Wound healing disorders are often a symptom of an underlying disease and manifest clinically in different ways. In addition to treatment of the underlying disease, local wound treatment is the most important pillar of therapy. The MOIST concept describes the phases of wound healing. From the “Big Five” wound dressings available today, it is important to choose the treatment method that is best suited to the individual patient.
Acute wounds are usually due to trauma following cuts or abrasions and heal quickly. Chronic wounds are said to occur when wound closure fails to occur within 8 weeks [1]. The prevalence of chronic wounds is strongly age-dependent, which is due on the one hand to an age-correlated decrease in the biological regenerative capacity of the skin and on the other hand to the fact that wound healing disorders frequently occur as a symptom of age-associated underlying diseases (e.g. venous or arterial vascular diseases or diabetes mellitus) [2]. In about 90% of cases, vascular diseases are the cause of chronic ulcers, explains Dr. med. Kerstin Kusch from the Charité, Universitätsmedizin Berlin, on the occasion of her presentation at the FomF (D) Dermatology and Allergology [1]. More than half of these are venous leg ulcers, slightly less common are mixed leg ulcers, followed by arterial leg ulcers and diabetic foot syndrome. The remaining 10% are due to other causes: Infections (e.g., late syphilis, atypical mycobacteriosis, cutaneous leishmaniasis), underlying autoimmunologic diseases (e.g., pyoderma gangrenosum, bullous dermatoses), neoplastic changes (basal cell/ squamous cell carcinoma), or exogenous factors (drugs, contact allergies, burns).
ABCDE rule for the diagnosis of chronic wounds
In order to achieve sustainable therapeutic success, early diagnosis of the underlying causes is crucial. Care of the underlying disease based on this combined with adequate local treatment is important for wound closure. Detailed history and careful clinical inspection according to the ABCDE rule are key elements to clarify the etiology of wound healing disorders [1,2].
A – Medical history: A careful medical history should be taken as the first step in the diagnostic procedure. In addition to the current symptoms (pain, intermittent claudication) including intensity and duration of occurrence, this includes the investigation of possible underlying diseases, as well as a medication history and inquiries about relevant lifestyle factors (e.g. diet, nicotine, alcohol).
B – Bacteria: A common complication of chronic wounds is bacterial superinfection in the form of erysipelas or phlegmon. If there is evidence of infection, blood count, C-reactive protein, and erythrocyte sedimentation rate should be determined in addition to body temperature. Bacterial diagnostics can also exclude multi-resistant pathogens such as methicillin-resistant Staphylococcus aureus or multi-resistant Gram-negative pathogens. If osteomyelitis is suspected, clarification by imaging is recommended.
C – Clinical examination: In addition to the wound description including localization, size/depth, wound margin, wound environment, necroses, coatings and exudate, sensitivity testing, edema diagnosis, mobility in the ankle joint and assessment of malpositions are important elements of the clinical examination.
D – Circulation: The venous and arterial systems should be examined as part of vascular diagnostics. Arterial diagnostics of the lower extremities includes the determination of the ankle-brachial pressure index in addition to palpation of the foot pulses. Doppler sonography of the leg veins (possibly color-coded duplex sonography) is considered the basic diagnostic test for suspected cardiovascular insult.
E – Extras: If the basic diagnostic clarifications do not succeed in determining the causes of the wounds, a large number of further diagnostic procedures are available. A biopsy can be very informative. If diabetes mellitus, vesicular autoimmune dermatoses, vasculitis, lues, coagulopathy, or calciphylaxis are suspected, serologic analyses can be initiated. In addition, epicutaneous testing (allergic contact dermatitis), pathergy test (pyoderma gangraenosum, Behçet’s disease), capillary microscopy (collagenosis) and genetic analyses are used for etiological clarification.
