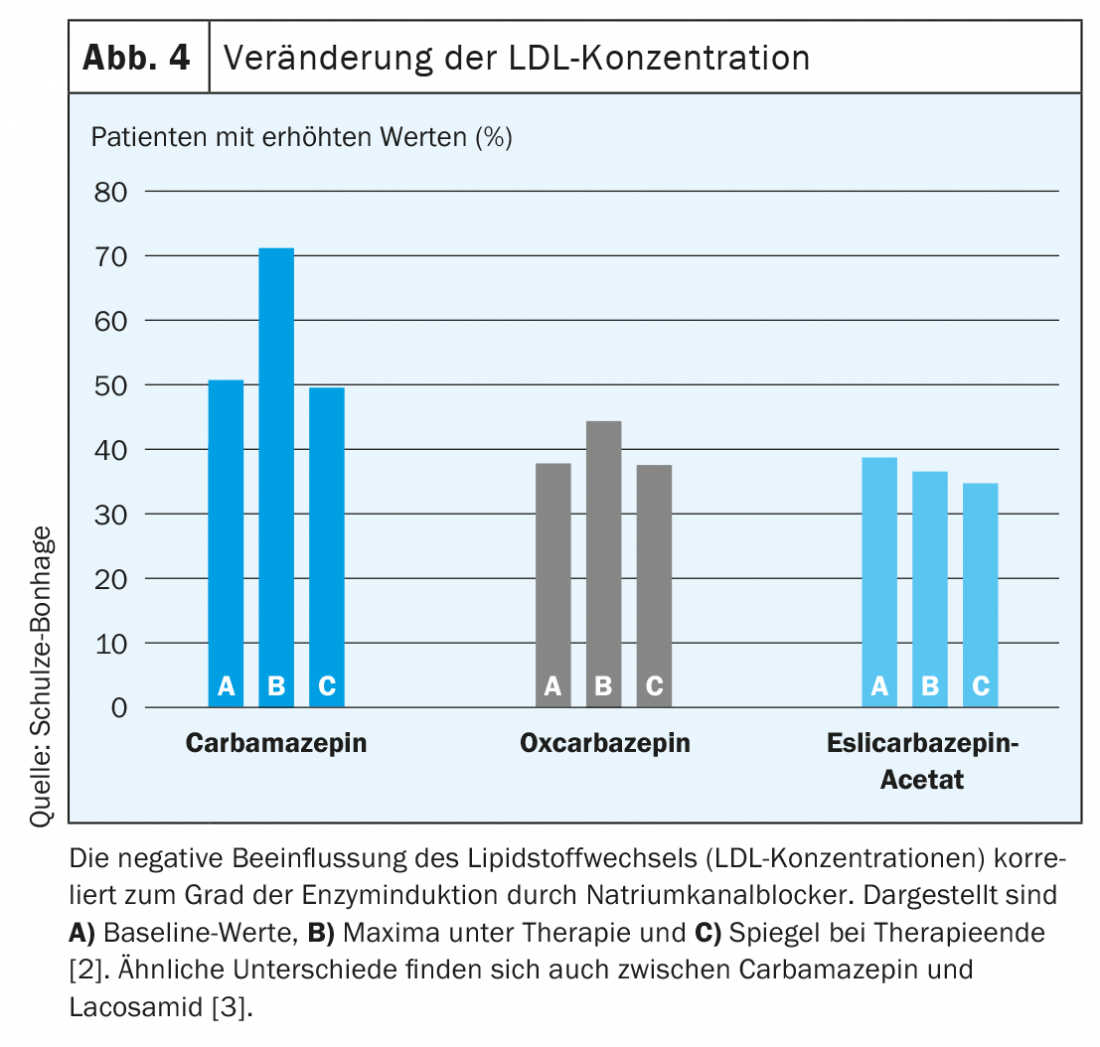
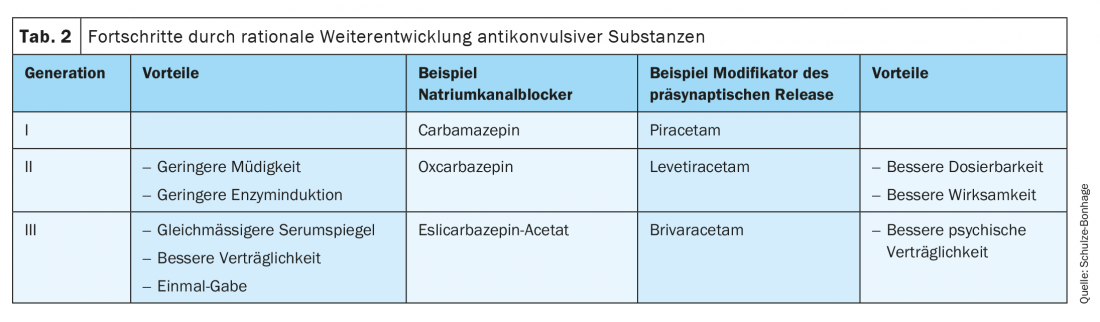
The arsenal of available pharmacotherapies for the treatment of epilepsy has expanded dramatically in recent years. More targeted selection and prioritization based on the form of epilepsy, consideration of comorbidities, and incorporation of individual patient characteristics is now possible. Lack of or weak enzyme induction in second- and third-generation antiepileptic drugs avoids previously typical antiepileptic drug side effects such as osteoporosis, polyneuropathies, and metabolic syndromes.
