In addition to chlamydia and gonococci, there are numerous pathogens that can cause urethritis. Occasionally, clinical features may indicate the responsible germ, such as marked painfulness and meatitis in adeno- and herpesviruses or concomitant balanoposthitis in Mycoplasma genitalium. Microscopic diagnosis of fluorine allows differentiation of gonorrhea from NGU, enables immediate therapy, and may additionally provide evidence for viral urethritis. Especially in chronic or recurrent forms, a broad pathogen clarification should be performed, taking into account Mycoplasma genitalium and Trichomonas vaginalis. Prolonged azithromycin should be used in cases of treatment failure on standard therapy (especially M. genitalium and U. urealyticum).
After exclusion of a urinary tract infection, a distinction must be made between a non-infectious and an infectious form of urethritis (tab. 1) . Typical causes of non-infectious urethritis are mechanical-traumatic triggers; chemical (e.g. disinfectants, soaps) or local causes such as congenital anomalies, phimosis, neoplasia may also be accompanied by non-infectious urethritis. Traditionally, infectious urethritis is divided into two groups: Gonococcal urethritis (GU) and so-called non-gonorrheic urethritis (NGU). This classification arose historically to distinguish NGU-a group of infections of similar symptomatology with, at the time, unclear, heterogeneous, and difficult-to-determine etiology-from the much better-studied and more serious gonorrheic urethritis. NGU, formerly also called nonspecific urethritis, was comparatively rare along with gonorrhea, but now far exceeds its incidence and is not infrequently asymptomatic. In the following, however, only non-gonorrheal infectious urethritis and its pathogen spectrum, the necessary clarification steps and therapeutic measures will be discussed.
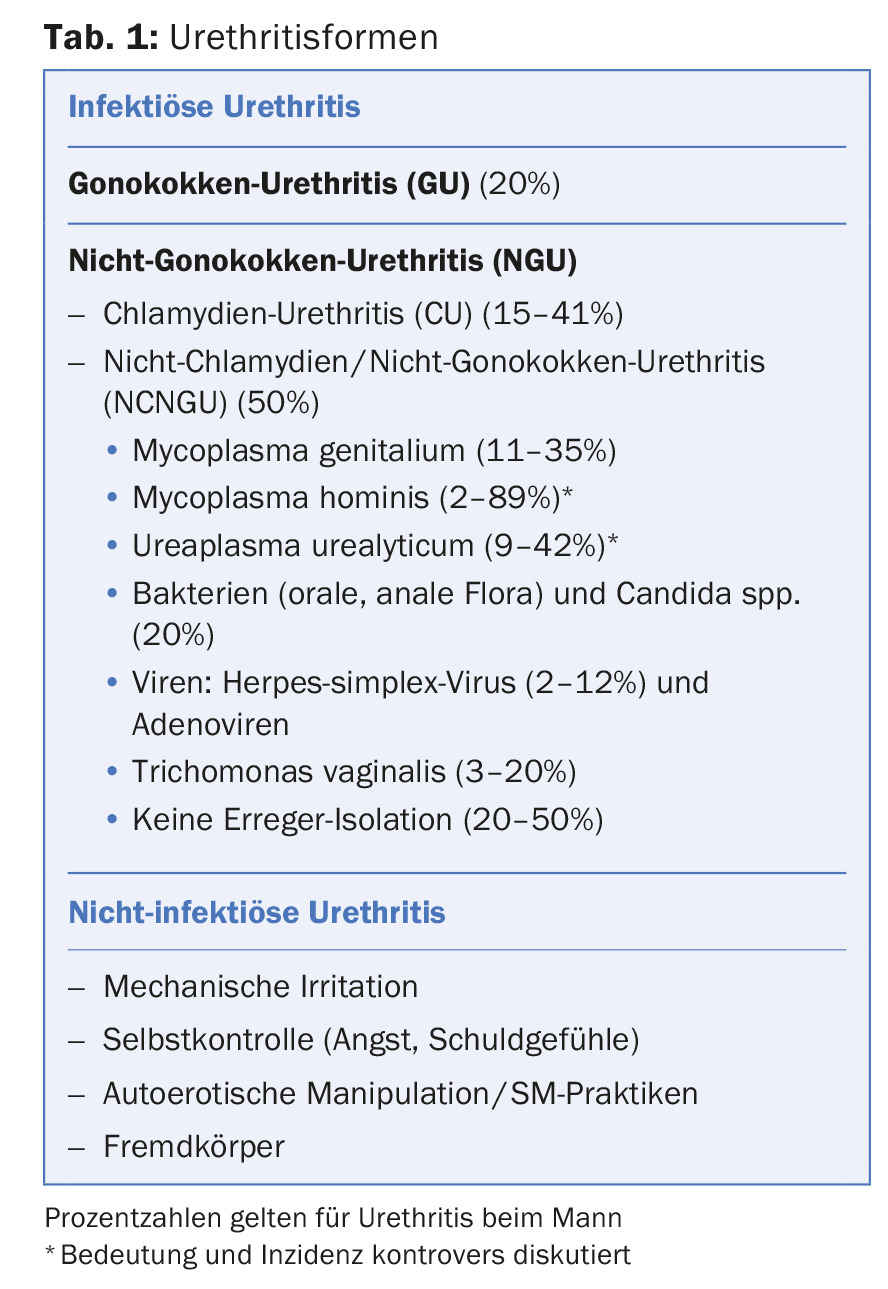