“The Big Five” of wound dressings
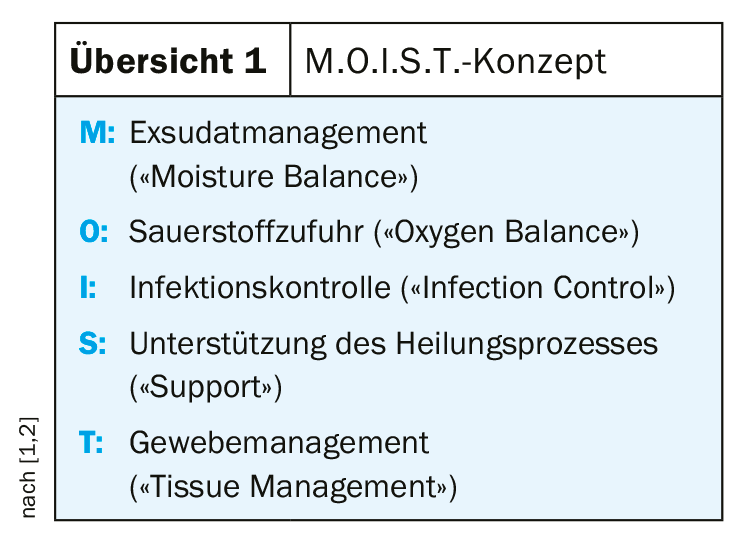
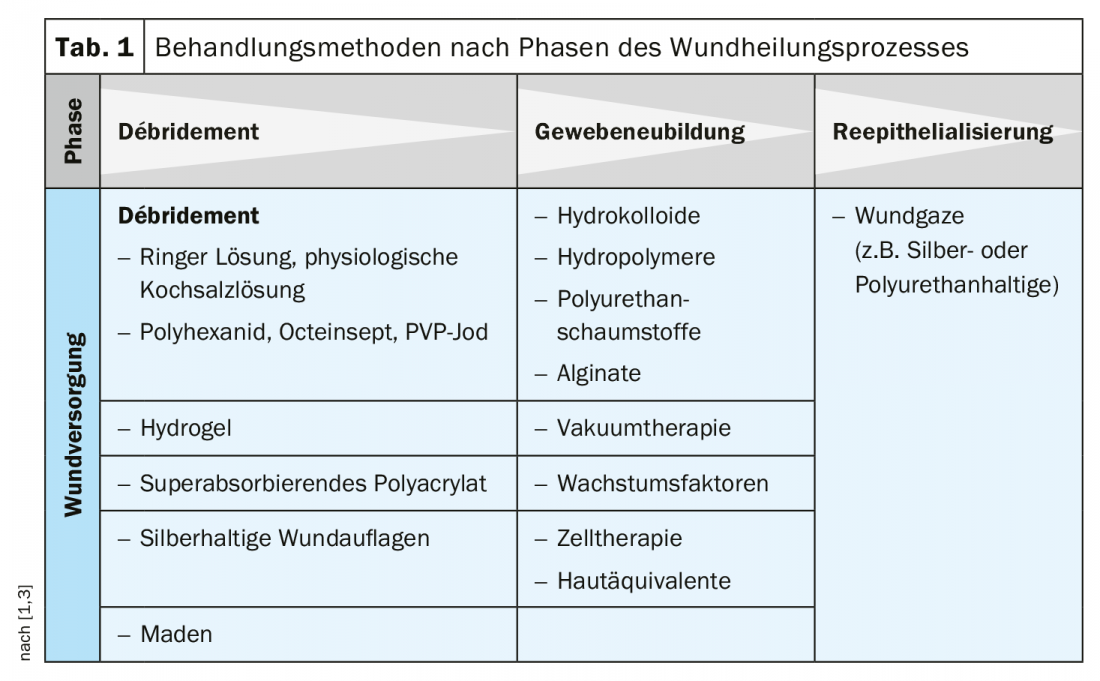
The use of the treatment methods currently available for local wound treatment is based on the clinical picture, taking into account the wound bed, the wound environment, the infection status and the amount of exudate, irrespective of the underlying disease. The M.O.I.S.T. concept described in Overview 1 serves as a guide for the use of various wound therapeutics (it is an evolution of the original T.I.M.E. concept) [1,2]. An important therapeutic goal is to transform the microenvironment of the chronic wound, characterized by persistent inflammation, into one that is conducive to the healing process. As part of a phase-adapted approach, wound cleansing and debridement are performed first, followed by stimulation of granulation tissue growth and promotion of epithelialization. A rough overview of which treatment method is appropriate in which phase of wound healing is given in table 1, whereby the choice of wound dressing must also be adapted in particular to specific features such as wound depth and individual characteristics (e.g. contact allergies) [3]. The multitude of wound dressings available today can be divided into the following five categories (“Big Five”) [1]:
I: Classic wound dressings: gauze/fleece dressings, absorbent dressings, superabsorbent dressings, impregnated wound gauze/wound contact dressings with silicone
II: Hydroactive dressings: alginates and aquafilaments, hydrogel dressings and gel, hydrocolloids, hydropolymers.
