If hair begins to thicken in a man or woman, there are many ways to react to this symptom. If the despair caused by hair loss is great, the hair consultation at the USZ, for which PD Dr. med. Thomas Kündig is responsible, is an important point of contact. There, a dermatological and trichological examination is performed and, depending on the underlying disease, therapy is initiated.
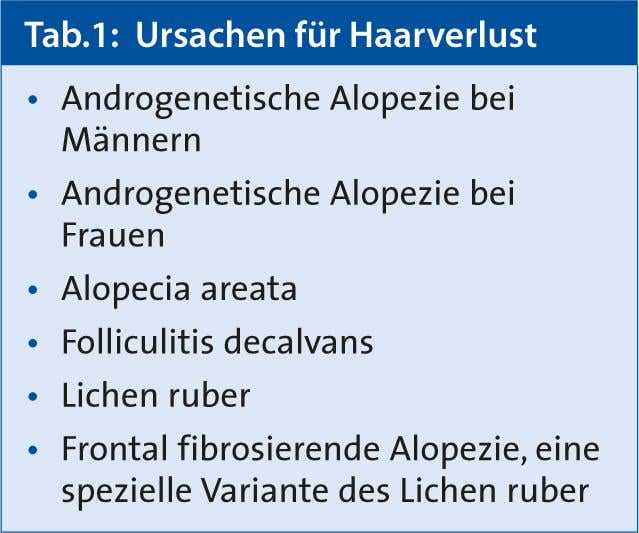
Hair loss includes two problem areas: increased daily hair change (effluvium) or visible hairlessness (alopecia). A loss of up to 100 hairs per day is normal. The most common causes of hair loss presented by PD Dr. med. Thomas Kündig at a training event in Zurich are summarized in Table 1.
Hair growth and loss are influenced by hormones, growth factors, medications and seasons, among other factors. The growth of each of the approximately 100,000 scalp hairs occurs in cycles, consisting of a perennial growth phase (anagen phase), a short follicular regression phase (catagen phase), and a two- to four-month resting phase (telogen phase). The hair stem cells of the hair follicle are located in the so-called hair bulge. If inflammation occurs there, the loss of stem cells results in scarring alopecia, i.e. irreversible hair loss. Once the inflammation has burned out, its cause can no longer be determined. The final stage of all scarring alopecias is the same. Typical picture both in dermoscope and histologically is the absence of hair follicles and scar tissue.
If the inflammation occurs at the hair root (bulb), the result is non-scarring alopecia. The prototype is alopecia areata. The hair is thinner, caliber variations, empty hair follicles and often a yellow halo around the hair follicles are found. The sensitivity of dermoscopy is higher than that of the trichogram, Dr. Kündig explained in this context.
The discussion remains open on the role of vitamins and trace elements. Cysteine, histidine, copper, zinc, niacin topical, biotin and niacin oral… for all of them there are studies that prove once more, once less effects on hair growth. “Interestingly, laboratory tests have shown that the levels in patients with hair loss are sometimes even above the normal values for vitamins and trace elements,” Dr. Kündig commented.
Alopecia by gender
Man and woman show very clear local differences in the distribution pattern of hair loss in androgenetic alopecia. In men, it is classified according to Hamilton-Norwood stages I-VII, and in women, it is divided into three stages according to Ludwig. In contrast to men, not all hair follicles of a head region are usually affected in women. Therefore, they do not experience complete baldness, but diffuse thinning of hair in the mid-parietal area.
Risk factors for male androgenetic alopecia are a certain genetic disposition, gender and age: in many affected individuals, hair loss begins as early as puberty. The role of serum levels of testosterone and dehydroepiandrosterone is questionable, as no other features of increased androgen action are evident, such as increased beard growth. Genetic predisposition has been shown in monozygotic twins with a concordance of 80-90%, there is a strong correlation to the father’s family. Caucasians are more commonly affected than Asians, “genome wide screenings” showed loci of increased risk (20p11.22).
The crucial androgen in male hair loss is dihydrotestosterone (DHT), which is formed from testosterone with the help of 5α-reductase type II. Under the influence of the androgen DHT, a miniaturization of the genetically predisposed hair follicles and thus also of the hair results.
