Nail fungus is not only a cosmetic problem, but an infectious disease that is contagious and can spread. From grandfather to grandchild, from foot to head. Onychomycosis should therefore be treated – using the three-step therapy, which is easy to perform, well tolerated and successful in family practice.
Nail fungus is an old disease. As early as 1854, Georg Meissner, a medical student in Göttingen, succeeded in “discovering the fungal cause of the disease”. Rudolf Virchow called it “onychomycosis”. The genius of this term is that under it can be included all the pathogens in question: Dermatophytes, yeasts and molds.
Masterful was his description of the clinical picture:
“Very clearly it appeared that the fungus had penetrated the edges from the front and then pushed itself both toward the center and backward deeper and deeper into the crevices of the horn formations, so that finally, at the very back, at the edge of the lunula, the large nest was formed. All the yellow spots were full of fungi, and in the crevices lay dense piles of spores. The yellowish-gray mass was so abundant that when the nail leaf was bent back and then allowed to spring back to its former position, a fine dust rose.”
What Virchow could not have foreseen was the spread of onychomycosis to a widespread disease and that it would be possible to cure it. From the age of 65, about one in two people suffers from it today. Children are also affected, which was unthinkable years ago. Nail fungus has developed into a family disease and for this reason is also one of the most important areas of therapy for the general practitioner.
The most common source of infection is parents or grandparents (Fig. 1). They not only transfer the genetic disposition, the receptors for the docking of fungi on the skin. If not treated, they also pass on the pathogen, the specific cause infection. The transmission is important. Because without fungus infection does not develop, regardless of the accompanying circumstances, which also play a role: damp skin, plastic shoes, circulatory disorders, smoking, sports.

Fig. 1: Onychomycosis in grandmother and granddaughter. The substance affected by the fungus must be removed. Pathogen: T. rubrum.
Therapy supplies
The necessity of the therapy results from the character of the infection. Although it is not threatening and can not penetrate inside the body, because skin fungi can thrive very slowly and optimally only at relative cold of 25-28 ° C.. You love cold feet!
However, the infection can spread on the skin, from nail to nail, to the groin, over the hands, and up to the face. In addition, there is the pressure of suffering. Many patients feel unattractive, no longer go to the swimming pool and exclude themselves.
A study by Szepietowski and Reich found the same level of stigma in patients with nail fungus as in those with psoriasis. The good news is that the level of suffering in the nail fungus group dropped to 40% of baseline just six months after starting therapy.
Thus, onychomycosis is a grateful disease, because it is curable. Because it has a specific cause, a pathogen that can and must be eliminated. The prerequisites for success are that the diagnosis is correct and the therapy corresponds to the clinical degree of infestation.
Clinic and diagnosis
Onychomycosis is usually a simple eye diagnosis. The nail affected by the fungus is either thick (Fig. 1) or atrophically destroyed (Fig. 3). Individual nails resist the disease, which is very characteristic of fungal infections. Unlike psoriasis, drug side effects or nail poisoning from formalin, which may be present in cosmetic nail polishes. In this case, several nails are almost always affected equally. If there is doubt about the clinical diagnosis, a sample should be taken. Even when systemic therapy is necessary. For this purpose it is sufficient, without prior disinfection, to cut as many fine shavings as possible from the affected nails onto a sheet of paper, fold it up and send it to a laboratory by normal letter.

Fig. 3: 8-year-old boy with onychomycosis before and after systemic therapy with fluconazole 150 mg, days 1-3 daily, then 150 mg per week. Pathogen: T. rubrum.
Therapy
The key to success lies in the interaction of external and internal therapies. Treatment is carried out in two or three steps, depending on the extent of the disease. If the nail is thickened (type 1 infection), the infected nail mass must be removed (Fig. 1). This is not necessary for a nail already decomposed by the fungus (type 2 infection) (Fig. 3).
First step: removing the infected nail mass
The first step is the most important. The nail affected by the fungus should be removed. Removal is necessary because no internal drug is able to reach all pathogens from the inside. Yellow nests often remain after tablet therapy, the dreaded “yellow streaks” that are the leading cause of relapse.
To eliminate the fungal nail material, several options can be considered:
- Laser
- Milling
- Treatment with 40 percent urea.
The latter is the only method that can be done with high efficiency, painless and without trauma by the patient himself, usually over two weeks until the diseased nail is completely removed. If necessary, it can be repeated as often as necessary.
The resounding power and effect of urea is shown in Figure 2. The fungus-containing part of the nail is removed like a scalpel. The unaffected parts remain healthy like a curb. Pain does not occur in the process. A protective nail layer is preserved and the surrounding skin also shows no side effects.
