Psychiatry was also a topic at the Update Refresher General Internal Medicine in Zurich. Thomas Heinsius, MD, of the Psychiatric Polyclinic of the Integrated Psychiatry Winterthur (ipw), gave a broad overview of psychotropic drugs. Which substances are used when and what risks should be considered? He also discussed the various clinical pictures of anxiety disorders. Here he particularly emphasized the importance of psychotherapeutic approaches.
Thomas Heinsius, MD, Psychiatric Polyclinic of the Integrated Psychiatry Winterthur (ipw), started his review with a meta-analysis on antipsychotics [1]. Here, it became apparent that above all the individual effect and side effect profiles should guide the choice of substances. The only antipsychotic with clear evidence of improved efficacy is clozapine (Leponex
®
). It also causes significantly fewer extrapyramidal side effects than other drugs (odds ratio 0.3 vs. placebo). The two substances amisulpride (Solian®) and olanzapine (Zyprexa®) show a trend towards better applicability in various studies. They followed behind clozapine in the efficacy endpoint. Furthermore, amisulpride was the least likely to cause individuals to discontinue therapy (followed by olanzapine and clozapine). However, the risk of weight gain-possibly a relevant factor in the shortened life expectancy of schizophrenics-is greatest for olanzapine.
Recent data on adverse effects of antipsychotics indicate greater loss of brain tissue at higher doses. In rodents and primates, eight weeks of treatment with antipsychotics showed loss of brain volume, and there was also increased mortality compared with placebo in patients with dementia.
According to Dr. Heinsius, the consequences for the clinical use of antipsychotics are therefore:
- The core indications for antipsychotics are psychoses and deliriant-agitated states (especially in the elderly).
- The selection of the appropriate substance is made individually according to the effect and side effect profile.
- Cautious up-dosing is indicated, especially in elderly (confused) patients.
- The use of antipsychotics should be considered in other psychiatric disorders such as depression, anxiety, or obsessive-compulsive disorders only after all other therapeutic options (especially psychotherapeutic and psychosocial interventions) have been exhausted.
Among the benzodiazepines, Dr. Heinsius mentioned lorazepam (Temesta®), alprazolam (Xanax®), oxazepam (Seresta®), and diazepam (Valium®). Benzodiazepines have a rapid onset of action and a broad therapeutic range. An important side effect is sedation (CAVE driving). The risk of dependence due to the development of tolerance should also be considered in any case. Its use is conceivable in acute situations until other therapies are effective – after exhaustion of the other therapeutic options, it may also be used in the longer term.
Antidepressants
“One important group of psychotropic drugs is antidepressants,” Dr. Heinsius said. “A large complex database exists on their use during pregnancy. The state of current knowledge can be read on the well-maintained and actively maintained website www.embryotox.de.” These agents are increasingly prescribed despite two critical meta-analyses in 2008 that showed only a small effect for all antidepressants compared with placebo. While 5.8% of the U.S. population was taking antidepressants in 1995, this figure had risen to 10.1% by 2005 (3.6% in Switzerland in 2008). Turner et al. [2] demonstrated that many antidepressant trials submitted to the FDA with negative or questionable results were not published in the first place. “We only have access to a selected, embellished set of data, which is highly problematic,” Dr. Heinsius said. Considering all FDA data, the effect size (overall -32%) is significantly worse than it appears in the literature.
Kirsch et al. [3] demonstrated in their meta-analysis (also based on FDA data), on the one hand, that antidepressants produced a good reduction in the Hamilton Depression Rating of 9.6. On the other hand, a reduction of 7.8 was also obtained with placebo. Thus, the difference was 1.8 points, corresponding to an effect size of 0.32. However, according to NICE, the cutoff for clinical relevance is a 3-point difference and an effect size of 0.5. Consequently, if this criterion is followed, the antidepressants were not relevantly more effective than placebo. Only among the very severely depressed was the difference between placebo and antidepressants significant (but remained comparatively small). According to DGPPN guidelines, antidepressants should therefore not generally be used for the initial treatment of mild depression, but only after critically weighing the advantages and disadvantages of such treatment.
