Reports on the abuse of loperamide for the purpose of euphoria or as a substitute for methadone have recently increased. Misuse can lead to dysregulation of the heart muscle cells, which often manifests itself as ventricular arrhythmias. Due to the μ-agonism of loperamide, supratherapeutic doses are also suspected of inducing sphincter Oddi dysfunction and a predisposition to pancreatitis.
Loperamide abuse reflects the progression of the opioid epidemic in the U.S., most commonly manifested by cardiac complications. Some opiates have been shown to increase basal sphincter of Oddi pressure, and abnormal pancreatic sphincter of Oddi manometry has been shown to be a risk factor for recurrent acute pancreatitis. Mild pancreatitis usually heals spontaneously, while severe pancreatitis is characterized by organ failure and often requires admission to an intensive care unit.
A 32-year-old man with acute abdominal pain, fatigue and weakness and an extensive history of gastroduodenal ulceration and fluctuating abdominal pain for four months presented to the team of Dr. Christopher A. Bouvette, Department of Medicine, University of Oklahoma College of Medicine, Oklahoma City [1]. Six years earlier, the patient had undergone several emergency laparotomies and an antrectomy with a Roux-en-Y gastrojejunostomy due to penetrating duodenal ulcerations associated with the use of non-steroidal anti-inflammatory drugs. The patient stated that he had not had any recent abdominal trauma or instrumentation. His only active medication was omeprazole and paracetamol as required. He also denied the consumption of alcohol, tobacco or illegal drugs.
On arrival, the patient was free of fever and had normal blood pressure, his heart rate was between 45 and 55 beats per minute, the authors write. An electrocardiogram revealed transient episodes of asymptomatic bradycardia with a corrected QT interval of 577 milliseconds. Physical examination revealed postoperative scarring along the midline of the abdomen. Palpation of the epigastrium was associated with significant tenderness without rebound.
High-grade pancreatic duct leak developed
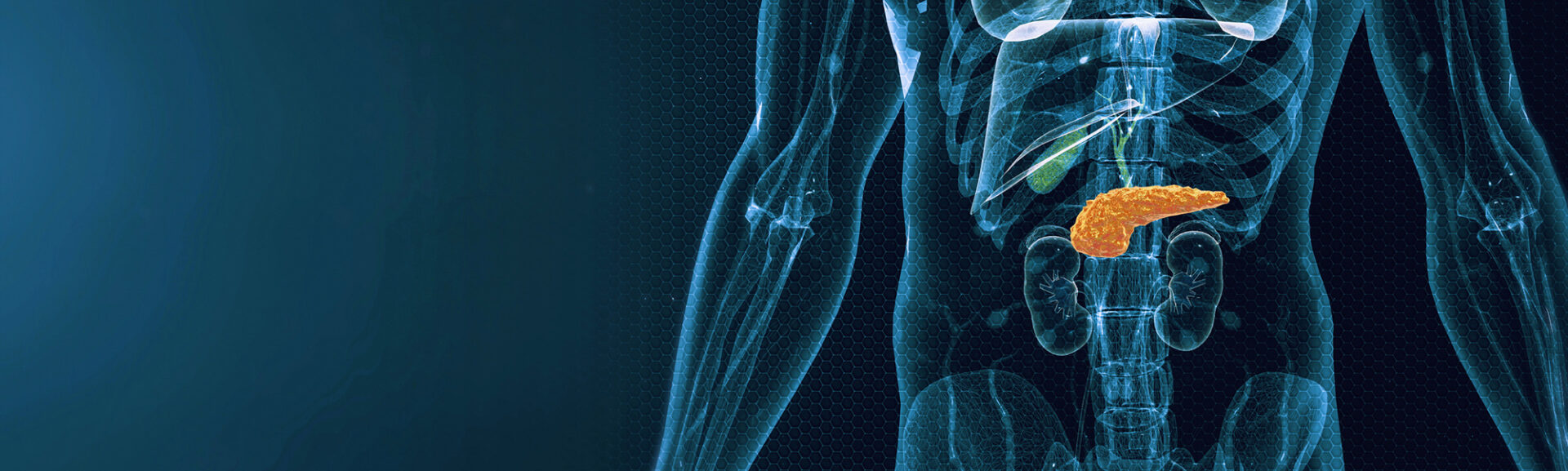
On admission, the laboratory values were significant for leukocytes (19 ×109 cells/l), hemoglobin (7 g/dl), platelets (700 ×109 cells/l), sodium (135 mmol/l), creatinine (0.77 mg/dl), total bilirubin (0.3 mg/dl) and triglyceride (110 mg/dl), among others. A urine drug screen revealed a negative result. Computed tomography of the abdomen and pelvis revealed severe constipation, acute pancreatitis, localized peripancreatic/perigastric/left-sided retroperitoneal fluid collections and severe splenic vein compression with splenomegaly (Fig. 1).