Since 1990, more than 20 drugs have become newly available for the prophylaxis of epileptic seizures. These differ not only in their mode of action but also in terms of their dosage, propensity to interact, and typical side effects. On the one hand, their targeted use requires more knowledge on the part of the user; on the other hand, however, it enables an increasingly individual patient-oriented selection. In the present article, with reference to patient groups depending on age, sex, and comorbidities, guidance is given for appropriate selection of antiepileptic drugs.
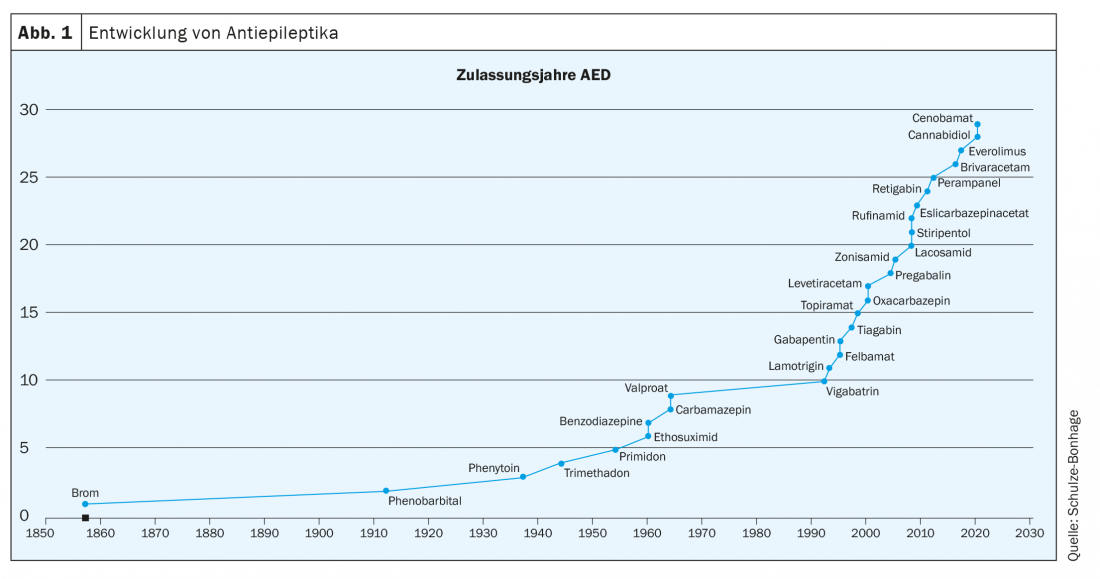
Since the introduction of second-generation antiepileptic drugs in the past 30 years, the arsenal of available phamacotherapies for epilepsy treatment has expanded enormously (Fig. 1). While this expansion has not yet solved the problem of phamacoresistance in approximately one-third of epilepsy patients, it does allow for more targeted selection and prioritization based on the form of epilepsy, consideration of comorbidities, and incorporation of individual patient characteristics, such as gender, age, and occupational demands (Table 1).

Epilepsy syndromes and anticonvulsive therapy.
The main groups of epilepsies treated in adulthood include structural epilepsies with focal (or multifocal) seizure onset on the one hand, and presumed genetic epilepsies with generalized, i.e., early onset involving both hemispheres, on the other. More than 60% of adult epilepsies are classified as focal, and the proportion of patients with incomplete seizure control is more than 40% in this group. Accordingly, the majority of new antiepileptic drug developments were made with the indication of treating focal epilepsies and their seizures.
