The most important success factors for successful rehabilitation in COPD patients include motivation for self-management, smoking cessation, weight reduction, and exercise promotion (strength building). The motivational interview and patient education are promising concepts for this.
Pulmonary rehabilitation aims to optimize the physical capacity limited by COPD, bronchial asthma or emphysema, using a combination of methods suitable for this purpose. Rehabilitation includes all measures that improve the disease and its consequences. Often, COPD patients are overwhelmed by the complexity of their disease or show little confidence in managing it. Carrying out the therapy, adjusting it if necessary, and organizing adequate medical help at the right time and using available resources is important.
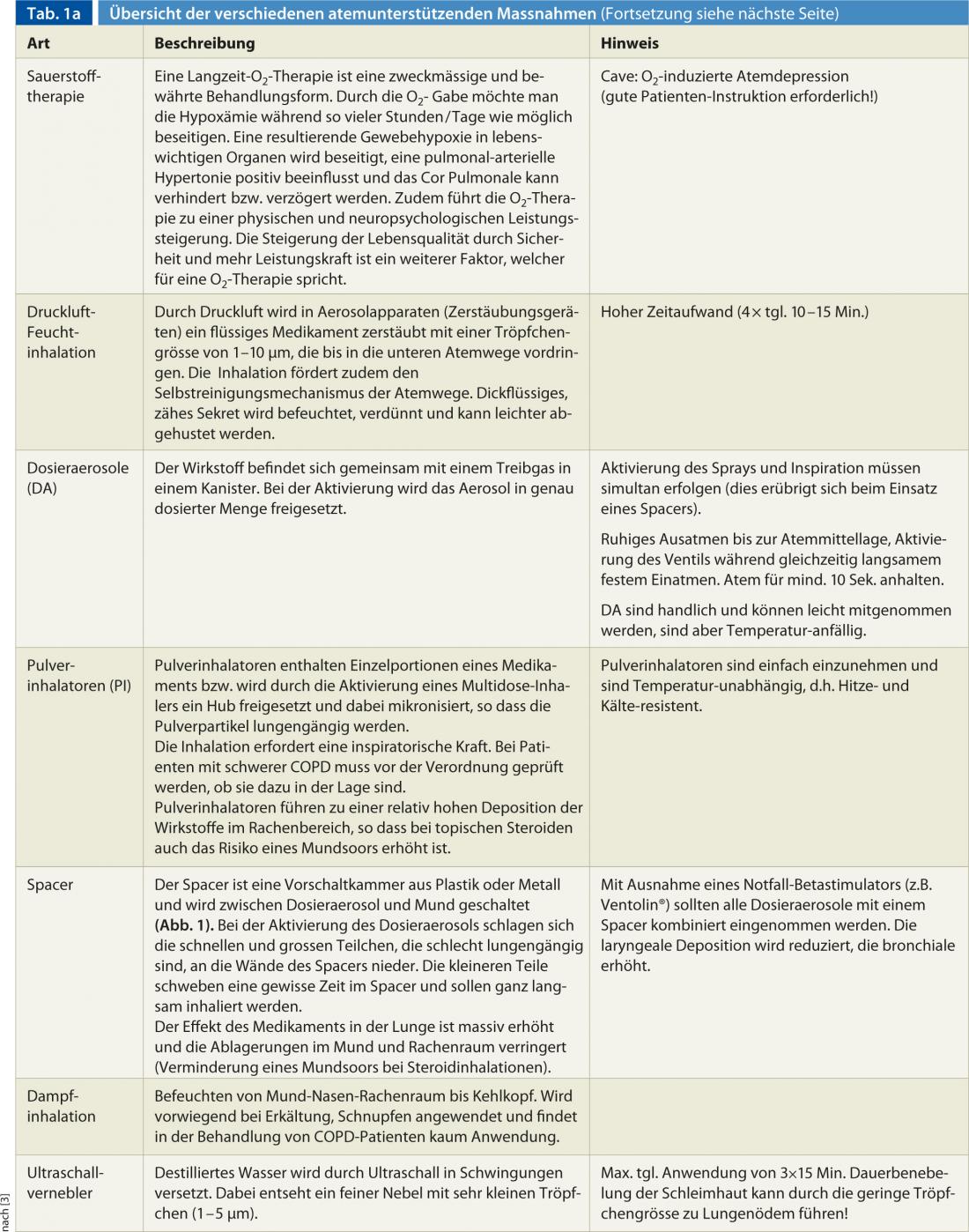
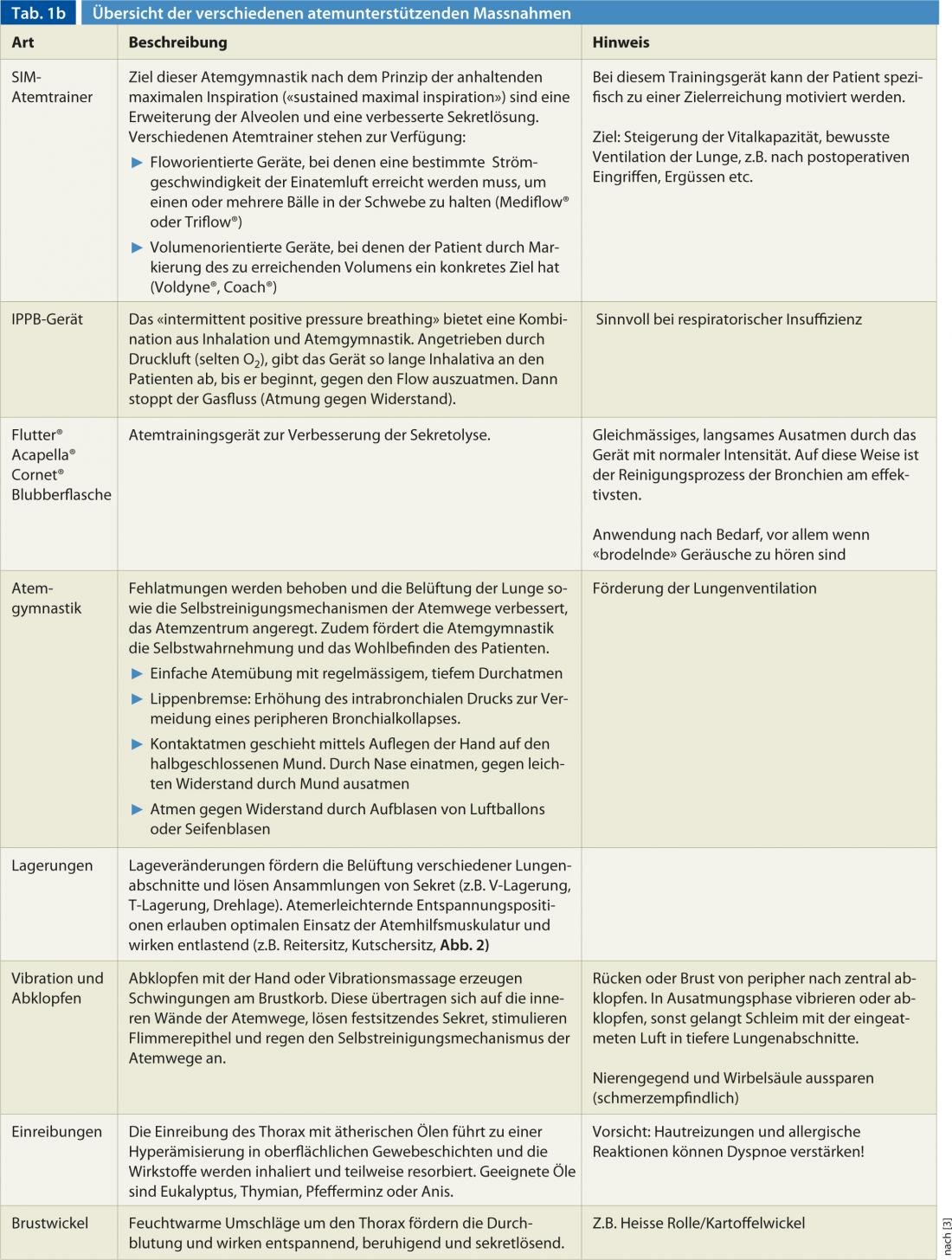
Another important pillar of treatment for COPD is patient education. Those affected should learn methods so that they can cope with their illness more easily. Rehabilitation is helping people to help themselves [1]. The following article points out the key points of self-management promotion and motivational interviewing. The tabular overview highlights the breath support interventions and describes the main application and instructional focus (Tab. 1).