The patient received supportive intravenous fluids and opioid analgesia to treat the pancreatitis. Piperacillin-tazobactam was administered due to the localized abdominal fluid collections, leukocytosis and suspected intra-abdominal infection. The extent of the abdominal fluid collections and the development of a marked left pleural effusion raised concern about a possible pancreatic leak. Analysis of the pleural fluid revealed elevated amylase and lipase levels, which confirmed this.
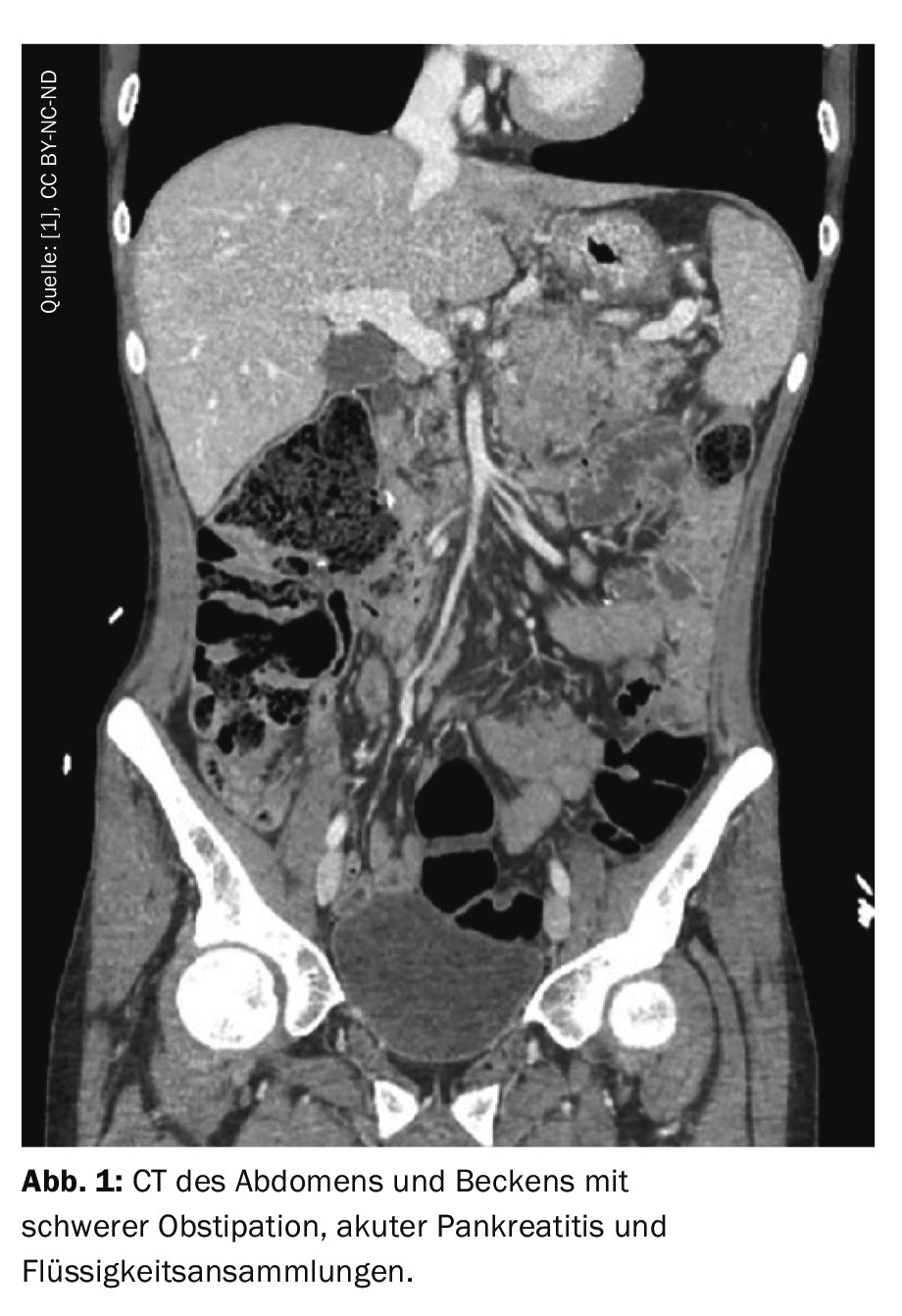
The patient’s hemodynamic instability prompted the doctors to transfer him to the intensive care unit, where he was found to be in septic shock associated with Escherichia coli bacteremia. After stabilization, endoscopic retrograde pancreatography was used to rule out calculus/impaction. Instead, a high-grade pancreatic duct leak was found at the level of the body-tail junction, for which an 11 cm long 7-French stent was inserted into the ventral pancreatic duct (Fig. 2).
150 tablets of loperamide daily
After endoscopic retrograde pancreatography, the patient’s clinical condition improved. The autoimmune pancreatitis panel (IgG4) and the genetic panel (CFTR, SPINK1, PRSS1 and CTRC) were sent in and were within the normal range.
Only in the course of further medical questioning did the patient finally admit that he had taken up to 150 tablets of loperamide 2 mg per day in the last six months. It has been suggested that these prolonged supratherapeutic doses of loperamide may have caused sphincter Oddi dysfunction and resultant pancreatitis. After his condition stabilized, the patient was discharged to an inpatient substance abuse rehabilitation center.