New developments in the last decade for the treatment of focal epilepsies include brivaracetam, eslicarbazepine acetate, perampanel, lacosamide, and most recently cenobamate*. Brivaracetam and eslicarbazepine acetate are third-generation antiepileptic drugs that have been rationally developed from predecessor compounds. Brivaracetam is a third-generation derivative of piracetam and levetiracetam, with higher specific efficacy at the point of onset and improved tolerability, particularly with regard to psychiatric side effects. Eslicarbazepine acetate, as a pro-drug, is a further development of carbamazepine and oxcarbazepine with a more selective use of an enantiomer and significantly improved pharmacokinetics, allowing a single dose without disruptive plasma peaks. Lacosamide also has a modified mode of action at sodium channels and thus joins the group of sodium channel blockers with a particularly low interaction potential. Perampanel is a new development with a target at glutamate subreceptors and thus expands the spectrum of available approaches. Finally, cenobamate combines two mechanisms of action (sodium channel blockade and enhancement of GABA-ergic inhibition) in one substance (tab. 2).
* currently not yet approved in Switzerland
How can this multitude of antiepileptic drugs be used profitably in the individual patient?
In some countries, in addition to proof of efficacy in pre-specified placebo-controlled trials, superiority in head-to-head comparisons is required for attestation of additional benefit. However, such studies do not meet the international requirements for pivotal studies and are therefore mostly not available; results of direct comparisons also depend considerably on selected study parameters (dosing rate, target doses), at least for short studies.
The main comparative information on the efficacy and tolerability of monotherapies comes from SANAD studies conducted in the United Kingdom (Tab. 3). Here, after randomization of the treatment substance but open treatment with margins in the dosage, the retention rate over periods of years was recorded as a practice-relevant outcome parameter – the retention rate captures aspects of both efficacy and adequate long-term tolerability.
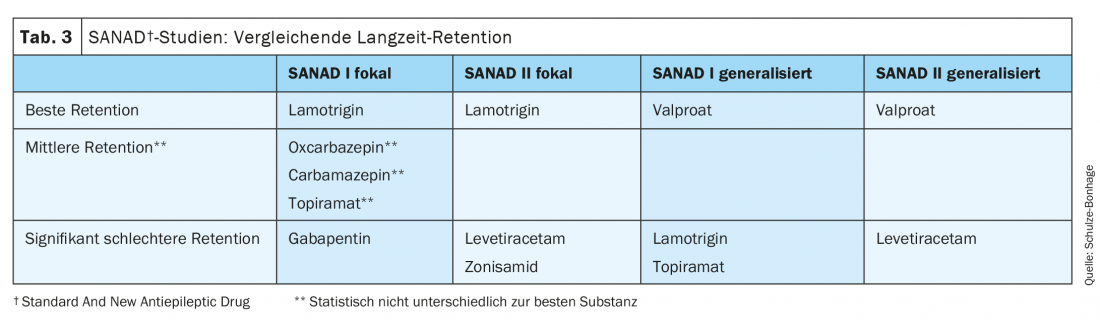
The first SANAD study was the first to demonstrate the superiority of lamotrigine and the inferiority of gabapentin in a large collective with a selection corresponding to clinical practice; oxcarbazepine also performed well here, topiramate rather worse. In the recently published SANAD-II study, lamotrigine had to compete with levetiracetam and zonisamide. Here, too, lamotrigine performed best, largely due to its often very good tolerability; in comparison, the often favored levetiracetam, in particular, exhibited psychiatric side effects such as depression and irritability much more frequently. Overall, therefore, there are good reasons to consider lamotrigine and oxcarbazepine for monotherapy of focal epilepsies.
Treatments of generalized epilepsies differ in their effectiveness
While the differences in efficacy in the treatment of focal epilepsies are gradual and other aspects usually play the major role in drug selection, there is a clear hierarchy of efficacy in generalized epilepsies: Valproate was shown to be clearly superior to lamotrigine, levetiracetam and topiramate in a large number of studies, including both SANAD studies. Only in absence treatment can ethosuximide be considered equally effective.
However, the example of valproate shows particularly clearly that efficacy is only one criterion for the individual choice of medication. This is because side effects of valproate are diverse and relevant to the patients being treated. These adverse effects include persistent weight gain often exceeding 5 kg, metabolic syndrome, polycystic ovary syndrome, thrombocytopenia, encephalopathy, coagulopathy/coagulopathy, osteopathy, hair loss, a tremor, furthermore significantly increased risk of teratogenicity and risk of intelligence reduction with exposure during pregnancy. Many of these risks are not evident at all in the results of short-duration studies, such as common three-month studies, and are barely evident in the outcome parameters even in studies lasting a year or more. Notwithstanding the study evidence of a clear preference for valproate, at least in women of childbearing age, based on the risks and side effects, valproate is chosen only as a drug of last choice when the other available options fail.
Individualized selection of antiepileptic drugs
Therefore, the consideration of the individuality of the patient takes the place of a scheme of a general therapy sequence. Important aspects for the choice of medication include age, gender, seizure situation and compliance (Fig. 2).