Targeted patient education and self-management encouragement promote confidence to manage dyspnea and any exacerbation [2]. Quality of life and treatment efficacy can be greatly enhanced by rehabilitation and have a positive impact on psychophysical resilience and the extent of dyspnea at a given level of exertion [3]. The effects of endurance and strength training as well as respiratory muscle training have been proven (see article Silvio Catuogno/Sandra Brülisauer).
Therefore, motivation for self-management and patient education regarding proper inhalation and inhalation technique, adherence to an exercise plan/rhythm, smoking cessation, weight reduction, and promotion of problem-solving skills are among the main goals during rehabilitation.
The social reintegration of patients is also important. Often, lung patients become severely isolated due to their physical limitations. Experience groups or the cantonal lung leagues can be helpful in this regard and can help the affected person to talk about his or her problems and to find a way out of isolation.
Promotion of self-management skills
One of the most important intervention principles for the chronically ill is encouragement to self-manage. The independence, the active role of the affected person and the motivation of self-responsibility are the key to successful therapy and the achievement of the rehabilitation goal in people suffering from COPD [4]. Self-management education for COPD patients may lead to a reduction in hospital admissions [2]. Self-management interventions are primarily aimed at competence development, with a focus on “skills training.”
The literature points out that self-management support must be problem-oriented. Teaching problem-solving skills is critical [5]. Chronically ill people usually already bring a great deal of individual experience with them. They have experienced their symptoms in a very personal way, developed strategies, and experienced the impact on everyday life. These experiences and the individual’s symptom management theories are important information for the caregiver so that he or she can respond to the patient individually in an empathic manner [6]. Problem-solving competence according to Haselbeck and Schaeffer 2007 comprises different abilities and skills [5]:
The competence to be able to recognize, define and assess problems: Problems must be identified and addressed in a timely manner to avoid problem compounding. This requires good self-awareness and accurate self-observation skills, as well as the ability to interpret, assess problems, and develop and implement solutions (e.g., perceive signs of exacerbation in COPD and assess the dangers).
The ability to make viable decisions: Changing patient roles and advances in medical technology have increased the diversity of decisions for those with the disease in recent years. On the one hand, this means an opportunity, but on the other hand, it also means a risk of overload. Strengthening decision-making is therefore an important component in promoting self-management or problem-solving skills (e.g., making the decision to seek emergency medical attention in the event of fever and increased dyspnea).
The ability to use resources: This includes, among other things, identifying one’s own resources as well as those of others, checking them for their viability, and deploying and using them in a targeted manner. This enables crises, problems and challenges to be tackled and overcome by the company itself.
The ability to establish and maintain viable relationships with professional stakeholders: Holding professional support in line with needs and requirements means having close and resilient relationships with the relevant professional actors. In addition, specific communication and interaction skills are needed to ensure that ideas about the patient role reach the respective health care professionals. Contacts must also be established with informal helpers, because they play an essential role, especially in the case of chronic illnesses.
The ability to plan one’s own actions and implement them in line with goals: It is about setting goals for action and plans on the basis of decisions made by oneself and translating them into concrete actions. To this end, solutions to problems proposed by the professional actors must be tailored to the individual situation and the everyday demands faced by the person with the disease. Once the implementation is done, it is necessary to evaluate it in order to see if it has led to the desired goal and if the result has been solved satisfactorily.
In conclusion, self-management support with its focus on patient autonomy and activation is a promising and important concept that is already highly relevant internationally for supporting coping with chronic illness and will become even more important in the future. The recognition that the patient’s autonomy must be preserved and that the patient must be seen as a co-producer of his or her health allows therapies and treatments to become more effective and efficient. Pathways that lead to partnership with the patient are among the most important components of care for the chronically ill [5].