In female androgenetic alopecia, everything is different. In later age, hair density decreases constantly in women; an acceleration in menopause could not be found. In a cohort of 1000 women with hyperandrogenism, only 4% have androgenetic alopecia and 75% have hirsutism. There is no genetic predisposition, only low-grade concordance in monozygotic twins, case-control studies showed no genetic associations. The familial disposition is much less pronounced in women than in men.
Treatment options for women
“All women are skeptical when you inform them that help is available,” in Dr. Kündig’s experience. The most effective substance against female androgenetic alopecia is the topical application of minoxidil solution, as demonstrated by numerous well-controlled clinical studies. Minoxidil has an almost linear dose-dependent effect. Minoxidil twice a day is more effective than once (44.1 hairs/cm2 vs. 64.4 hairs/cm2) [1]. “If you want more hair, you have to put more on,” Dr. Kündig said. Recommended for use two hours before bedtime to prevent contamination of facial skin. A 2 percent minoxidil solution should be started, as the 5 percent solution often leads to the growth of vellus hair on the face as a side effect. However, the phenomenon is reversible and disappears four months after discontinuation.
A 5% formulation is almost twice as effective, but the adverse effects are then also more frequent. 5% Minoxidil causes irritation of the scalp. The problem is propylene glycol, which is used as an excipient. The problem cannot be minimized with an individual formulation either. Alopexy® 2% solution, for example, therefore contains six times less propylene glycol and cyclodextrin instead. Minoxidil monotherapy is equally effective as a combination with shampoo or tretinoin. Seborrheic eczema is more common because fewer hairs are less effective at removing sebum from the scalp.
For alopecia with hyperandrogenemia, systemically given antiandrogens such as cyproterone acetate, chlormadinone acetate, or dienogest are available. However, in a comparative study with minoxidil, the cyproterone acetate group performed significantly worse [2]. This, too, is an indication that testosterone does not play the decisive role in female androgenetic alopecia, as has long been assumed, Dr. Kündig explained.
Ell-Cranell alpha 0.025% solution, topical alfatradiol, is popular with men because of its relatively rapid onset of action. In women, on the contrary, it does nothing, the thickness of the hair does not increase under it. Finasteride is even rather counterproductive in women, Dr. Kündig added.
Therapy for men
For the treatment of male androgenetic alopecia, there are only two agents that have been proven in well-controlled, scientific studies: The finasteride 1 mg tablet, where the dose is clearly established, and the 2 or 5 percent minoxidil solution or foam. In a study comparing minoxidil with finasteride, it became clear that the effect depended on the dose of minoxidil [3]. A combination is also an option, he said. However, Dr. Kündig prefers to give patients topical minoxidil in high doses. Hair loss is thus stopped in about 90% of those treated. In about 50% of patients, there is even a visible thickening of the hair in the course of therapy. In the discussion at the training event in Zurich, experienced users brought up the point that the efficacy at the crown and the back of the head can be different.
Higher dosages of finasteride do not bring more hair. Finasteride selectively inhibits the enzyme 5α-reductase type II, thereby reducing serum concentrations of dihydrotestosterone by 70%. It is important to note here that it takes six months for more hair growth to show up and twelve for it to really be noticeable. “You have to tell people that”. Maximum densification is achieved with minoxidil after only six months. The effect lasts as long as the respective drug is taken continuously.
Source: USZ Regional Dermatology Series: Diseases of the Head/Facial Skin, April 11, 2013 in Zurich.
Literature:
- Olsen EA: Five-year follow-up of men with androgenetic alopecia treated with topical minoxidil. J Am Acad Dermatol 1990; 22(4): 643-646.
- Vexiau P, et al: Effects of minoxidil 2% vs cyproterone acetate treatment on female androgenetic alopecia: a controlled, 12-month randomized trial. Br J Dermatol 2002; 146(6): 992-999.
- Saraswat A, Kumar B: Minoxidil vs finasteride in the treatment of men with androgenetic alopecia. Arch Dermatol 2003; 139(9): 1219-1221.