The role of etiology
The etiology of epilepsy is a major factor in the chance of achieving complete seizure freedom. Thus, the risk of pharmacoresistance is particularly high in malformations of cortical development, especially cortical dysplasias or tuberosities, and in hippocampal sclerosis. Imaging therefore plays an essential role in early education about realistic treatment options and potentially useful early non-drug treatments such as epilepsy surgery.
In difficult-to-treat epilepsies, combination treatments using particularly potent antiepileptic drugs (such as topiramate, perampanel, or cenobamate) are more frequently required than, for example, in vascular epilepsies, in which monotherapies with antiepileptic drugs such as lamotrigine, eslicarbazepine acetate/oxcarbazepine, or pregabalin are often sufficient.
With the development of orphan drugs, epilepsy syndrome is coming into particular focus. For example, cannabidiol and fenfluramine have recently become available for Dravet syndrome and Lennox-Gastaut syndrome, and vigabatrin, cannabidiol, and everolimus have been shown to be effective for tuberous sclerosis. Everolimus is an example of a pioneering approach to influencing epileptogenesis in tuberous sclerosis with longer time windows to achieve full efficacy with a disease-specific approach to action for the first time.
Seizure situation
The degree to which a patient is acutely affected by the severity and frequency of seizures may play a significant role in the decision to dose an antiepileptic drug. Effective treatment can be achieved with the first dose of pregabalin, levetiracetam, and brivaracetam, within a week by many sodium channel blockers except lamotrigine; in contrast, lamotrigine, zonisamide, and cenobamate* require many weeks to months until effective concentrations are achieved in a tolerable manner.
* currently not yet approved in Switzerland
For high-frequency series, the availability of an intravenous form of administration may also be an advantage; however, oral up-dosing is usually sufficient. In particular, the aspect of an intravenous treatment option should not lead to the choice of a medication that is not actually preferred (such as phenytoin).
Dose regimen and compliance
Compliance in taking the prescribed medication regimen and long-term adherence of treated patients are of central importance for long-term treatment success. Favorable for regular intake are treatments with substances that need to be given only once a day (eslicarbazepine acetate, perampanel, cenobamate*, in my opinion also zonisamide or valproate), to be avoided if possible are three times daily intake protocols.
* currently not yet approved in Switzerland
Another key factor is that the treatment is well tolerated. In epilepsies responding well to low doses, this is often a minor problem, but with the need for higher doses and polytherapy, the selection of individually well-tolerated drugs and their appropriate combination becomes significant. Side effects are subjectively experienced in very different ways; taking the patient’s individual information seriously is crucial for cooperation between doctor and patient.
Complex dosing regimens (such as with lamotrigine) may overwhelm patients with low intelligence or memory impairment and result in failure to achieve planned target doses. A mutually accepted strategy is also of high importance for a coordinated gradual tapering of treatments.
In patients with known problems regarding medication adherence, medications with a long half-life (perampanel, m.E. zonisamide, eslicarbazepine acetate, and valproate) may offer advantages because a single missed dose results in less serum concentration fluctuation).
The role of age
According to all available data, antiepileptic drugs basically work at any age; thus, except for the last time, all drugs were also tested in adults and then successfully given to older patients and children. Accordingly, the FDA is also moving away from specific pivotal studies for the 4-18 age range.
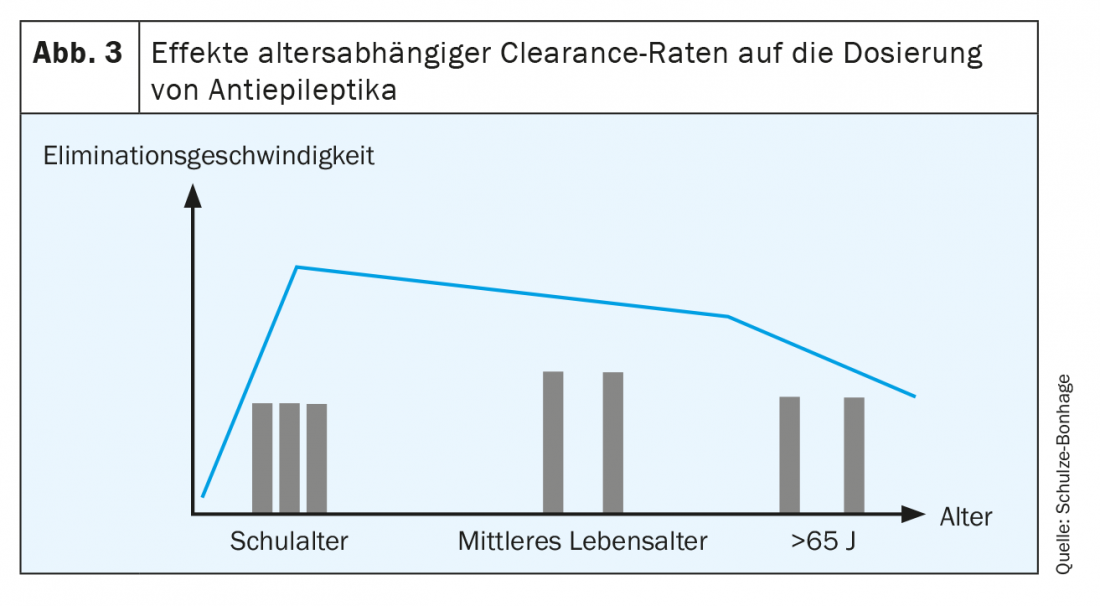
Nevertheless, age-related peculiarities must be taken into account:
- Especially prenatally and in the first year of life, the composition of neurotransmitter receptors may differ relevantly. For GABA receptors in particular, this is known to reverse the effects of GABA-ergic substances with possible proconvulsant effects.