The prevalence of the causative pathogen spectrum is reported differently according to region (tab. 1). The proportion of patients in whom no pathogen could be isolated depends on the diagnostics performed and on the fact that, for example, viral urethritides are more common than previously assumed but are rarely sought. NGU is present when the stained smear preparation from the urethra contains more than five polymorphonuclear leukocytes
per field of view (total magnification 400x) in the absence of intracellular diplococci.
Chlamydia
Chlamydia trachomatis comprises a total of 15 serotypes defined by different protein antigens, designated by the letters A-C, D-K, and L1-L3, which cause different diseases. Serovars D-K are causative for urethritis, cervicitis, endometritis, and salpingitis. The pathogens do not infect squamous epithelium but exclusively cylindrical epithelium and have a prevalence of 4-5% in women in Europe.
C. trachomatis is found in 15-41% of all urethritis cases in men. However, in the literature of the last decade, the frequency of chlamydia as a causative agent is not consistently reported. Transmission occurs during sexually unprotected contact, with age under 20 years, promiscuity, and lack of or improper condom use as risk factors. Annual screening for sexually active patients younger than 25 years is recommended as well as for women older than 25 years with risk factors (multiple partners, new partners). However, genital chlamydial infections affect all social groups equally.
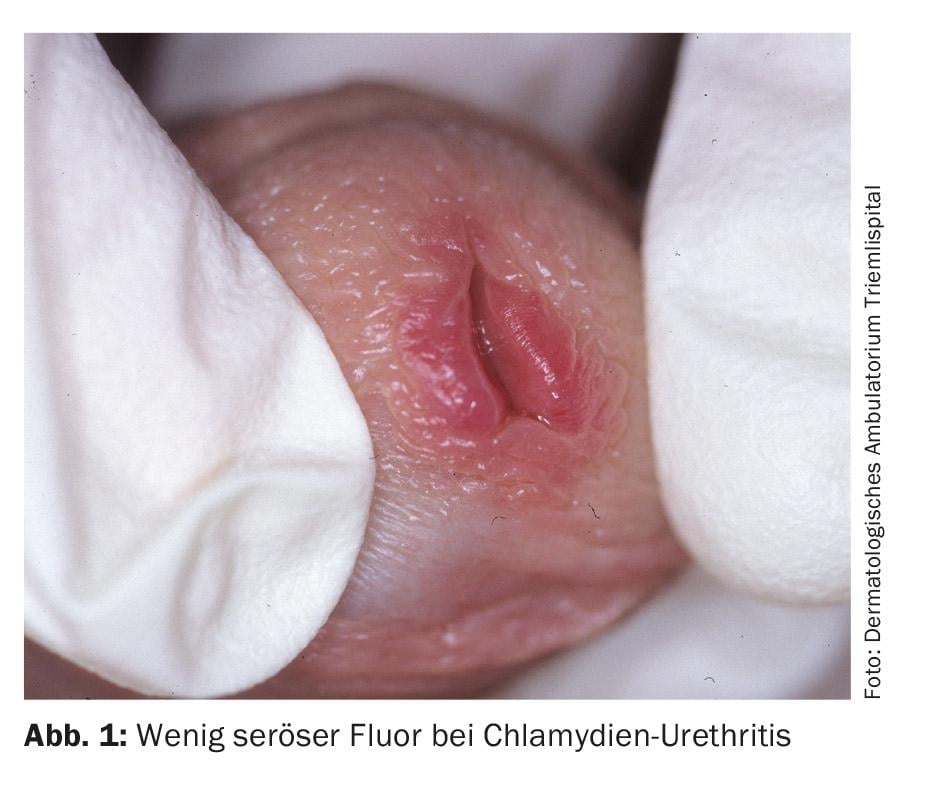
Chlamydia infection in men becomes noticeable after an incubation period of seven days to three weeks with serous discharge. Additionally, burning sensation and alguria are indicated. On examination, apart from a discrete reddening of the orificium urethrae and adhesion of the urethral orifice, there are usually no other findings (Fig. 1) . In 30-50% of all infected men, the infection is