Palpitations are a common symptom and usually of harmless etiology. A targeted history taking together with the clinical examination and the resting ECG allow to decide which patients should be submitted to an extended diagnostic procedure and where an exspective approach may be chosen. An overview of current diagnostic triage and basic therapeutic concepts.
Palpitations (lat. palpitare = to tremble, to blink) are a frequent symptom in the general practitioner’s and cardiologist’s consultation [1] and are described by patients as heart stuttering, palpitations, palpitations or dropouts, among other symptoms. The term palpitations implies an unpleasantly experienced, increased, accelerated, or irregular heart action [2]. The causes of these symptoms are varied and range from harmless extrasystoles to potentially life-threatening ventricular tachyarryhthmias. Diagnosis of palpitations is sometimes difficult and lengthy due to the usually transient nature of the symptoms/arrhythmias. In the majority of patients, the cause of palpitations is benign and there is a low risk of mortality overall [3].
The task of the treating physicians is to document and diagnose any arrhythmias (symptom-rhythm correlation), to stratify the risk, and finally to provide arrhythmia-specific treatment if possible. Based on a careful history taking, clinical examination and the performance of a resting ECG, an initial clinical assessment is performed and a decision is made as to which patients should undergo the most targeted, further diagnostics.
Causes
Pathophysiologically, palpitations can be assigned to different mechanisms/causes (Tab.1), whereby three categories can be formed: On the one hand, too rapid, irregular or slow and vigorous contractions in the context of arrhythmias, on the other hand, intensified, violent contractions with abnormal cardiac motion in structural heart disease or increased stroke volume, and finally, changes in the subjective perception of the heartbeat, such as in psychosomatic disorders [4].
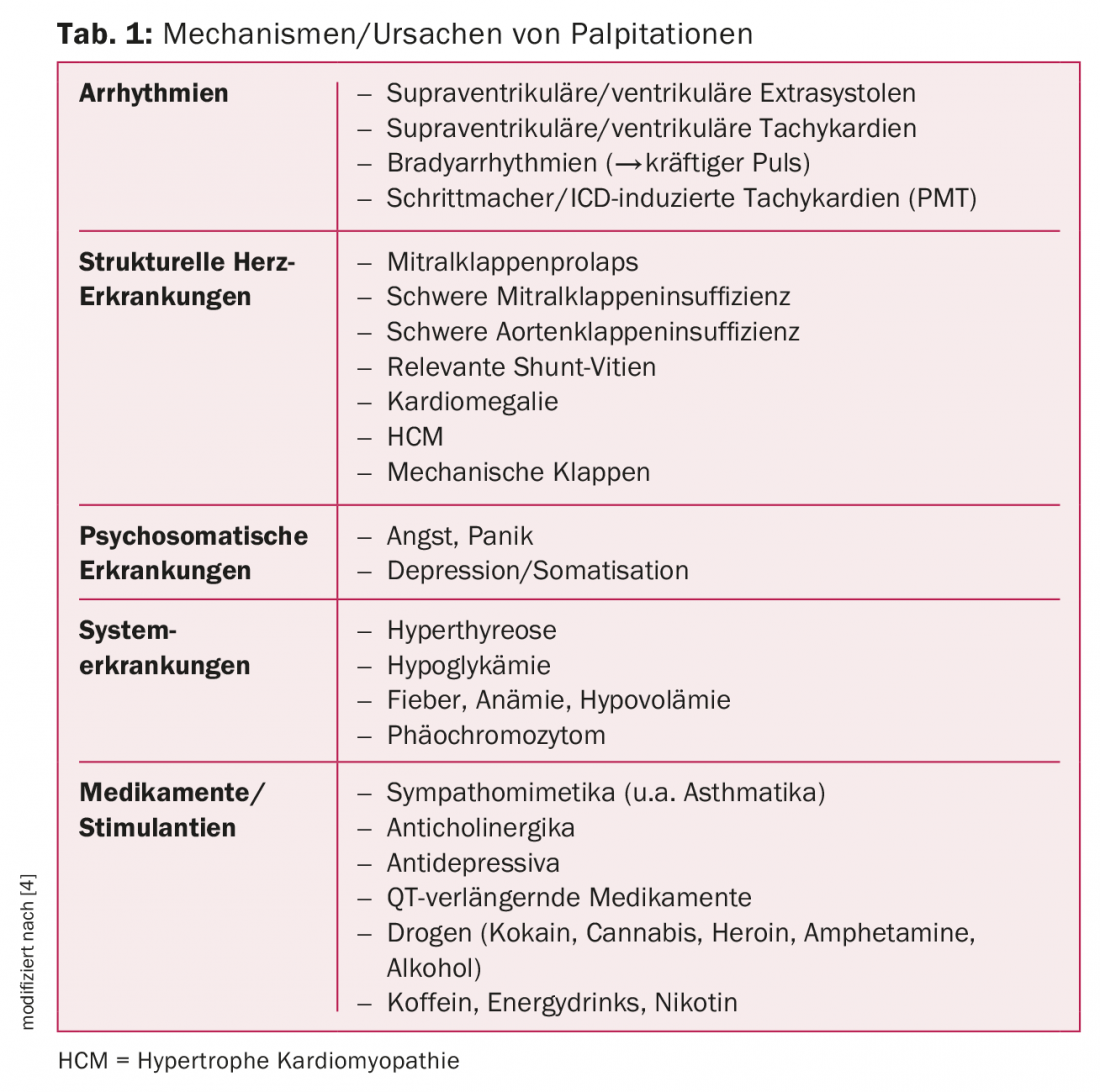
Palpitations in the context of arrhythmias can be triggered by atrial and ventricular extrasystoles, by regular or irregular ventricular or supraventricular arrhythmias. Male sex, older age, irregular palpitations, preexisting heart disease, and episode duration >5 min are suggestive of a rhythmogenic cause of palpitations [3].