The over-the-counter 40 percent urea preparations contain either urea (Onyster®) or urea and the addition of bifonazole (Canesten® Extra Nail Set). It has a broad spectrum of activity against all relevant pathogens, making the nail material detached from the urea no longer infectious. The urea also acts as a means of transport and takes the bifonazole to the nail bed, which can also develop its effect there.
Compared to urea medication, it is an illusion to believe that if you apply an acrylic varnish such as Loceryl® or Batrafen® to the thickened nail 1x per week, the active ingredients contained therein will reach the nail bed and the nail will heal as a result. Filing the nail before such lacquer therapy is also a concern, as the filed nail shavings are infectious and a serious source of infection. Apart from the small effect of this measure. Heavily thickened nails can alternatively be milled off sterilely by a podiatrist to a tolerable degree and then further treated with urea.
Equally critical is treatment with lasers such as the 3 step, Pinpoint or Cool Breeze, which do not ablate the nail, but only shine through it and heat it to 60 °C. This should cause the fungi to die or evaporate. This is not very credible, since the spores of the pathogens can survive up to 80 °C and do not contain water. The treatment is also expensive. Only lasers that ablate the nail (Erbium Yag laser) are effective. However, unlike urea therapy, this treatment is painful, also expensive and associated with side effects. There is a risk of nail bed destruction. A conduction anesthesia must be administered prior to treatment.
Surgical nail extraction is no longer in keeping with the times. It is painful and creates trauma where it is uncertain whether the nail will regrow or penetrate the tissue, which may result in further surgery and scarring of the nail bed.
Second step: Topical antifungals
The “nail wound” exposed by the urea, or the nail already primarily decomposed by the fungus (type 2 infection), must be consistently treated with topical antifungals. Urea-free preparations containing bifonazole (Canesten® Extra spray or cream) are suitable for this purpose. Unlike creams containing terbinafine (Lamisil®), these also have a protective antibacterial and anti-inflammatory effect. A major advantage of bifonazole is its unlimited approval in children and pregnant women.
With varnish against the nail fungus
Another option is daily therapy with Ciclopoli® against nail fungus. It is a liquid and water-soluble varnish containing ciclopirox. This substance has a sporocidal effect, which ensures that recurrences cannot occur, originating from fungal spores remaining in the nail tissue. Ciclopoli, in contrast to the classic acrylic lacquers, which are firmly brushed onto the nail surface, has a special transport system, which allows the active substance to penetrate even into deeper nail layers. It is advisable to continue local therapy until the nail has grown out clinically completely healthy. The sporocidal varnish should continue to be applied prophylactically for some time after the end of the internal therapy (Fig. 4).

Fig. 4: 35-year-old with onychomycosis before and after systemic therapy with terbinafine 250 mg, day 1-14 daily, then 250 mg per week. Pathogen: T. rubrum. Further prophylactic therapy with Ciclopoli varnish.
Shoes treatment
Recurrence prophylaxis also includes disinfection of footwear, as the fungal spores contained there can survive for longer than six months.
Third step: Systemic therapy
Internal therapy is added to local treatment when a nail is affected more than 50% or more than three nails are affected at the same time. It should always be based on a thorough local treatment, since the healing successes are rather modest with a rate of 40-70% with tablet administration alone.
Topical therapy compensates for this deficit and is thus the basic building block of any onychomycosis therapy. In many cases, only both forms of therapy in combination enable a healing success. If individual nails are slightly affected, local treatment is usually sufficient.
Table 1 contains the dosage information and indications for use of the systemic preparations. Fluconazole (e.g. Diflucan®) should be used in children due to excellent tolerability and terbinafine (e.g. Lamisil®) in the elderly due to lack of interactions. The value of itraconazole lies in the therapy of specific pathogens such as S. brevicaulis.