asymptomatic. The most common site of chlamydial infection in women is the cervix, and the infection is asymptomatic in up to 70%. If left untreated, genital chlamydial infection persists in women for an average of two years. This chronic asymptomatic infection appears to be the main cause of bilateral tubal occlusion, which is the most common cause of infertility in women and is estimated to affect over 100,000 women in Germany. The clinically manifestations are whitish-yellowish genital discharge with itching and burning at the vaginal introitus. Pharyngeal infections not infrequently appear to be asymptomatic in addition, but do not require different therapy.
Diagnosis: In women, the pathogens are detected by smear tests of the cervix or vagina or urine analyses (somewhat less sensitive) using PCR. In men, a urine examination or a smear from the urethra may also be performed.
Due to their small size and low affinity for dye, chlamydiae cannot be seen natively or by staining. As obligate intracellular bacteria, cultivation is also difficult, which is why culture is rarely performed anymore.
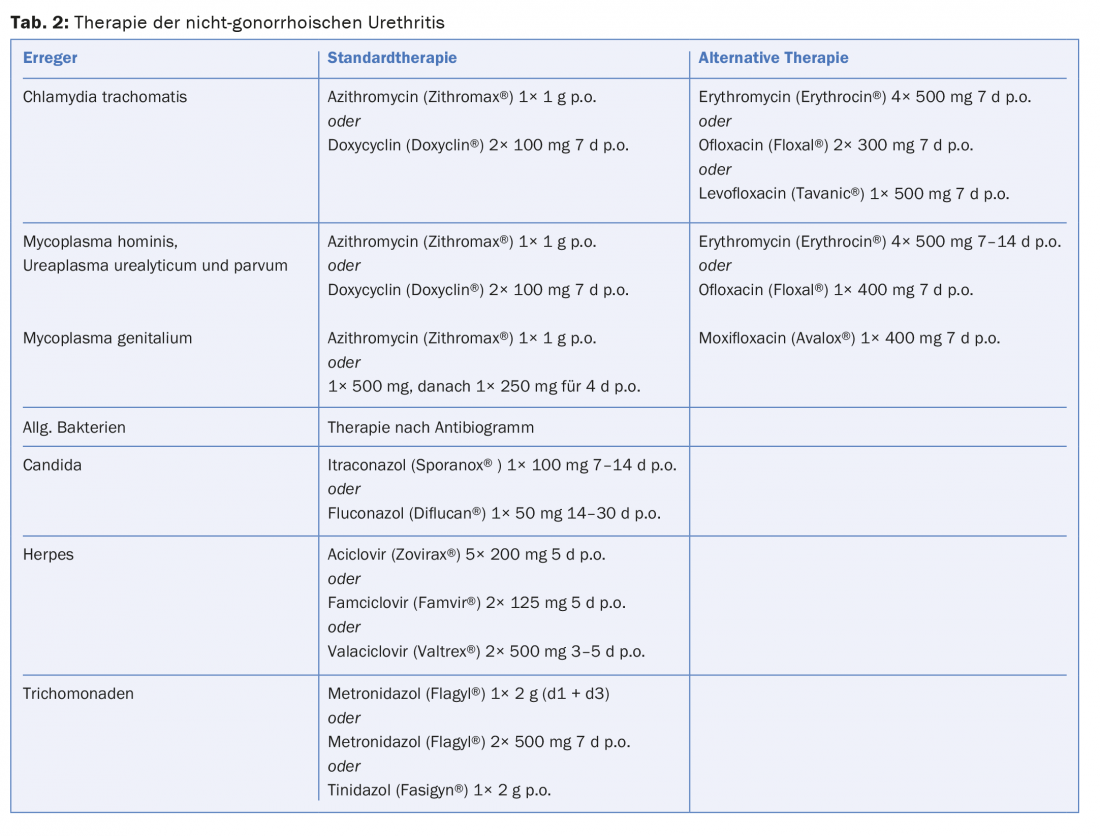
Therapy: uncomplicated urogenital infections can be treated with doxycycline 2× 100 mg for seven days or azithromycin 1 g once. The efficacy of the two antibiotics is nearly equivalent with slightly better response to doxycycline but better compliance under azithromycin. As recently documented, NGU healing rates appear to be somewhat declining with these standard therapies, but switching to other medications is not recommended. Based on current data, azithromycin, like erythromycin, can be considered safe in pregnancy. Alternatively, amoxycillin can be administered 3× 500 mg/d for seven days during pregnancy.
Mycoplasma
