Every year in December, around 7500 breast cancer experts from all over the world meet at the San Antonio Breast Cancer Symposium. The highlights of current breast cancer research on prevention, diagnosis and therapy will be discussed. Over 1000 abstracts were submitted and discussed. This makes the meeting one of the most important opportunities for experts to discuss the latest data.
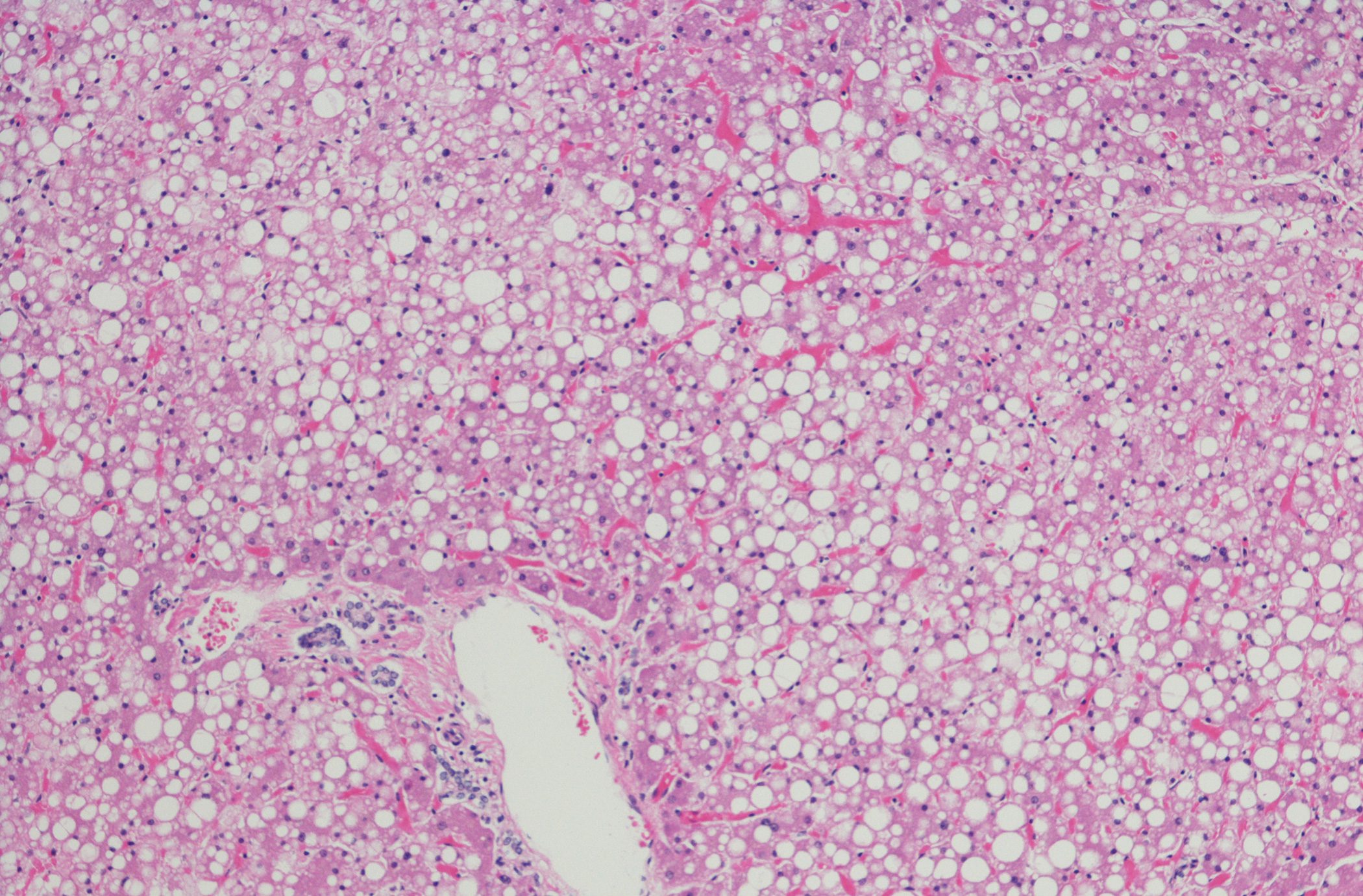
Breast cancer is not only widespread, it is also a type of cancer that is associated with obesity. Eating healthy foods can serve as a protective factor that has been shown to reduce the risk of obesity and postmenopausal breast cancer mortality, a recent study has revealed [1]. A cross-sectional ecological analysis was conducted by combining data on postmenopausal breast cancer mortality from 2010 to 2020 from the Centers for Disease Control and Prevention (CDC) with aggregated data from the US Department of Agriculture’s Food Environment Atlas from 2012 to 2020. The value for the “food swamp” was calculated as the ratio between fast food/convenience stores and grocery stores and farmers’ markets. The “food desert” score was calculated as the percentage of residents who live more than 1 mile (urban) or 10 miles (rural) from a grocery store and whose household income is ≤200% of the federal poverty level. The researchers categorized food deserts and swamps as low, moderate or high, with higher scores representing districts with fewer resources for healthy food. Counties with high postmenopausal breast cancer mortality rates had higher percentages of poverty rates (17.2% vs. 14.2%), rates of adult obesity (32.5% vs. 32%), and diabetes (11.8% vs. 10.5%), compared with counties with low postmenopausal breast cancer mortality rates. The age-adjusted odds of counties having high postmenopausal breast cancer mortality were 53% higher in counties with high food desert scores and more than twice as high in counties with high food swamp scores.
Not too much of a good thing