“Prescription must be integrated into an overall treatment concept and into a trusting doctor-patient relationship. Clinical checks should be carried out closely at the start of treatment. The patient must be informed in detail about the risks and side effects,” the speaker emphasized. “Psychotherapy works best. It is an important part of treatment and should not be forgotten.”
Anxiety disorders
According to Dr. Heinsius, fear is in principle a natural reaction to ensure survival that occurs in all people. Anxiety of disease value is common in the population (1-year prevalence is approximately 15%). The modern classification systems distinguish different types of conciseness. Overlap between the different types is common.
Panic attack: sudden onset of anxiety or discomfort with a peak within ten minutes. It causes many physical symptoms initially, such as rapid heartbeat, sweating, tremors, shortness of breath, dizziness, nausea, and chest pain, and only later psychological symptoms (e.g., derealization; depersonalization; fear of dying).
Panic disorder: A panic attack is not yet a disease in the true sense of the word. Only when the panic attacks recur unexpectedly and there is persistent concern about the recurrence and significance of the attack for at least a month after the attack, and subsequently significant changes in behavior, is it said to be a panic disorder. It may be accompanied by agoraphobia. Induction by any substances or drugs must be excluded.
Social phobia/anxiety disorder: This involves either a marked fear of being the center of attention or embarrassment, or a marked avoidance of such situations. There are typical anxiety symptoms and therefore a clear emotional burden (also due to the avoidance behavior). Those affected have insight that the fears are exaggerated.
Specific phobias: In principle, the same applies as for social phobia, but the fears are directed towards specific objects (e.g. animals) or situations (e.g. heights, flying).
Where does fear come from and how can you fight it?
On the one hand, genetic predisposition plays a role in the development of anxiety disorders, as shown by various twin studies (the agreement regarding the diagnosis of panic disorder was significantly higher in monozygotic twins compared to dizygotic twins). In addition, early stresses such as the death of a parent, sexual or other physical abuse in childhood, but also the current living and working situation as well as current social constellations are important factors for the development of an anxiety disorder. In the so-called bio-psycho-social model according to Gilbert all these parameters are summarized. Within the framework of this model, the various biological, psychological, and social factors influencing the development of mental disorders are well represented.
Psychotherapy is, according to current knowledge, the treatment of first choice for uncomplicated panic disorder, social phobia, specific phobias and agoraphobia. The best studied is cognitive behavioral therapy. Its active components are:
- Eduction of the patient
- Hyperventilation control
- Exposure procedures (introceptive and situational).
Before the confrontation phase, the intensity level of anxiety increases rapidly and the patient wants to flee from the unpleasant situation. This is because he fears an exponential increase in the anxiety curve if he is exposed to confrontation. But if he does so in a psychotherapeutically well-supervised environment, at some point during the confrontation he experiences a turning point at which the anxiety curve slowly declines. So the fear can’t keep increasing. This must be made clear to the patient. The relief and later the satisfaction of having succeeded gives him longer-term confidence in dealing with such situations. “On the whole, self-help, i.e. information for the patient, e.g. via a self-help book, is often not promoted enough. Yet this is a very useful and helpful supplementary method, especially for educated people. The patient must be aware of the mechanisms of his anxiety disorder. Then he can also combat it effectively and break the vicious circle of anxiety,” explained Dr. Heinsius.
Sustainable therapy
Medication options include antidepressants and benzodiazepines. An overview of the drugs approved in Switzerland for the treatment of anxiety disorders is given in Table 1.