Mycoplasmas are immobile gram-negative bacteria. They differ from other bacteria in their small cell size, small genome, and lack of cell wall. On special culture media, ureaplasmas (Ureaplasma urealyticum) and non-ureaplasma mycoplasmas (Mycoplasma hominis) can be distinguished. Subsequently, U. urealyticum was divided into Biovar 1 and Biovar 2. In 1999, Biovar 1 was classified as a new independent bacterial species under the name U. parvum, while Biovar 2 was designated U. urealyticum. In 1981, another variant – Mycoplasma genitalium – was discovered, which was subsequently described in several studies as the causative agent of acute urethritis and increasingly also as the causative agent of chronic urethritis, but also cervicitis, endometritis and in female infertility.
The significance of genital mycoplasmas for the development of sexually transmitted diseases is controversial. M. hominis does not appear to be responsible for NGU in males, despite detection in the genitourinary tract. U. urealyticum (Biovar 2) can also be frequently isolated from the genital tract of healthy women and men; possible clinical manifestations have been postulated in younger patients, high bacterial concentration, specific serotype Biovar 2, and initial infection. The significance of U. parvum remains unclear.
Mycoplasma infections can cause clinical symptoms of urethritis in men in addition to silent courses. In particular, U. urealyticum and M. genitalium infections manifest themselves in the form of acute, but also chronic urethritis with dysuria and fluoride. A special clinical feature of urethritis caused by M. genitalium is the significantly frequent association with balanitis and/or posthitis, which is not observed with chlamydia and ureaplasma.
Diagnostics: Due to their size and low affinity for dyes, detection of mycoplasmas in Gram preparations is not possible. U. urealyticum, U. parvum and M. hominis are detected by PCR or culture, M. genitalium exclusively by PCR. Serological tests are of no importance for the diagnosis of infections with mycoplasmas in clinical routine.