Axillary lymph node dissection may be unnecessary in breast cancer patients with one or two positive sentinel lymph nodes if adjuvant nodal radiotherapy is performed. This is the conclusion of a large Scandinavian study [2]. 1204 patients with one or two positive sentinel lymph nodes underwent randomized axillary dissection, while 1335 patients with the same findings did not undergo dissection. The patients had clinically T1-3 N0 primary breast cancer. About 89% in both groups received adjuvant radiation, including radiation to the nodes, and almost all also received systemic therapy, which included endocrine therapy in over 90%. Only about 2% of patients received neoadjuvant therapy.
At a median follow-up of almost four years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection group and 7.1% in the group without dissection having a recurrence. The estimated recurrence-free 5-year survival rate was just under 90% in both groups. Omitting the dissection was not inferior to performing it. In addition, however, the results reported by the patients were worse in the dissection group.
Interruption of endocrine therapy is harmless
New study data show that the risk of short-term cancer recurrence is not increased in young women with early hormone receptor (HR)-positive breast cancer who interrupt endocrine therapy to become pregnant [3]. There was concern that the use of fertility preservation methods or assisted reproductive technology could have harmful effects on patients with HR-positive breast cancer – especially if they involve the use of hormones. Therefore, a secondary analysis was conducted in which the researchers focused on the resumption of menstruation and the use of fertility preservation and assisted reproductive technologies.
Of the 516 women evaluated for the menstrual analysis, two thirds were aged 35 and over. Slightly more than half (53%) had amenorrhea at the time of inclusion in the study. Encouragingly, 85% of the women had their periods again within six months and 94% within 12 months of stopping endocrine therapy. Of 497 evaluable participants who paused endocrine therapy to attempt pregnancy, 368 (74%) became pregnant. Looking at the time until pregnancy, there was a clear correlation between younger age and faster pregnancy. In a multivariable model, age <35 years was the only factor independently associated with shorter time to pregnancy.