- In the first months of life, hepatic elimination of many substances is delayed; this increases the risk of intoxication symptoms with drugs that are predominantly hepatically eliminated.
- In preschool and school-age children, on the other hand, renal elimination is more rapid than in adults; this requires the use of higher doses and, if necessary, more frequent administration of single doses to achieve the desired effect level.
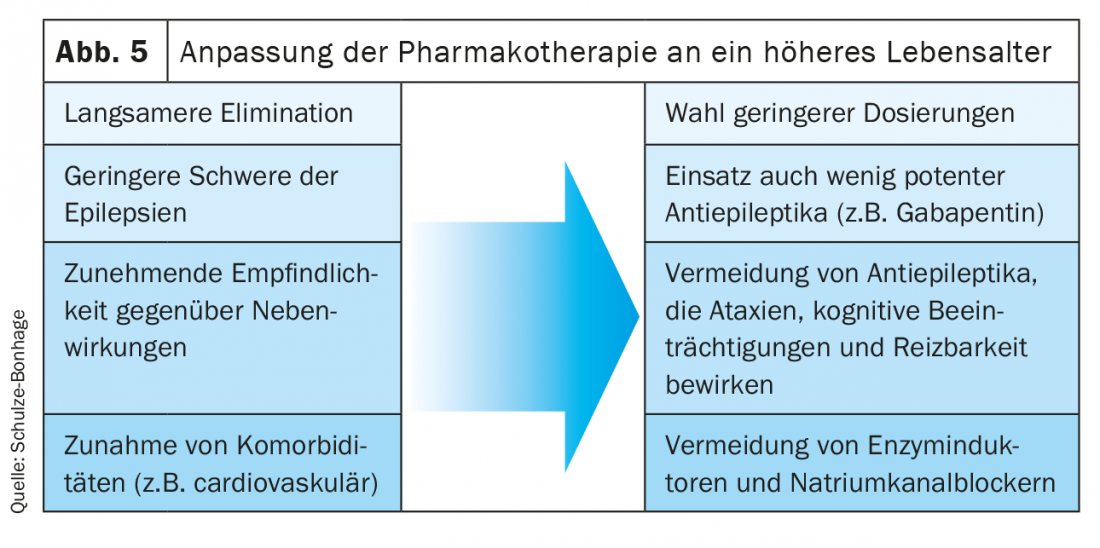
- In older age, renal elimination in particular decreases; this allows the use of lower doses or longer intervals between individual doses (Fig. 3).
- In older age, the risk of side effects increases, including those affecting bone metabolism. With a general predisposition to osteoporosis, potent enzyme inducers and valproate are associated with a substantially increased risk of fracture and should be avoided.
- In older age, tolerance for side effects decreases, especially of sodium channel blockers and of cognitively impairing drugs. Differences between treatments that have little effect in middle age become significant here, such as the poorer tolerability of carbamazepine compared with lamotrigine or gabapentin (Fig. 5) [1].
- Finally, the etiologic spectrum of epilepsies changes throughout life. For de novo epilepsies in older age, which now account for the majority of epilepsies, this means a good response to even less potent drugs such as gabapentin (Fig. 4).
Specific aspects in the treatment of women
All established anticonvulsants show comparable efficacy in men and women. However, there are differences in terms of willingness to tolerate certain side effects. In particular, drugs that frequently lead to weight gain (such as carbamazepine, vigabatrin, pregabalin, valproate) are more likely to be rejected by women than by men, as is hair loss during treatment with valproate or skin blemishes during lamotrigine. On the other hand, strong enzyme inducers often cause acutely disruptive impotence in men.