Therapy: Tetracyclines, macrolide antibiotics and quinolones are the drugs of choice. Doxycycline 2× 100 mg/d for seven days or azithromycin 1× 1 g are considered standard therapy for M. hominis, U. parvum, and U. urealyticum. (Tab.2). In chronic forms of urethritis, a longer duration of therapy may be necessary. Azithromycin is recommended for the treatment of genital urethritis because its effect is clearly superior to that of tetracyclines. Increasingly, treatment failures have been observed recently, which is why, in the event of a non-response of 1 g azithromycin a treatment lasting several days is favored (Tab.2). Moxifloxacin is considered the absolute reserve drug; however, initial treatment failures have also recently been described in macrolide and quinolone resistance. With an increase in resistance, the place of other drugs such as sitafloxacin or gatifloxacin must be further investigated to avert the threat of untreatability of M. genitalis.
Bacteria of the oral and anal flora
Urethritides can be caused by numerous other bacteria. Staphylococcus aureus can result in urethritis, cystitis, or prostatitis, especially in patients with urethral catheters. Streptococci and especially enterococci can also lead to urethritis. E. coli can rarely cause urethritis, cystitis, prostatitis or epididymitis, and pyelonephritis in men after anal intercourse. Rarely, a Pseudomonas infection may also present with urethritis.
Pathogens of the oral flora such as Haemophilus influenzae and parainfluenzae, but also meningococci, can not infrequently be causative, especially since oral sex is nowadays regarded by many as supposedly unproblematic with regard to the transmission of infections and accordingly few condoms are used during oral sex. The actual prevalence of urethritides caused by Haemophilus is unknown because, on the one hand, there is no obligation to report and, on the other hand, the pathogen is usually not included in the work-up.
Diagnosis: Bacteriological detection of the pathogen by means of culture should always be sought to establish the diagnosis.
Therapy: Therapy depends on the pathogen and antibiogram.
Candida
Candida albicans can lead to urethritis secondary to balanitis or vulvovaginitis, especially in the presence of diabetes mellitus or immunodeficiency.
Diagnosis: Detection is performed in the direct preparation and by mycological culture.
Therapy: Imidazole derivatives such as itraconazole 100 mg/d for 7-14 days or fluconazole 50 mg/d for 14-30 days are used for therapy (Table 2).
Viruses
Viral urethritis must be suspected if the bacteriological clarifications were unproductive. In herpes simplex virus (HSV) urethritis, a painful serous discharge is found, often accompanied by herpetiform eruptions on the external genitalia. Less commonly, HSV infection occurs exclusively intraurethrally (Fig. 2).

In recent studies, HSV type 1 has been shown to cause NGU more frequently than HSV type 2. The proportion of HSV in NGU is variably reported but accounted for up to 12% in one study. Adenoviruses can also cause urethritis. This is usually characterized by marked meatitis and pain (Fig. 3); the majority are also accompanied by highly contagious conjunctivitis (Fig. 4) . Heaps of mononuclear cells in the direct preparation can be diagnostically groundbreaking. Especially after unprotected oral contact, adeno- and herpes simplex viruses must be considered as the cause in the absence of pathogen detection, pronounced painfulness and meatitis. Epstein-Barr viruses also appear to be important.

Diagnostics: In the case of herpes infections, smear examination is a good option. Cultural detection of HSV requires about 48 h. Viruses can only be obtained from fresh lesions for culturing. By PCR, the smear material can be analyzed within a few hours. Both culture and PCR can also be performed from urine. Antigen detection by immunofluorescence is also suitable for diagnosis. Detection of adenoviruses by PCR can be done by smear or from urine.
Therapy: Therapy of herpetic urethritis is performed with nucleoside analogues if required.
Trichomonads
Trichomonas vaginalis is a flagellate of oval shape with four flagella and an undulating membrane. Trichomoniasis is a sexually transmitted infection that occurs worldwide and its prevalence depends on sexual risk behavior. In statistics, there are significant differences in infection rates between individual population groups and between developed and developing countries. In Switzerland, for example, this infection plays a minor role in contrast to Seattle, where up to 20% of NGU cases in men are caused by this pathogen.
Diagnosis: Microscopic examination of the native preparation with 0.9% NaCl from the vaginal vault, cervix and urethra yields hit rates of up to 75%. Polarization or dark-field microscopy increase the hit rate.