In addition to structural heart disease, psychosomatic disorders are also a frequent cause of palpitations. Primarily, a somatic genesis (arrhythmias, structural heart disease) should be excluded. It is not uncommon for patients with supraventricular tachycardia to be falsely diagnosed with psychosomatic disease, which can ultimately be cured by antiarrhythmic therapy. Younger age and female gender may indicate a psychosomatic cause [5].
Especially in sinus tachycardias, but also in atrial fibrillation, (multifocal) atrial tachycardias, and less so in the other tachyarrhythmias, internal diseases (hyperthyroidism, anemia, infections, dyselectrolytes, etc.), stimulants, or drugs should be considered.
Basic diagnostics
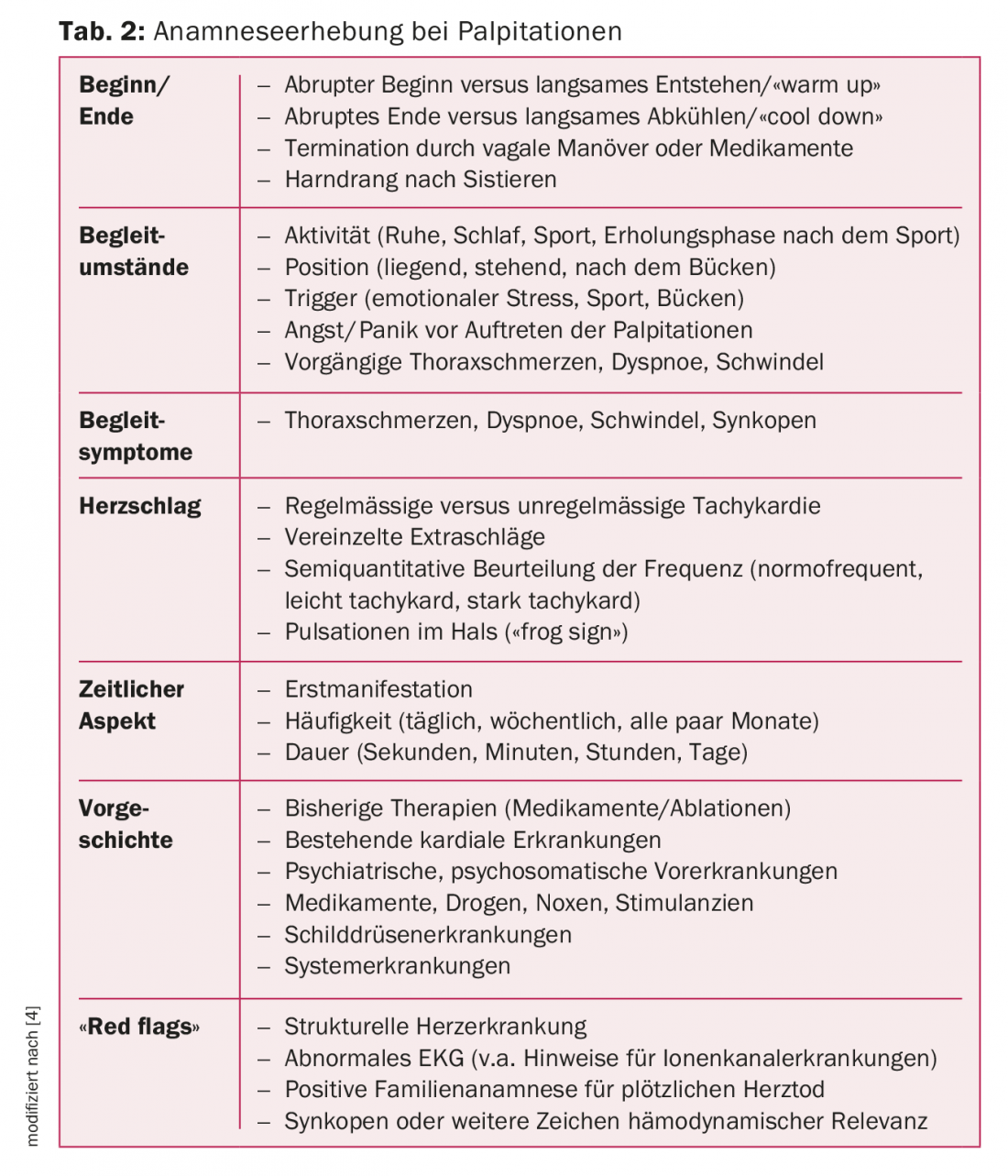
The basis of the clarification of palpitations is a detailed medical history. After the patient has described his symptoms, palpitations should be explored specifically. Table 2 summarizes the most important questions. The questioning is on the one hand about the assessment of the symptoms during the episode(s), on the other hand about the behavior of the heartbeat, as well as the episode frequency and