In terms of fertility preservation and the use of assisted reproductive technologies, about half of the women (51%) were undergoing some form of fertility preservation at the time of breast cancer diagnosis and before the start of the study, most commonly ovarian stimulation for embryo or egg cryopreservation. After inclusion in the study, the figure was 43%. In the multivariable model, cryopreserved embryo transfer was the only assisted reproductive technology that was significantly associated with a greater chance of pregnancy and more than doubled the patient’s chances. However, age also plays a decisive role here: women under the age of 35 had a 50% higher chance of becoming pregnant than women aged between 35 and 39 and 84% higher than women aged between 40 and 42. But there were no obvious short-term adverse effects on breast cancer outcomes. After three years, the breast cancer-free interval between women who underwent ovarian stimulation for cryopreservation and women who did not was almost identical at 9.7% vs. 8.7%.
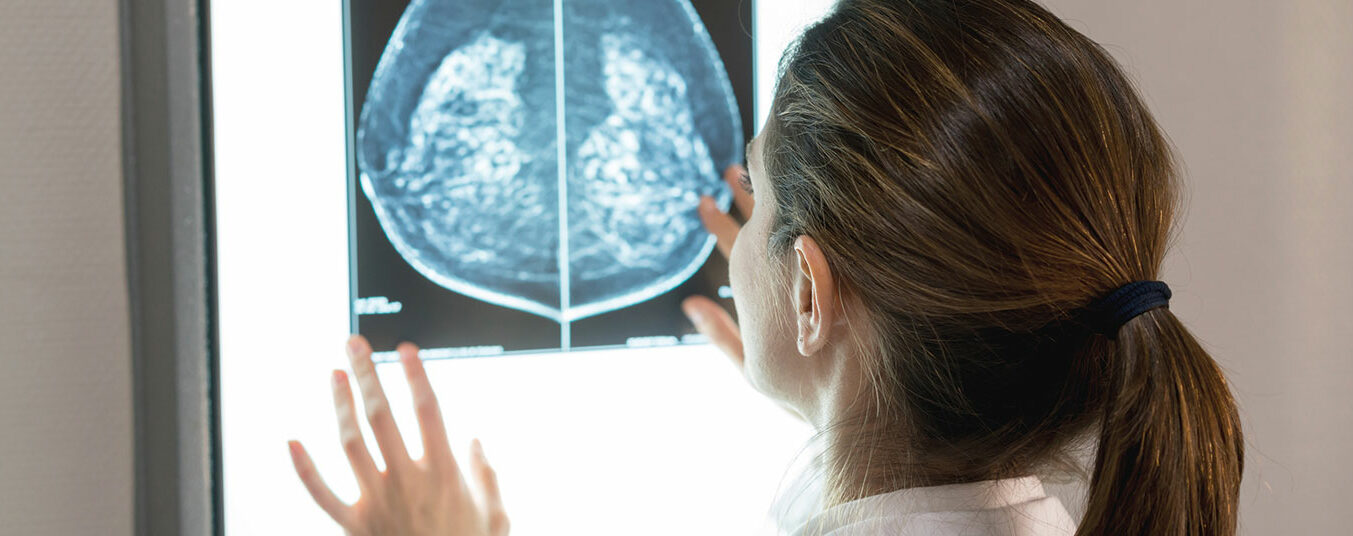
Extend mammography intervals
Women aged 50 years and older who have undergone curative treatment for breast cancer and are still cancer-free after three years can safely deviate from the recommended annual mammography surveillance, according to the results of a new randomized study [4]. To this end, 5235 women aged 50 and over were randomly selected for an annual or less frequent mammogram. Invasive carcinoma was found in 87% of the women, while 13% had ductal carcinoma in situ. After a mean follow-up period of 8.7 years, recurrence occurred in 7% of the women. After 5 years, the breast cancer-specific survival rate was 98.1% in the group with annual examinations and 98.3% in the group with longer intervals. There was also no difference in the rates of recurrence-free survival and overall survival.