Motivational interviewing
Motivational interviewing was originally developed for people with addiction problems. Today, this approach is used in many counseling sessions in the psychosocial setting. What is important here is not primarily the technique, but the respectful and open basic attitude. It is an emancipatory consulting concept. Patients set the pace and direction of the conversation. This promotes patient ownership. He becomes the expert of his awareness and change process. The counselor is only a companion and acts in a directive way, actively supporting the patient in detecting, exploring and, if possible, resolving his ambivalences. Attempts at persuasion on the part of the consultant have proven ineffective in practice [7].
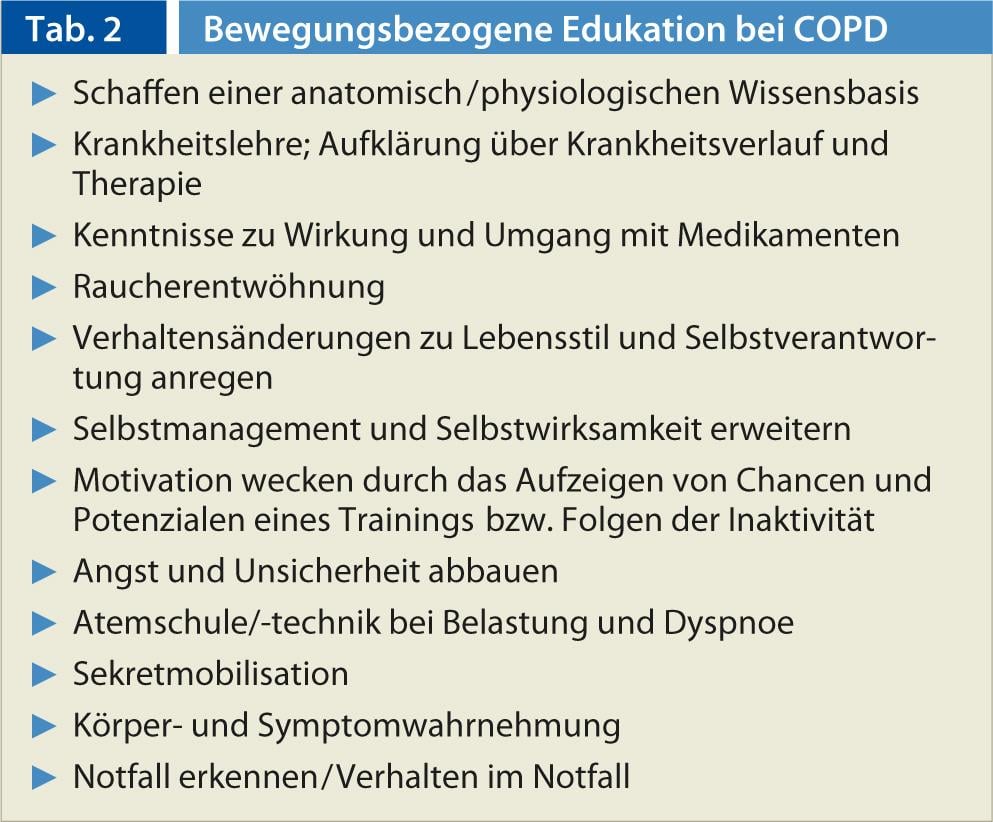
For Miller and Rollnick 2009, Prochaska and Di Clemente’s transtheoretical model (TTM) is central. In the TTM, the stages of motivation to change are described. It is important to recognize at what stage of the change process the patient is. Depending on the stage, the authors suggest different strategies of the consultant. Resistance arises primarily when the counselor’s strategy does not match the patient’s stage of change. Table 2 summarizes the five principles of motivational interviewing.
Breathing support measures
If drug therapy for COPD is used orally or systemically, this has side effects on other organs. Steroids are administered perorally preferably to treat an exacerbation, at the beginning of steroid therapy, or when topical steroids are not effective enough. Other drugs that are usually administered perorally include antibiotics and theophyllines.
Correct instruction and subsequent control of oxygen handling are indispensable components of therapy, as are instructions on the various inhalatives, breathing exercises, chest compresses, positioning in case of respiratory distress, rubs and secretolytic measures. Table 3 summarizes the most important points to remember for inhalation instruction.