Women of childbearing age: with menarche, fluctuations in estrogen concentrations cause relevant effects on the pharmacokinetics of hepatically eliminated antiepileptic drugs; high estrogen levels lead to accelerated degradation of lamotrigine and oxcarbazepine in particular. Such fluctuations may enhance the intrinsic proconvulsant effects of estrogens and lead to cyclic increases in seizure frequency. Choosing antiepileptic drugs with less variation in serum concentrations may be beneficial in this setting.
Similar effects occur with conception protection by taking estrogen-containing ovulation inhibitors: at the doses chosen here, in addition to clinically relevant decreases in serum concentrations of lamotrigine, oxcarbazepine, and levetiracetam, there is also a separate proconvulsant effect. This repeatedly leads to recurrent seizures in young women who are prescribed estrogen-based contraceptive protection without adjustment of anticonvulsant medication, even after prolonged seizure control. Pure progestogen preparations (“mini-pill”) or intrauterine devices (“IUDs”) are preferable for conception protection.
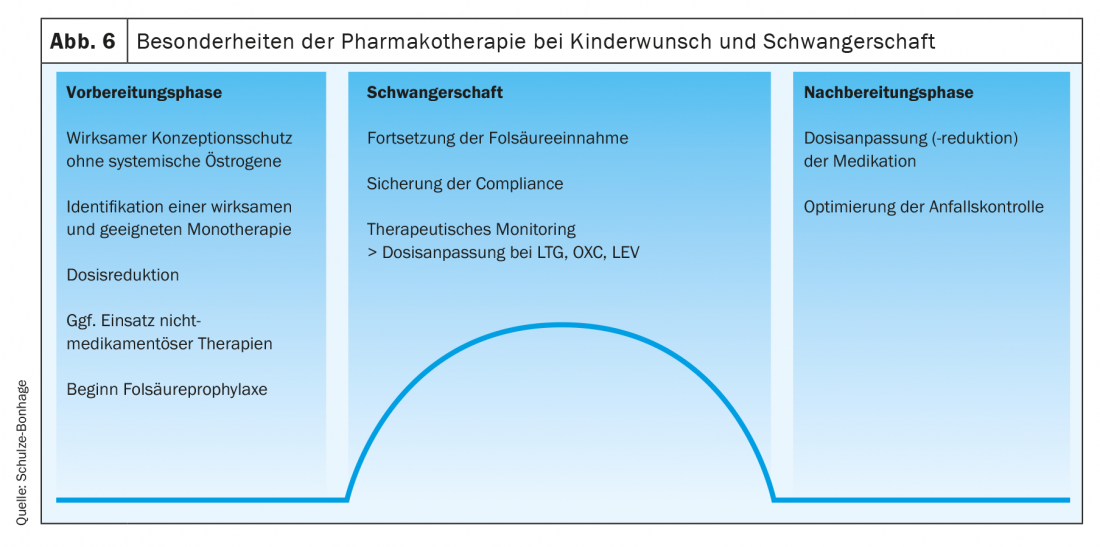
In the preparation and treatment during pregnancy, the aspect of minimizing the risk of teratogenicity comes to the fore. Folic acid prophylaxis, treatment in monotherapy, and preferential use of the minimum required doses of lamotrigine, levetiracetam, and oxcarbazepine while avoiding valproate are of high importance, especially for the embroygenesis phase. Peripartum, a slight increase in the dose of the basic medication or a temporary, low-dose additional administration of clobazam (5-10 mg) may help to reduce the risk of seizures.
Postpartum, anticonvulsant concentrations rise again during the first few weeks; despite the often disturbed nighttime sleep, an increase in dosage made during pregnancy can be gradually reversed. Anticonvulsant concentrations passing into breast milk are not dangerous with modern antiepileptic drugs and are no reason to refrain from breastfeeding the child (Fig. 6).
Women 45 years and older: During menopause, seizure control worsens in approximately one-quarter of epilepsy patients. At times, the risk of seizures increases, especially in women with a high sensitivity to fluctuations in sex hormones and a cycle dependence of seizure frequency (so-called catamenial epilepsies). Accordingly, intensification of treatment may become necessary; advantageously, the spectrum of applicable antiepileptic drugs can be fully exploited here.
With menopause comes an increased risk of developing osteoporosis, which may be increased by anticonvulsants and is a particular risk in seizures with falls. Hormone replacement therapy, which is effective for prophylaxis, increases the risk of seizures due to the estrogens it contains; accordingly, higher doses of anticonvulsant therapy may be required.
However, fracture incidence increases substantially, particularly with the use of strong enzyme inducers and valproate; a switch to low enzyme inducing agents is therefore indicated (for example, from carbamazepine to less enzyme inducing sodium channel blockers such as lamotrigine, lacosamide, oxcarbazepine, or eslicarbazepine acetate).