III: Interactive wound dressings: collagen wound dressings, gelatin-containing wound dressings, hyaluron-containing wound therapeutics
IV: Antibacterial and odor-binding wound dressings: activated charcoal dressings, hydrophobic wound dressings, antiseptic wound dressings, silver-containing wound dressings
V: Special wound dressings: maggot therapy, local negative pressure therapy
Although the spectrum of wound dressings is broad, the respective principles of action are similar. By absorbing the wound exudate, factors harmful to wound healing (e.g. bacteria, toxins, proteases) are eliminated, maceration of the wound environment is prevented and a moist wound environment is induced. In the case of products with heterogeneous mechanisms of action containing, for example, collagen, chitosan, hyaluronic acid, hemoglobin or growth factors, the aim is to actively influence factors in the wound environment that impede wound healing, such as matrix metalloproteases (MMP), pH, oxygen supply, reactive oxygen species (ROS), growth or coagulation factors. These wound dressings have proven themselves in the practical care of patients with chronic wounds and can contribute to an improved quality of life for patients.
Vacuum therapy is a method that has proven to be very effective, especially for stimulating tissue formation, and in recent years has become a standard procedure in the treatment of large-area as well as deep acute and chronic wounds [2]. In this technique, a polyvinyl alcohol or polyurethane sponge or, alternatively, a gauze dressing is inserted into the wound defect. Subsequently, an airtight film is applied and subatmospheric pressure is created, which stimulates the wound healing processes. In particular, this method proved to be very effective in the treatment of diabetic foot syndrome, decubitus ulcer and venous leg ulcer.
Compression therapy is an effective method used in the treatment of most chronic lower extremity wounds or edema. In addition to patients with venous leg ulcers, many other types of chronic wounds such as mixed leg ulcers, vasculitis, vasculopathy, or necrobiosis lipoidica can be treated with it after exclusion of relevant contraindications (critical ischemia) [2]. Due to the painfulness, the treatment should be started with a lower pressure. In the initial phase of decongestion, multicomponent systems are available for this purpose, as well as adaptive compression bandages in which pressure values can be specifically adjusted. Ulcer compression stockings should be fitted only after decongestion has been completed in the maintenance phase.
With regard to future prospects for the further development of wound treatment methods, research is concerned, among other things, with the question of whether better effects can be achieved through combinations of several therapeutic modalities with different active principles, such as growth factors, cells and skin equivalents, than when used as monotherapy, and in what form corresponding therapeutic strategies could be used.
Source: FomF (D) Dermatology and Allergology 2020
Literature:
- Kusch K: Modern management of chronic wounds. Kerstin Kusch, MD, Dermatology and Allergology Refresher, FomF.de, Hofheim (D), Sept. 10, 2020.
- Eming SA, Dissemond J: Wound therapy. In: Plewig G et al. (Eds). Brown-Falco’s Dermatology, Venereology and Allergology. Springer Reference Medicine 2017.
- Dabiri G, Damstetter E, Phillips T: Adv Wound Care (New Rochelle) 2016; 5(1): 32-41.
DERMATOLOGIE PRAXIS 2020; 30(5): 48-50 (published 12/10/20, ahead of print).