possible trigger factors. In addition, asking about associated syncope, sudden cardiac death (1st- and 2nd-degree relatives), and the presence of structural heart disease can already provide initial risk stratification.When characterizing palpitations, it may be helpful to ask the patient to pre-tap the rhythm and frequency of palpitations. Overall, the history may provide clues to specific arrhythmias, but the overall diagnostic accuracy is low [6].
The clinical examination involves looking for evidence of the presence of structural heart disease (vitiation, cardiomegaly, signs of heart failure, etc.) and any systemic disease (hyperthyroidism, anemia, etc.).
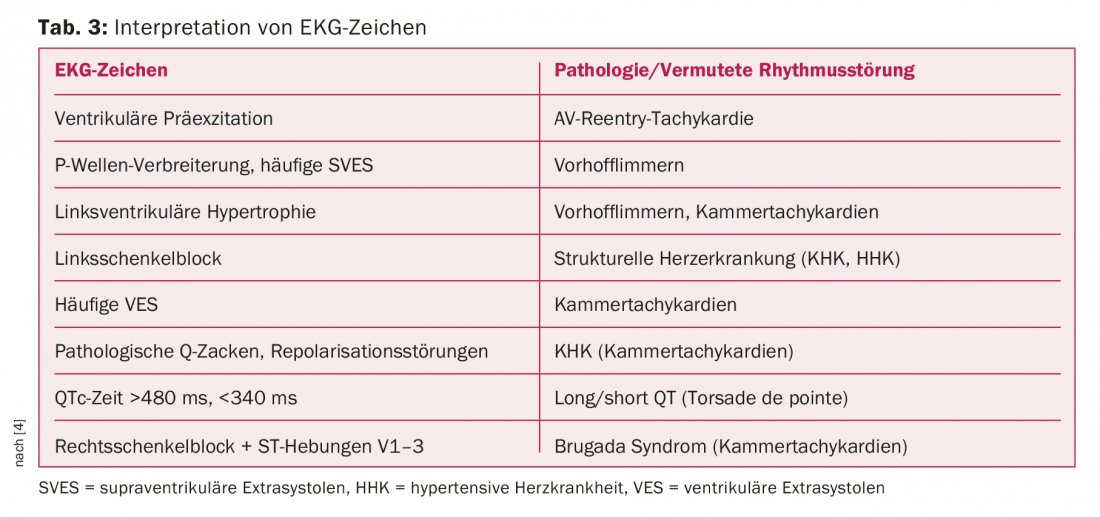
If the patient experiences palpitations during the consultation, then the first step is to perform a resting ECG. The 12-lead ECG during palpitations is considered the diagnostic gold standard. It is indispensable in the evaluation of palpitations/potential arrhythmias. In the case of persistent palpitations, a symptom-rhythm correlation can be established directly. Otherwise, the ECG is used for further risk stratification and cause clarification [4], (Table 3).