Professional aspects
Occupational performance that is impaired as little as possible is an essential socio-medical treatment goal. While achieving good seizure control and, in particular, also avoiding severe, stigmatizing seizures and prolonged postictal impairment obviously contribute to this, cognitive, psychological, and motor tolerance also have considerable importance for job retention. Especially in intellectual activities, sedating substances (such as carbamazepine, phenobarbital) and cognitively problematic substances (topiramate, in some cases also higher-dose zonisamide, benzodiazepines and barbiturates) must therefore be avoided and cognitively well-tolerated substances (for example brivaracetam/levetiracetam, lacosamide, lamotrigine, eslicarbazepine acetate, pregabalin or also valproate) must be preferred.
In patients with high motor demands, drugs that cause tremor (valproate, lacosamide, lamotrigine) or lead to ataxia (especially sodium channel blockers with plasma peaks such as higher-dose unretarded oxcarbazepine or lacosamide, in my opinion also perampanel in some combinations) are not drugs of first choice.
Psychiatric side effects of antiepileptic drugs may also be essential for occupational integration. Often problematic here are both depressive moods and increased irritability, which is common with treatment with levetiracetam. These symptoms need to be actively inquired about, and an early change in medication prior to any development of occupational conflict is advised.
Polytherapy and the role of comedication
With the growing spectrum of available antiepileptic drugs, the possibility of their combination multiplies. Important basic rules for rational combination therapy are:
- Avoidance of enzyme inducers in combination with hepatically metabolized antiepileptic drugs (example: unfavorable combination of carbamazepine and lamotrigine).
- Selection of medications with different modes of action to achieve at least additive effect and subadditive side effects.
- Avoidance of combinations with more than two antiepileptic drugs.
- Observation of the total dose and adjustment of individual doses to give room for the development of an additionally given drug.
Interactions also play a significant role in the use of comedications to treat other conditions. Of particular importance in epilepsy patients are psychotropic drugs; here, pharmacodynamic adverse interactions with amoxapine, bupropion, clomipramine and maprotiline as well as pharmacokinetic interactions with sertraline and fluoxetine should be considered.
Comorbidities
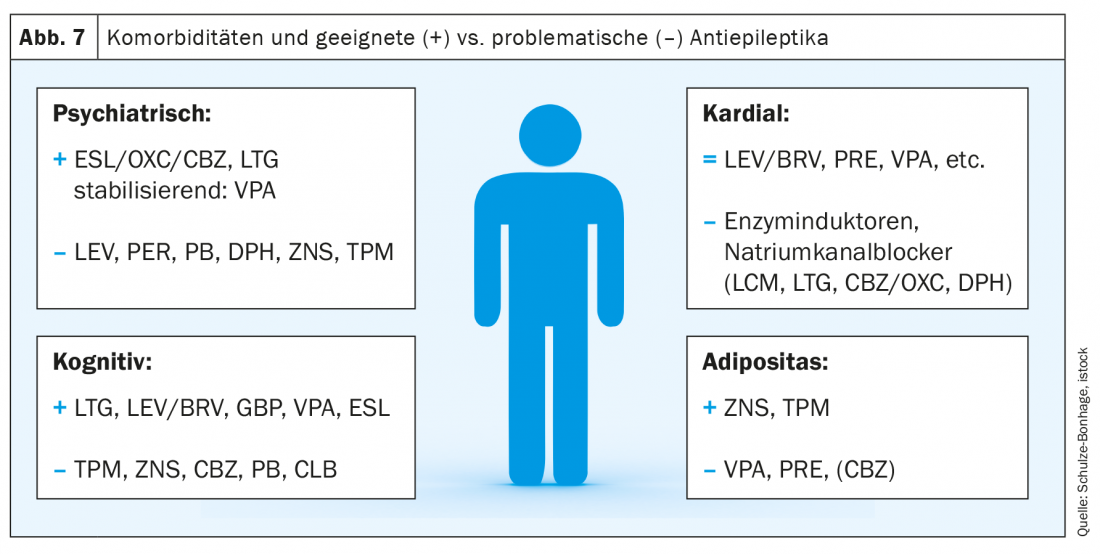
Comorbidities are a relevant aspect in epilepsies depending on age and are essential to avoid adverse effects. Psychiatric and internal diseases play the largest role here (Fig. 7).
- In the presence of depression, potentially depressogenic substances should be avoided (barbiturates, phenytoin, levetiracetam, and m.e. zonisamide).
- Mood-stabilizing substances such as sodium channel blockers, gabapentin/pregabalin and valproate are particularly suitable.
- The use of levetiracetam and perampanel is more likely to be avoided in psychotic disorders.
- For sleep disorders, substances that improve sleep structure are beneficial (such as pregabalin, m.E. perampanel).
