in a high rate of seizure control of more than 65% in all patients, Schulze-Bonhage pointed out. Therapy-naïve patients respond even better to initial treatment with the new preparation. Responder rates of over 90% were observed over a 12-month period.
Individual patient profile
However, according to the expert, efficacy alone should not be the sole deciding factor for or against a therapy. Individually tailored to the patient’s needs, time to efficacy also plays a role. If an immediate effect is needed, levetiracetam, pregabalin, or brivaracetam may be used. The sodium channel blockers such as eslicarbazepine or oxcarbazepine take about a week to respond, and lamotrigine or zonisamide require significantly more time. Another important aspect is comorbidities in terms of psychiatric, cardiac, cognitive, or metabolic effects.
Effective monotherapy still state of the art
The expert summarized that monotherapies remain a good choice especially in early treatment phases of epilepsies. For generalized forms, valproate remains the most effective but not the best tolerated drug. Especially in young women, monotherapy with lamotrigine or levetiracetam should be tried beforehand. In focal epilepsies, the tolerability profile determines long-term adherence. Sodium channel blockers in particular are the focus of the best treatment options, but should be used with caution in the presence of preexisting cardiac disease.
Congress: FomF Neurology Update Refresher
InFo NEUROLOGY & PSYCHIATRY 2021; 19(3): 36-37 (published 6/4/21, ahead of print).