Extensive laboratory tests are not part of the initial diagnostic workup. In the authors’ opinion, however, thyroid values (TSH +/- peripheral thyroid values), hemoglobin and humoral inflammation values should be determined generously in the case of clinical abnormalities, since they can significantly influence the diagnosis and, in particular, further treatment.
History, clinical examination, and resting ECG allow initial assessment and help decide which patients should be evaluated further. The following flow chart illustrates the clarification process (Fig. 1).

Advanced diagnostics
If the cause of the palpitations is unclear after basic diagnostics, advanced diagnostics should be evaluated by the cardiologist, especially if there is evidence of hemodynamic relevance of the palpitations, structural heart disease, or other “red flags” (Tab.2). In patients with structurally normal cardiac findings and rare (oligosymptomatic) episodes, this may be omitted. In the extended workup, correlation of symptoms with rhythm is the gold standard for confirming the diagnosis and classifying palpitations into rhythmogenic and nonrhythmogenic causes. Depending on the frequency and duration of the episodes, an appropriate monitoring device is selected (Tab. 4) .
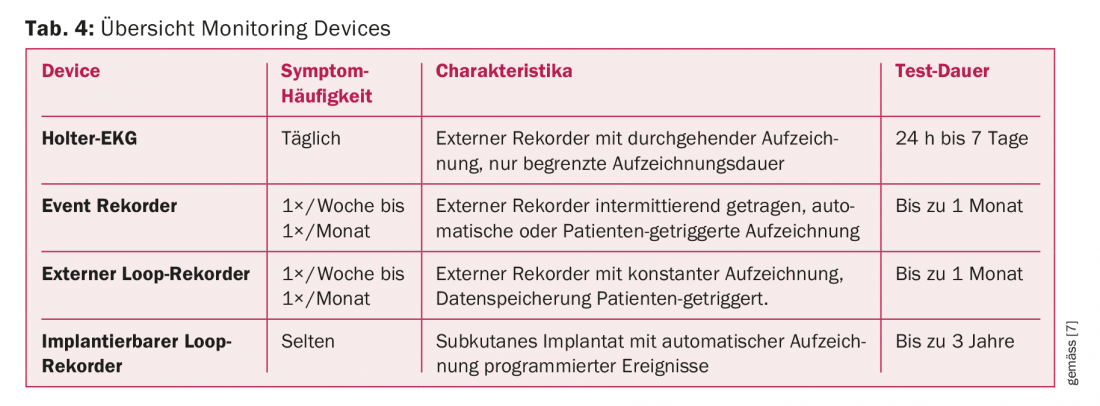
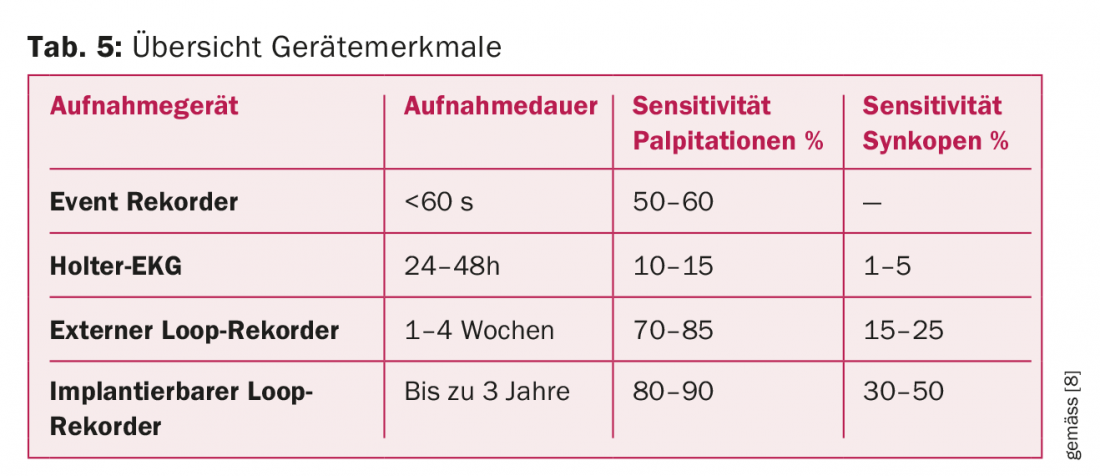
Ideally, the documentation of the actual arrhythmia is successful; at the same time, the beginning and end of the arrhythmia provide important information about its mechanism and the exact diagnosis. The specificity of the tests is high, at least for differentiating whether the palpitations are rhythmogenic or non-rhythmogenic. The sensitivity varies depending on the device and the question (Tab. 5).