However, the prerequisite is that the patients are cancer-free three years after curative treatment. This is because it is known that all breast cancer patients have several peak values for recurrence. A peak is reached two to three years after curative treatment in high-risk patients. The other peak is at the start of hormone therapy, i.e. at five to six years. But this particular group of patients has a low to medium risk and are therefore not the high-risk patients participating in treatment trials.
Pregnant with breast cancer
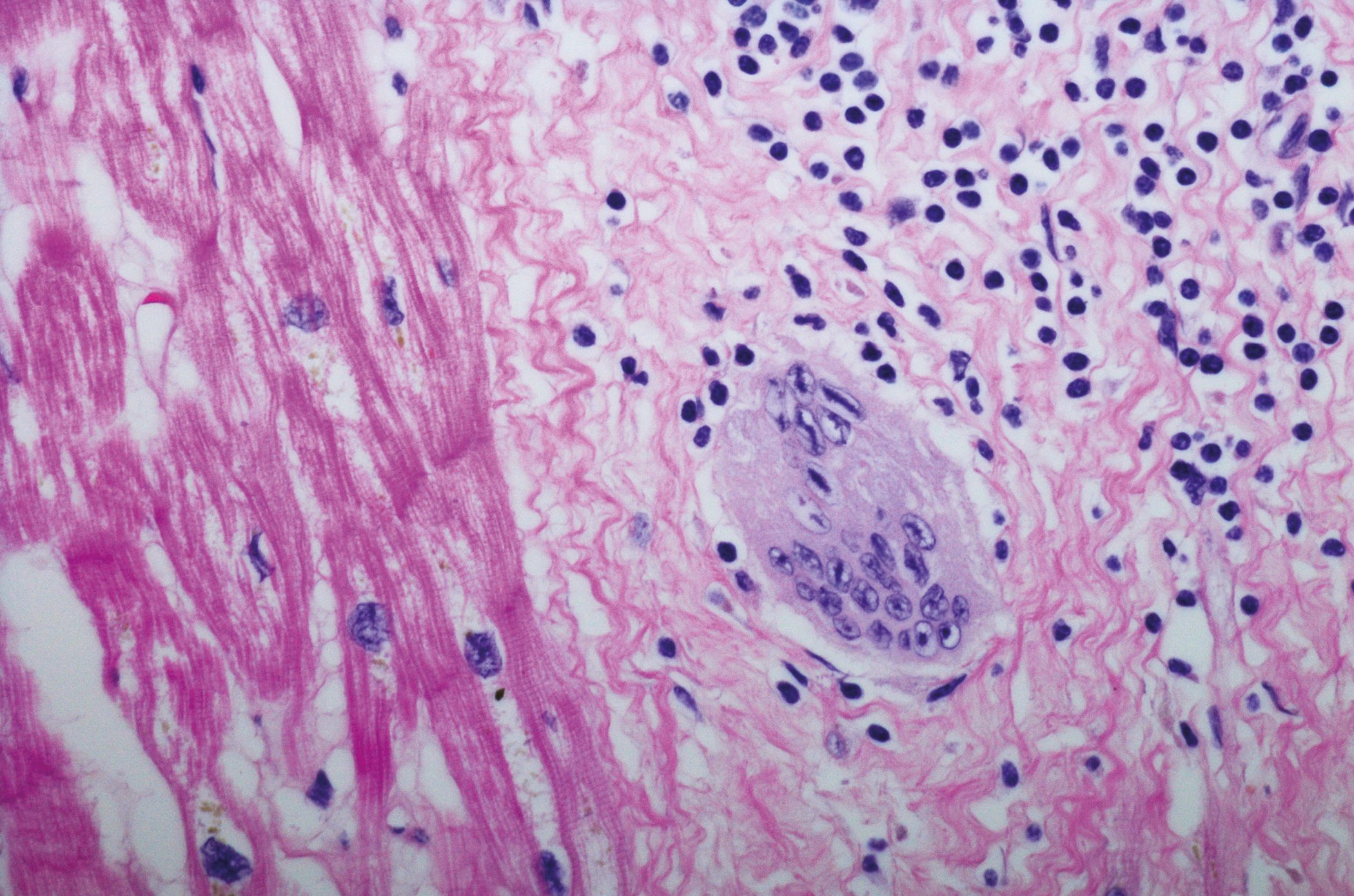
Breast cancer during pregnancy is a very difficult clinical situation, as the expected antineoplastic effects of treatment must be carefully weighed against possible harmful consequences for the developing fetus. According to a retrospective cohort analysis, exposure to taxanes during pregnancy appears to be safe for mothers and offspring [5]. As a rule, anthracycline-based chemotherapeutic agents are used during pregnancy, as more safety data are available. However, study results suggest that taxanes may be more effective in certain clinical situations. The safety concerns regarding taxanes relate to a potentially prolonged effect and a correspondingly higher risk of adverse effects, as the newborns lack the cytochrome enzymes for metabolizing the drugs. On the other hand, pregnant women metabolize taxanes faster and there are placental barriers that can prevent high molecular weight molecules such as taxanes from reaching the fetus.