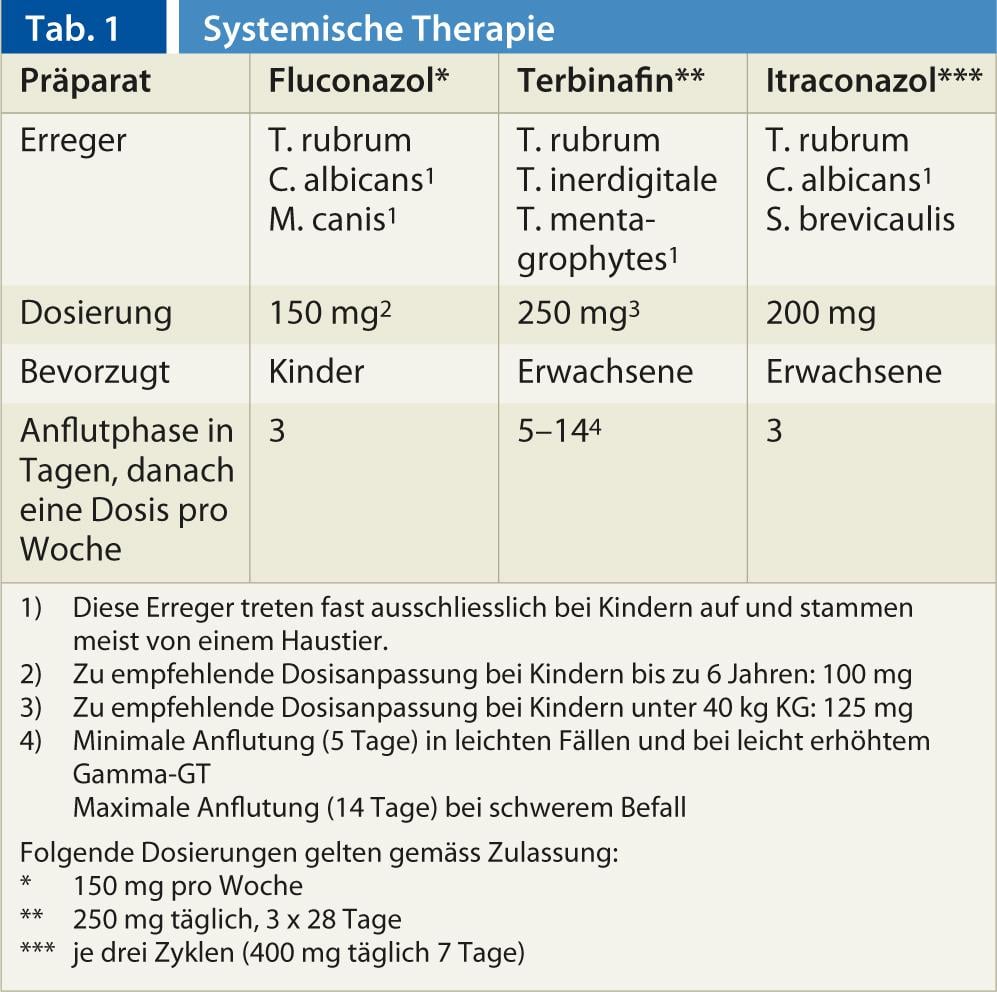
The efficacy gaps for each drug listed in the table are a reason to determine the causative agent prior to therapy. In children, no therapy should be carried out without determining the pathogen, as children’s nails can also be infected by germs originating from pets. In adults, empiric therapy with terbinafine may be used, since M. canis and C. albicans occur relatively rarely here.
New therapy options
A significant innovation in onychomycosis therapy is low-dose long-term treatment with a dose of 250 mg of terbinafine per week until clinical cure, in combination with local therapy. It differs fundamentally from the approved and guideline-recommended therapy of 250 mg of terbinafine daily for three months.
In view of the high efficacy of terbinafine, for Trichophyton rubrum already 0.001 µg/ml are lethal, such a high-dose therapy is no longer appropriate and furthermore much too short, since after three months no completely infected nail has grown back. This takes at least one year. After a short daily flare-up phase, in children it is only three days, it is sufficient to take the systemic antifungals only once a week thereafter, while continuing the topical therapy until the nail has grown out healthily.
Such therapy is virtually free of side effects, patient-friendly and economical. The success of the synergy of local and internal therapy is shown by the healing processes on Figures 3 and 4. A side effect of internal therapy is the rapid healing of the frequently affected skin of the feet, interdigital spaces or hands (Fig. 5).

Fig. 5: The same patient as in Fig. 4. healing of the skin under therapy with terbinafine two weeks after the start of therapy.
This proves that foot and nail fungus belong together, are caused by the same pathogens, are two stages of the same disease, and nail fungus is almost always the result of inadequately treated foot mycosis. Also due to the diverse spectrum of pathogens, tinea pedis should also be treated with creams containing substances with broad-spectrum activity: Bifonazole and Ciclopirox. This should be done thoroughly over two to three weeks so that foot fungus does not turn into nail fungus.
CONCLUSION FOR PRACTICE
- The interplay of external and internal therapies is necessary for healing. The pathogen is thus attacked and eliminated from the inside and outside.
- Decisive for the healing success are the correct diagnosis, the cooperation of the patient and the consistent two-sided therapy until the nail has grown out also visually healthy. In this way, any onychomycosis is permanently curable.
Prof. Dr. med. Hans-Jürgen Tietz
Possible conflicts of interest: none
HAUSARZT PRAXIS 2013; 8(3): 29-33