A range of suitable culture media with a sensitivity of about 95% is available. The culture is offered in very few laboratories. PCR, which has the highest sensitivity, is also still not widely used.
Therapy: trichomoniasis can be treated with metronidazole 1× 2 g with possible repetition after two days or with 2× 500 mg/d for seven days, but the antabuse-like effect should be noted. Rarely, resistance to metronidazole can be observed. Furthermore, tinidazole 1× 2 g is a therapeutic option. Tinidazole has a longer half-life, fewer side effects, and a slightly higher cure rate.
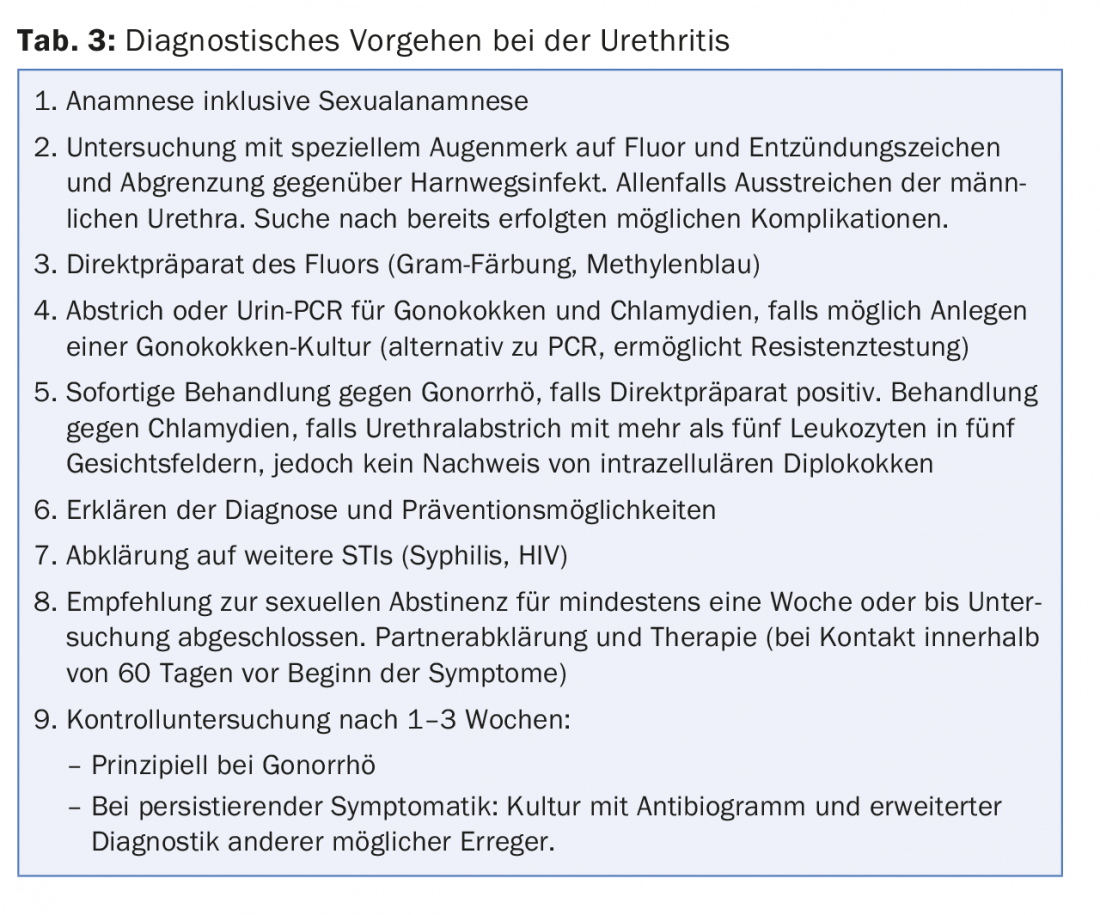
An example of a possible approach to urethritis is listed in Table 3.
Literature by the author
DERMATOLOGIE PRAXIS 2015; 25(4): 5-10