In addition to ECG diagnostics/recording for the purpose of symptom-rhythm correlation, echocardiography with the question of structural heart disease is also part of the extended workup. Echocardiography provides important information that may be helpful for both risk stratification and origin of the arrhythmia. For example, a left ventricular ejection fraction (LVEF) <35% increases the likelihood of ventricular tachyarrhythmias and sudden cardiac death, as do findings of hypertrophic (obstructive) cardiomyopathy or arrhythmogenic right ventricular dysplasia [9]. Marked left atrial dilatation is associated with an increased incidence of atrial fibrillation.
Depending on the findings of the echocardiography and rhythm diagnostics, further clarifications (cardiac MRI, ischemia diagnostics, left heart catheterization, electrophysiological examination, etc.) are necessary. Optimally, after the extended diagnostics, a diagnosis can be confirmed and a specific therapy can be initiated. Otherwise, a decision should at least be made as to whether an expansive approach is justifiable on the basis of risk stratification.
Therapy
Triggering factors, treatable structural heart disease (e.g., CHD), or systemic disease should be addressed directly. If arrhythmias are documented, the most targeted medical or catheter therapy possible should be performed (e.g., electrophysiologic study and slow pathway ablation for classic AV nodal reentry tachycardia). If necessary, pacemakers, implantable cardioverter defibrillators (ICD) or cardiac resynchronization therapy (CRT) devices are also used.
Cardiovascular risk factors (hypertension, diabetes, obesity, nicotine, etc.) should be consistently treated, as they are known to adversely affect the prognosis of patients and, as in the case of atrial fibrillation, may also maintain the arrhythmia. A detailed overview of the specific treatment of the different arrhythmias is not possible here, but can be found in recent guidelines, for example those of the ESC (European Society of Cardiology) [10,11].
Summary
Palpitations are a common symptom in the general population and usually of harmless etiology. A targeted history taking together with the clinical examination and the resting ECG allow to decide which patients should be submitted to an extended diagnostic procedure and in which patients an exspective procedure may be chosen.
The basis of advanced diagnosis of palpitations is the elucidation of symptom-rhythm correlations by means of ECG devices, which should be selected according to the frequency, duration, and clinic of palpitations. Echocardiography completes the diagnosis and answers the question about the structural cardiac findings. Further examinations such as cardiac MRI, non-invasive or invasive ischemia diagnostics or electrophysiological examinations are used in a targeted manner.
Take-Home Messages
- Palpitations are uncomfortably experienced, increased, accelerated, or irregular cardiac actions and overall are a common cardiac symptom.
- Pathophysiologically, there are three main causes: Arrhythmias, structural heart disease, and altered subjective perception of the heartbeat.
- In the majority of patients, the cause is benign.
- A targeted anamnesis together with the clinical examination and the resting ECG form the basic diagnostics.
- The basis of advanced diagnostics is the clarification of symptom-rhythm correlations using ECG devices, supplemented by echocardiography.
- Therapy depends on the underlying disease and ranges from medication to surgical therapies, including the
- Treatment with pacemaker devices. Modification of cardiovascular risk factors should also be included.
Literature:
- Abbott AV, et al: Diagnostic approach to palpitations. Am Fam Physician 2005; 71: 743-750.
- www.pschyrembel.de
- Weber BE, et al: Evaluations and outcomes of patients with palpitations. Am J Med 1996; 100: 138-148
- Raviele, et al: Management of patients with palpitations; Europace 2011; 13: 920-934.
- Lessmeier, et a.: Unrecognized paroxysmal supraventricular tachycardia. Potential for misdiagnosis as panic disorder. Arch Intern Med 1997; 157: 537-543.
- Thavendiranathan, et al: Does this patient with palpitations have a cardiac arrhythmia? JAMA 2009; 302: 2135-2143.
- Ioannou, et al: Ambulatory electrocardiography. BC Medical Journal 2014; 56: 86-89
- Steinberg, et al: ISHNE-HRS expert consensus statement on ambulatory ECG and external cardiac monitoring/telemetry. Heart Rhythm 2017; 14(7): e55-e96.
- Harris P, Lysitsas D.: Ventricular arrhythmias and sudden cardiac death. BJA Educ 2016; 16(7): 221-229.
- Katritsis, et al: EHRA consensus statement on the management of supraventricular arrhythmias. Europace 2017; 19: 465-511.
- Priori, et al: ESC Guidelines for the management of patients with ventricular arrhythmias. EHJ 2015; 36: 2793-2867.
CARDIOVASC 2017; 16(4): 3-7