The researchers recruited 103 women with an average age of 34 years from ten centers in six countries. The vast majority were also treated with anthracyclines during pregnancy, and almost all (97%) were treated with paclitaxel. The live birth rate was 98%, 43.4% were preterm, 24% were small for gestational age, 16% were admitted to the neonatal intensive care unit and 12.5% had hyperbilirubinemia. Obstetric complications included intrauterine growth restriction at 9%, premature rupture of membranes at 5%, as well as gestational diabetes mellitus, hypertension (4%) and pregnancy loss at 2%.
Inadequate supply
Guideline-compliant care is associated with improved overall survival in patients with inflammatory breast cancer. However, a large proportion of those affected do not receive this treatment at all, as a retrospective study of patients with inflammatory breast cancer revealed [6]. Inflammatory breast cancer is an aggressive form of breast cancer that is associated with poorer survival rates compared to other subtypes of breast cancer. Guideline-compliant treatment consists of neoadjuvant chemotherapy, followed by a modified radical mastectomy without immediate reconstruction and radiotherapy after the mastectomy.
The study analyzed data from 6945 women with non-metastatic inflammatory breast cancer. Guideline-compliant care was defined as trimodal treatment given in the correct sequence, with neoadjuvant chemotherapy started within 60 days of diagnosis. In 88% of patients, neoadjuvant chemotherapy was not initiated within 60 days of diagnosis. About half of all patients did not receive appropriate surgical treatment (modified radical mastectomy without immediate reconstruction and post-mastectomy radiotherapy) and only about one third of the cohort received guideline-conform treatment at all. However, guideline-compliant treatment and private insurance were both positively associated with better overall survival.
Congress: San Antonio Breast Cancer Symposium (SABCS) 2023
Literature:
- Bevel M, et al: Living in a Food Swamp Tied to High Breast Cancer Mortality. Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 08.12.2023.
- De Boniface J, et al: Nodal Radiation May Make BC Axillary Dissection Unnecessary. Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 06.12.2023.
- Azim HA, et al: Patients With HR-Positive Breast Cancer Can Safely Use Assisted Reproductive Technology. Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 08.12.2023.
- Dunn J, et al: Women Older Than 50 May Safely Deescalate Mammogram Frequency Following Surgery. Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 07.12.2023.
- Ferrigno Guajardo A, et al: Answering the Unknowns of Taxanes for Breast Cancer During Pregnancy. Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 09.12.2023.
- Diskin B, et al: Few With Inflammatory Breast Cancer Get Guideline-Based Care Abstract. San Antonio Breast Cancer Symposium (SABCS) 2023, 09.12.2023.
InFo ONKOLOGIE & HÄMATOLOGIE 2024; 12(1): 20-21 (published on 12.3.24, ahead of print)