The spectrum of possible internal comorbidities is wide. Frequently relevant are:
- Pre-existing Cardiac Conditions: Sodium channel blockers should be avoided in the presence of cardiac arrhythmias or conduction abnormalities or should be monitored with ECG registrations when used
- Obesity: antiepileptic drugs with a risk of developing metabolic syndrome should be avoided (especially valproate, pregabalin, and m.E. carbamazepine).
- In cases of hepatic or renal insufficiency, substances with alternative elimination are preferable.
Summary
The large number of available antiepileptic drugs allows for a choice of medication tailored to the individual patient. A variety of aspects play a role here, as compiled in the article. Many of the newer drugs allow for good tolerability even with long-term use and dosing regimens that are favorable for adherence. Another advantage of many modern antiepileptic drugs is a significantly reduced risk of drug interactions, especially in elderly patients. It is therefore worthwhile not to work with a fixed drug regimen, but to use a spectrum of antiepileptic drugs adapted to the patient.
As a rule, enzyme inducers and drugs with a significant risk of side effects, such as valproate and benzodiazepines, should be avoided in this context. Newly developed substances such as brivaracetam, eslicarbazepine acetate and lacosamide can also be used at an early stage in view of their improved tolerability, while other highly potent new developments such as perampanel and cenobamate* open up new opportunities for epilepsies that are difficult to treat.
* currently not yet approved in Switzerland
Take-Home Messages
- Lack of or weak enzyme induction in second- and third-generation antiepileptic drugs avoids previously typical antiepileptic drug side effects such as osteoporosis, polyneuropathies, and metabolic syndromes. These include lacosamide, levetiracetam, pregabalin, and other newly developed antiepileptic drugs such as brivaracetam, eslicarbazepine acetate, and cenobamate.
- For patients of older age, sodium channel blockers with little or no enzyme induction (lacosamide, lamotrigine, eslicarbazepine acetate) offer an important option.
- Teratogenicity data from pregnancy registries show lowest risks of low-dose treatments with lamotrigine, levetiracetam, and oxcarbazepine.
- The single-dose administration possible with eslicarbazepine acetate and perampanel is conducive to compliance.
- In particular, antiepileptic drugs with low interaction potential, neutral effect on bone metabolism and lipid metabolism, and low cardiac effects have advantages after the age of 50 years.
Literature:
- Rowan AJ, Ramsay RE, Collins JF, et al: VA Cooperative Study 428 Group. New onset geriatric epilepsy: a randomized study of gabapentin, lamotrigine, and carbamazepine. Neurology 2005; 64: 1868-1873.
- Ley M, Principe A, Rocamora R: Efectos a largo plazo de las dibenzacepinas sobre los parámetros metabólicos: comparación retrospectiva de carbamacepina, oxcarbacepina y acetato de eslicarbacepina en el mundo real. Rev Neurol. 2020; 71: 54-60.
- Mintzer S, Dimova S, Zhang Y, et al: Effects of lacosamide and carbamazepine on lipids in a randomized trial. Epilepsia. 2020; 61(12): 2696-2704.
Further reading:
- Marson A, Burnside G, Appleton R, et al: SANAD II collaborators. The SANAD II study of the effectiveness and cost-effectiveness of valproate versus levetiracetam for newly diagnosed generalised and unclassifiable epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet 2021; 397(10282): 1375-1386.
- Marson A, Burnside G, Appleton R, et al: SANAD II collaborators. The SANAD II study of the effectiveness and cost-effectiveness of levetiracetam, zonisamide, or lamotrigine for newly diagnosed focal epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet 2021; 397(10282): 1363-1374.
- Marson AG, Al-Kharusi AM, Alwaidh M, et al: SANAD Study group. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet 2007; 369(9566): 1016-1026.
- Marson AG, Al-Kharusi AM, Alwaidh M, et al: SANAD Study group. The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomised controlled trial. Lancet. 2007; 369(9566): 1000-1015.
- Sake JK, Hebert D, Isojärvi J, et al: A pooled analysis of lacosamide clinical trial data grouped by mechanism of action of concomitant antiepileptic drugs. CNS Drugs 2010; 24(12): 1055-1068.
- Schulze-Bonhage A: Epilepsies: forms, diagnosis and therapy. Medical Monthly Journal for Pharmacists 2021, 44: 160-170.
- Schulze-Bonhage A, Hintz M: Perampanel in the management of partial-onset seizures: a review of safety, efficacy, and patient acceptability. Patient Prefer Adherence 2015; 9: 1143-1151.
- Semah F, Picot MC, Adam C, et al: Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology 1998; 51: 1256-1262.
InFo NEUROLOGY & PSYCHIATRY 2021; 19(5): 14-21.