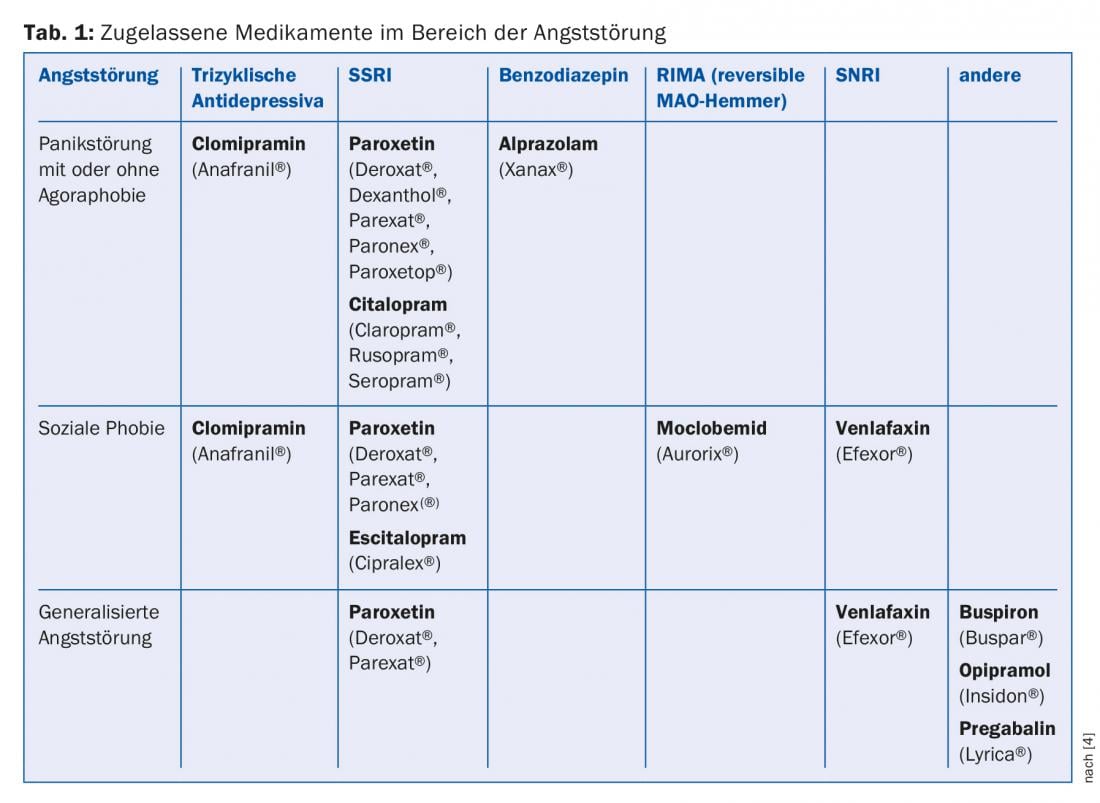
Efficacy has been demonstrated for both groups of substances. However, the use of benzodiazepines in particular must be well weighed because of side effects. Other medications used for anxiety disorders include herbal agents and beta-blockers.
Several meta-analyses found that although pharmacotherapy had a comparable effect size to psychotherapy (approximately 0.4 vs. 0.6) immediately after treatment. However, if the medication is not taken over a certain period of time, the effect is completely lost. At follow-up, the effect size was 0, whereas that of psychotherapy remained the same or even increased. “Medications for anxiety are thus only effective as long as they are taken. My experience, however, is that patients would like to get off the medication. Psychotherapy is the only thing that helps here. Of course, both concepts can be well combined,” says the expert.
Source: General Internal Medicine Update Refresher, May 8, 2015, Zurich.
Literature:
- Leucht S, et al: Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 2013 Sep 14; 382(9896): 951-962.
- Turner EH, et al: Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med 2008 Jan 17; 358(3): 252-260.
- Kirsch I, et al: Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med 2008 Feb; 5(2): e45.
- Frommberger U, Angenendt J: Pharmacotherapy of anxiety disorders. Medication often reduces symptoms more quickly than psychotherapy. Ars Medici Dossier 2009; II: 16-19.
HAUSARZT PRAXIS 2015; 10(6): 38-40











