The AACR Annual Meeting is where the cancer research community comes together to explore and push the boundaries of science in search of the next breakthroughs in cancer treatment. This has been achieved again this year in an impressive manner. With new treatment approaches in the field of lymphomas and solid tumors, two particularly promising options were singled out.
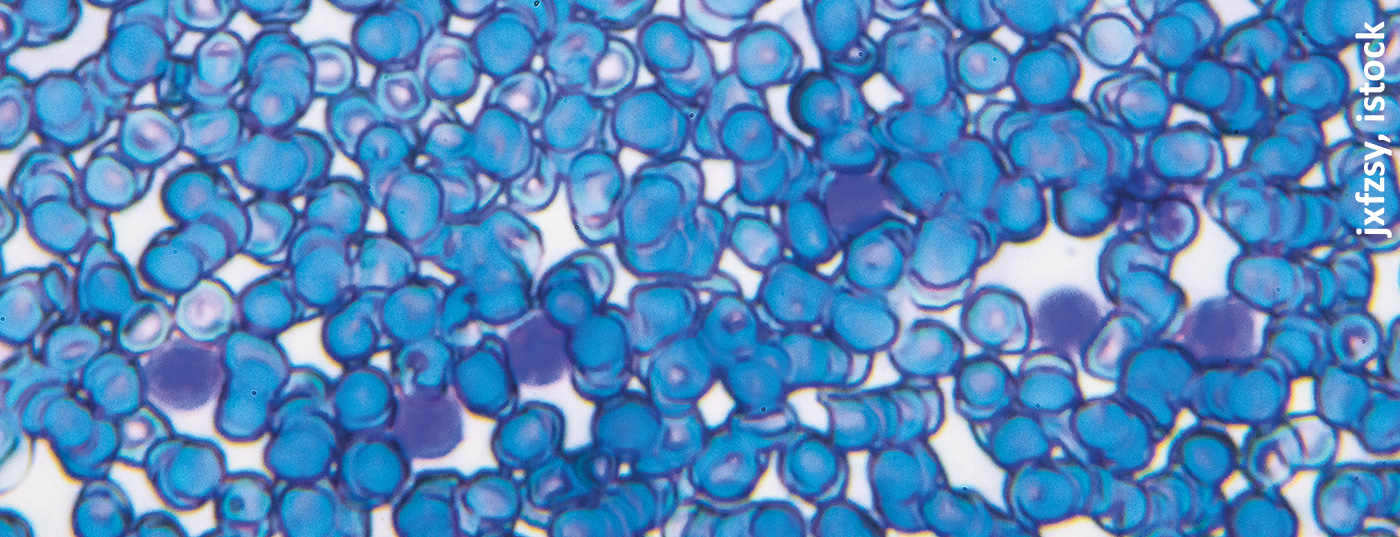
Patients with relapsed or refractory CD30-positive lymphomas underwent a novel cellular treatment option [1]. This combines natural killer cells (NK cells) with a bispecific antibody. The NK cells are derived from umbilical cord blood, pre-activated with cytokines and expanded in the laboratory. The bispecific antibody binds to CD30 on lymphoma cells and 16A on NK cells. The phase II/III study included 22 patients with lymphoma who had relapsed after many different treatments. All but one patient had previously received immunotherapy with a PD-1 inhibitor, 14 had undergone autologous or allogeneic stem cell transplantation, and two had previously received chimeric antigen receptor (CAR) T-cell therapy. Patients had received an average of six prior therapies for relapsed or progressive disease, but some had received up to 14 prior therapies. In this study, patients underwent immune cell conditioning with fludarabine and cyclophosphamide followed by two cycles of the novel AFM13/NK cell complex and additional infusions of AFM13 alone 7, 14, and 21 days after the second infusion of complexed cells. The novel cell-antibody complex was administered in doses of 1 million, 10 million, or 100 million cells/kg; the highest dose was chosen as the recommended phase II dose.
The results are impressive. Overall, 53% of patients had a complete response to treatment, 37% showed a partial response, and 11% experienced disease progression. The overall response rate for patients who received a higher dose was 100% (13 patients), with eight patients having a complete response and five having a partial response. At a median follow-up of 9 months, the progression-free survival rate was 52% and the overall survival rate was 81%. The corresponding rates in patients receiving the recommended phase II dose were 67% and 93%. In addition, the tolerability profile is excellent, with no cases of cytokine release syndrome, immune effector cell-associated neurotoxicity syndrome (ICANS), or graft-vs-host disease. the study provides evidence that performing memory-like NK cell infusions with a combined engager can result in excellent short-term responses in an antigen-specific manner. However, a longer follow-up period is required, as five of the patients with complete response relapsed within one year of follow-up.
Tackling solid tumors with CAR-T cells
Chimeric antigen receptor T cell (CAR-T) therapy has achieved impressive success in patients with hematologic cancers, but similar results for patients with solid tumors have been lacking. Now, a new CAR-T construct targeting the tumor-specific antigen claudin 6 (CLDN6) is showing promising preliminary activity in relapsed or refractory advanced solid tumors, particularly testicular and ovarian cancers, according to initial data. This novel CAR-T therapy, administered as monotherapy and in combination with an mRNA vaccine designed to boost T-cell responses, showed robust infiltration of T cells six weeks after infusion in a phase I study. Of 14 evaluable patients with CLDN6-positive solid tumors, six showed a partial response to therapy – four who received CAR-T monotherapy and two, with the combination of CAR-T agent and vaccine.
To date, the use of CAR-T therapy to treat solid tumors has been disappointing. It has been hampered largely by difficulties in identifying targets that spare healthy cells while maintaining an adequate T-cell response over time. Claudin 6 represents a promising target because the protein is abnormally expressed in several cancers, including testicular, ovarian, uterine, and lung cancers, but not in healthy adult tissue. In the first part of the Phase I study, patients received escalated doses of CLDN6-CAR-T monotherapy following lymphocyte depletion. In part 2, patients received increased doses of BNT211 combination therapy, with mRNA vaccine (CARVac) administered every two to three weeks up to 100 days after CAR-T cell transfer. Of 16 patients included, four with testicular cancer and two with ovarian cancer showed a partial response, corresponding to an objective response rate of 43%. The rate of disease control was 86%. The researchers also observed a deepening of partial responses 12 weeks after infusion. The therapy was particularly promising in five patients with testicular cancer treated with the higher of the two doses: one complete response, three partial responses, and one case with stable disease. This group achieved an objective response rate of 80% and a disease control rate of 100%.
Congress: American Association for Cancer Research (AACR) Annual Meeting 2022
Literature:
- Truly Impressive Responses in Lymphoma With Novel Cell Therapy. Medscape. 11.4.2022. AACR 2022 Annual Meeting. Abstract CT003.
- Novel CAR T Therapy for Solid Tumors: ‘Exciting Advance’. Medscape. 18.4.2022. AACR 2022
InFo ONCOLOGY & HEMATOLOGY 2022; 10(3): 17 (published 6/22, ahead of print).