As a basis for a differentiated diagnosis and treatment, a careful medical history is crucial. Tension headaches account for over 90% of all primary headache symptoms. Lifestyle measures are an important cornerstone of therapy and can be combined with pain-relieving medications for acute treatment or as prophylaxis.
With a 1-year prevalence of about 60% in adults and over 70% in adolescents, headache is one of the two most common health complaints, along with nonspecific back pain [1]. 20% of all sickness-related work absences are due to headaches [2]. According to the International Headache Society, there are 200 different types of headache, distinguishing between primary and secondary forms. More than 90% of cases are primary headaches, most commonly tension-type headaches, followed by migraine headaches (Fig. 1) [2].

Headaches affect the quality of life of those affected
If headaches occur regularly, they can lead not only to consequential health economic costs but also to a considerable reduction in the quality of life. Tension headaches and migraines are most common between the ages of 20 and 60 . Contemporary headache treatment is multimodal. The inclusion of lifestyle measures is particularly important in tension type.
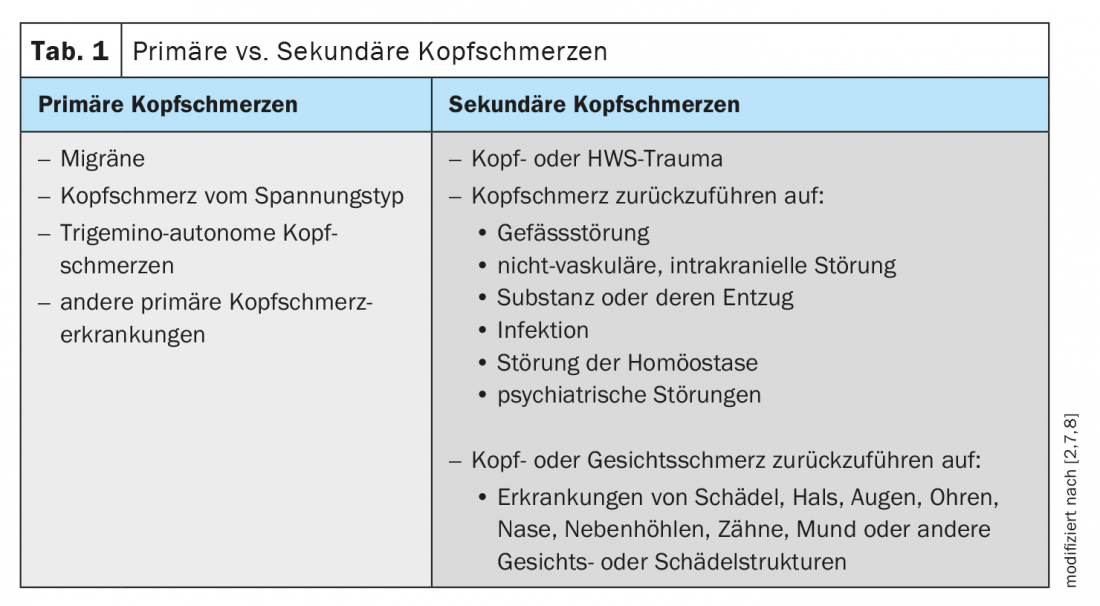
Table 1 lists possible causes of secondary headache, which in terms of frequency distribution account for less than 10%, but should still be considered in the diagnostic workup [2]. The complaints of patients with headaches should be taken seriously; it is a distressing symptom for those affected, regardless of the cause.
Is it a migraine or tension headache?
More than half of the primary headaches presented to the general practitioner are of the tension type. Especially the chronic form of the disease is frequently associated with stress, depression and anxiety disorders. Pathophysiologically, tension headache is thought to involve increased sensitivity of peripheral myofascial nociceptors and increased sensitivity of central pain processing pathways [3]. The Swiss Headache Society recommends the criteria of the International Headache Society [4] for diagnosis.