Loperamide is a gastrointestinal μ-opioid receptor agonist. At a dose of 16 mg (maximum daily dose) or less, it is actively removed from the central nervous system (CNS) by a P-glycoprotein (P-gp) membrane transporter-dependent mechanism. The main metabolite, desmethyl-loperamide, is of interest because in high concentrations it acts both as a P-gp substrate and as an inhibitor. This is typically the case with doses of 70 to 200 mg daily, Dr. Bouvette and his colleagues write. P-gp inhibition enables the accumulation of loperamide in the CNS. This is where the potential for abuse lies.
Opioids alter the biomechanics of the sphincter Oddi. In the absence of a plausible alternative cause, the authors suggest that long-term use of loperamide at supratherapeutic doses may have caused sphincter of Oddi dysfunction and associated pancreatitis. “In view of the variable opioid-specific effects on the sphincter Oddi, it is not possible for us to prove a causal relationship,” the authors explain. In addition, physicians should be more suspicious of loperamide abuse in patients with a clinical picture of opioid abuse, signs of ventricular dysregulation, and now possibly pancreatitis.
Literature:
- Bouvette CA, Nasir AB, Grossen AM, et al: Loperamide Misuse Presenting With Pancreatitis. AIM ClinicalCases 2024; doi: 10.7326/aimcc.2023.0874.
GASTROENTEROLOGY PRACTICE 2024; 2(1): 18-19