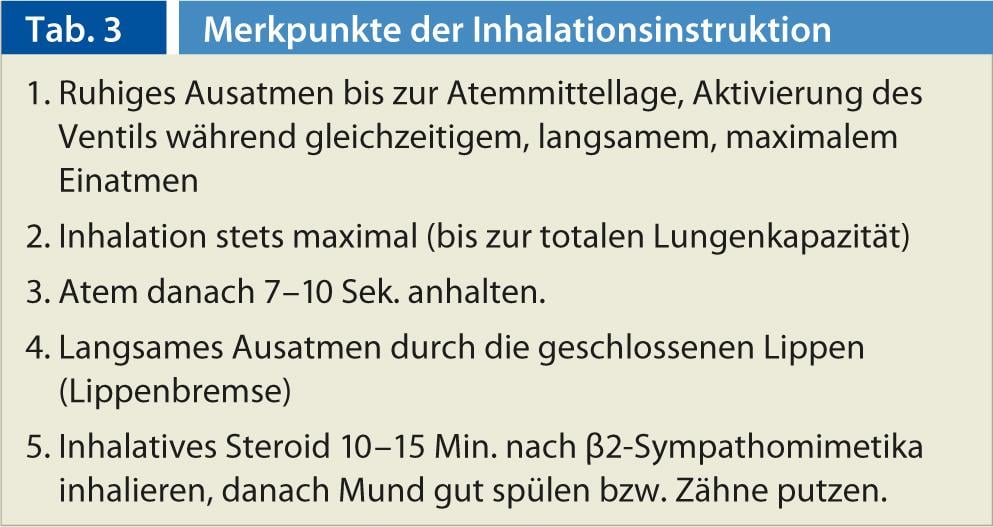
Figure 1 shows the spacer in use. Figure 2 shows possible postures that facilitate breathing.


Fig. 1: Spacer (upstream chamber for increasing the effectiveness of the metered dose inhalers)
Fig. 2: Coachman’s seat and rider’s seat are breath-supporting sitting positions and help with relaxation.
CONCLUSION FOR PRACTICE
Effective rehabilitation includes the following measures:
- Motivation for self-management
- Patient and family education
- Motivational interview (smoking cessation, weight loss)
- Diagnostics for reassessment and visibility of performance improvement
- Medication optimization
- Specific muscle building training
- (cf. article Catuogno/Brülisauer in this issue).
- Nutritional counseling
- Psychosocial counseling/support
Nadja Wyrsch
Literature:
- Steuer-Stey C: Therapeutic patient education and self-management: a guide for the project Living with a Long-Term Illness “LEILA” of the Municipal Health Services of the City of Zurich. University of Zurich: Zurich 2010.
- Effing T, et al: Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2003 2007; 1. CD002990; PMID: 12535447.
- Schäffler A, Menche N: Internal Medicine. (3rd ed.). Stuttgart: Fischer 2008.
- Holman H, Lorig K: Patient self-management: a key of effectiveness and efficiency in care of chronic disease. Public Health Report 2004; 119(3): 239-243.
- Haselbeck JW, Schaeffer D: Self-management support in chronic illness. Nursing 2007; 2(7): 82-92.
- Baeriswyl C, et al: Symptom management: a nursing theory and its application: Focusing on the patient experience. Nursing 2013; 3(13): 8-11.
- Miller R, Rollnick S: Motivational interviewing (3rd ed.). Freiburg: Lambertus 2009.
- Kerstjens H, et al: Bronchitis, chronic obstructive pulmonary disease (COPD). Bern: Huber 2007.
- Lungenliga Schweiz: Basic knowledge about lung and respiratory diseases. Bern: Swiss Lung League 2010.
- McIvor A, Little P: Chronic obstructive pulmonary disease. Praxis 2008; 97: 1247-1248.
- Wittmann M, et al: Patient Education in COPD During Inpatient Rehabilitation Improves Quality of Life and Morbidity. Pulmonology 2007; 61(10): 636-642.