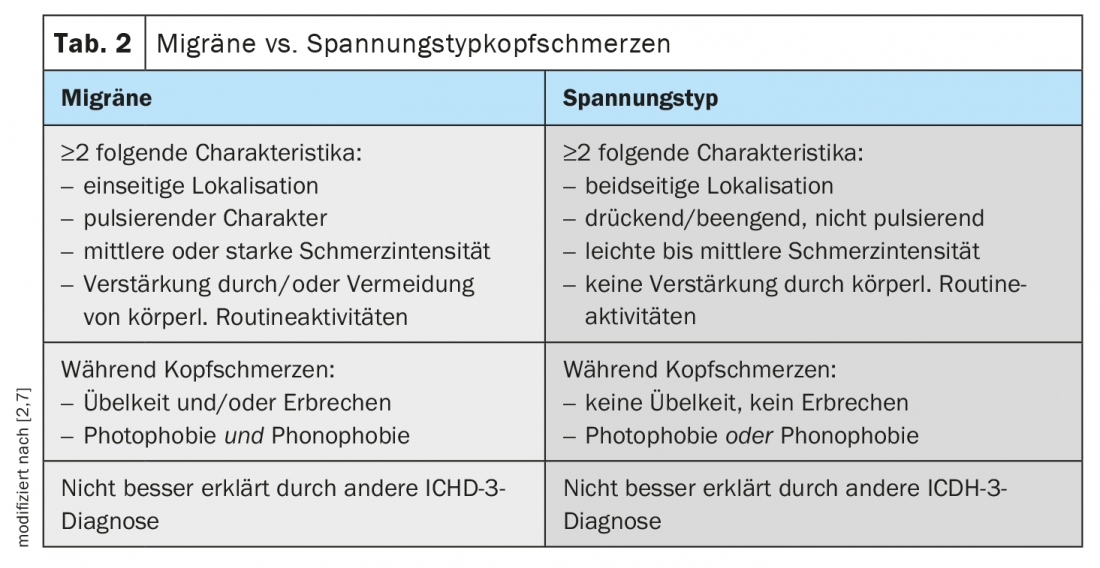
At the initial consultation, one anamnestic difficulty may be that patients cannot accurately describe the nature of their symptoms. Therefore, it is important to educate the patient and revisit this in a subsequent consultation to make a classification. In contrast to tension headaches, migraine often has a prodromal phase that can last up to two days and is associated with accompanying symptoms such as light sensitivity and nausea (Table 2) [2]. Tension headache, unlike migraine, is characterized by bilateral, non-pulsating pain that is not aggravated by routine physical activities. It must be clarified whether one of the following causes is behind the tension headache: teeth grinding, presbyopia (presbyopia), sinusitis.
Individual treatment plan
Tension headache occupies a special place in pain management because of its high prevalence. Chronic primary headaches in particular lead to a significant impairment of the quality of life in those affected. An important treatment goal is reintegration into everyday life and improvement of quality of life. Patient education and information play an important role in this. It is advisable to draw up a treatment plan together with the patient, taking into account individual aspects including suffering and fears. It is important to mobilize the patient’s resources to reduce suffering.
Lifestyle factors play an important role
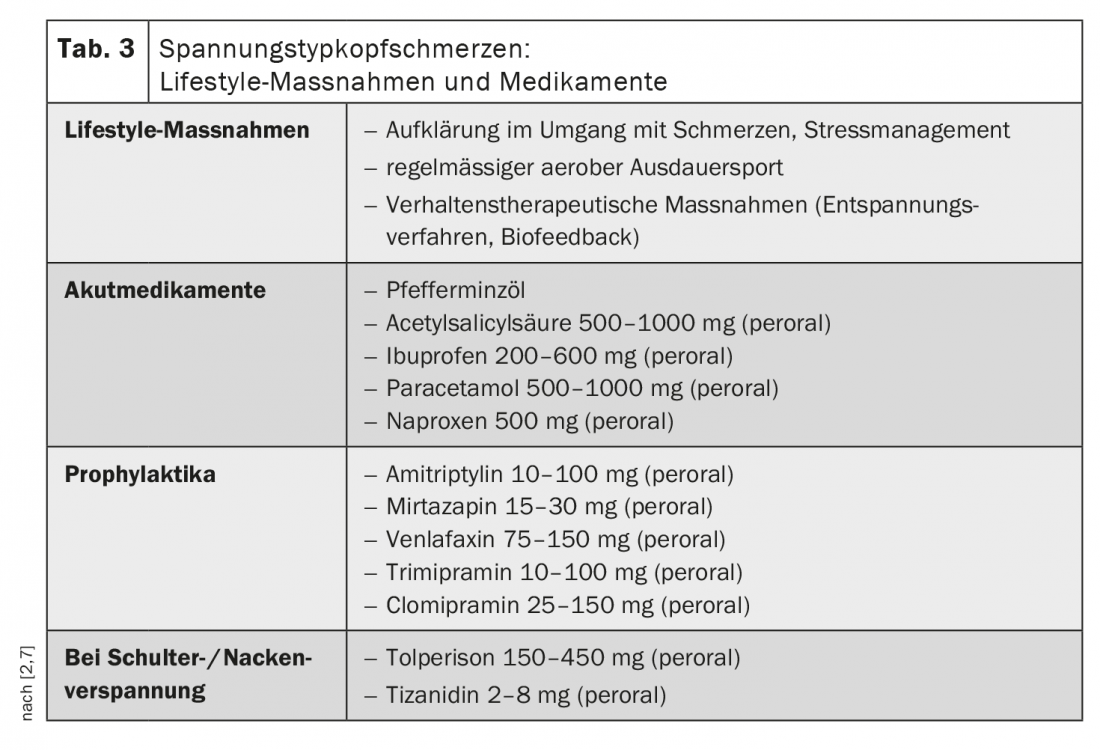
The inclusion of lifestyle measures is central to the treatment of tension headaches. This includes promoting a balanced and healthy lifestyle. Care should be taken to maintain a good balance of activity and relaxation. Stress reduction and regular physical exercise, preferably in the fresh air, are recommended. Endurance sports are helpful in relieving stress. Furthermore, measures to tone the autonomic nervous system, such as alternating showers, can have a positive effect [9]. A balanced diet and sufficient sleep are other important factors.
Medications recommended for acute treatment and prophylaxis
For tension headaches, a distinction is made between treatment of headache attacks and prophylactic measures. In episodic tension headache, the duration of symptoms is usually limited to half an hour to a few days; usually the headache subsides after 1 to 2 hours. Chronic tension headaches are said to occur when the headaches occur monthly for more than 15 days.
Medications that are helpful for acute tension headaches include, for example, acetylsalicylic acid, ibuprofen, acetaminophen, or naproxen (Table 3) [2]. It should be noted that pain medications are used at a maximum of 10 days per month in adequate doses to avoid chronicity of the headache problem due to medication overuse. The use of medications should be combined with lifestyle measures. If the headache is infrequent and can be well controlled, there is no need for prophylactic medication. For chronic headache, amitriptyline, mirtazapine, venlafaxine, trimipramine, or clomipramine are recommended as prophylactic pharmacotherapy (Table 3).
How to recognize and avoid rebound effects
Headaches from excessive medication use affect men more often than women [10]. The exact causes of this rebound phenomenon have hardly been clarified so far. Genetic factors are thought to play a role. It is thought that sufferers have a hypersensitive nervous system, so that the nerve cells in the brain that trigger pain are stimulated too quickly. Headache due to excessive medication use is diagnosed when all of the following criteria are true [10]: the headaches occur on more than 15 days per month, the sufferers have been regularly taking too much or too many medications to relieve their headaches for more than 3 months, and the symptoms cannot be better explained by any other headache disorder. How many days per month constitute excessive medication use also depends on the active ingredient. The literature indicates 10-15 days per month. Patients should be educated about this. To treat withdrawal symptoms that may occur after discontinuation, prescribing a different type of headache medication is recommended. Sufferers should be instructed to stop using previously overused medications or to use headache medications for a maximum of 10 days per month. Advice regarding healthy lifestyle habits is also important [10].
New guideline planned for 2021
Last year, the German Migraine and Headache Society launched a headache registry to improve clinical care for headache sufferers [5]. And later this year, the new edition of the guideline on the therapy of episodic and chronic tension-type headache is planned to be published under the auspices of the German Neurological Society (DGN) and the German Migraine and Headache Society (DMKG) [6].
Literature:
- Straube A, et al: Period prevalence of self-reported headache in the general population in Germany from 1995-2005 and 2009: results from annual nationwide population-based cross-sectional surveys. J Headache Pain 2013; 14: 11.
- Palla A: Headache: diagnosis and therapy. PD Antonella Palla, MD. Forum for Continuing Medical Education 23.6.2020.
- Brüne B, Erni S, Huber F, Beise U: Headache. Guideline, Last revised: 11/2018 Last modified: 11/2018, www.medix.ch (last accessed 03/15/2021).
- Swiss Headache Society: Treatment recommendations for primary headache, 10th fully revised edition 2019, https://headache.ch, (last accessed Mar. 15, 2021).
- “DMKG Headache Registry Launched,” www.aerzteblatt.de/nachrichten/115198/DMKG-Kopfschmerzregister-gestartet (last accessed Mar. 15, 2021).
- AWMF: Registered guideline project, www.awmf.org/leitlinien/detail/anmeldung/1/ll/030-077.html, (last accessed 03/15/2021).
- Swiss Concussion Center, https://swissconcussion.com (last accessed Mar. 15, 2021).
- International Headache Society (IHS): “International Classification of Headache Disorders,”3rd edition, ICHD-3, https://ihs-headache.org/en (last accessed Mar. 15, 2021).
- Neurologicum Lake Zurich, https://neurologicum.ch/diagnostik/kopfschmerzen-migraene (last accessed Mar. 17, 2021).
- Silberstein S: Headache due to excessive medication use, MSD Manual, www.msdmanuals.com/, (last accessed 03/17/2021).
HAUSARZT PRAXIS 2021; 16(4): 26-27
InFo NEUROLOGY & PSYCHIATRY 2021; 19(5): 27 (abridged version).
InFo PAIN & GERIATry 2021; 3(2): 28