A research team collected data in ten countries to evaluate the benefits of current and previous treatment strategies for atopic dermatitis. The results should contribute to an improvement in “disease management”. One finding of the study was that above a certain level of severity, topical therapy alone is often insufficient to meet key treatment expectations (itch relief and healing of skin lesions), but requires the use of systems therapeutics.
For this “real world” survey study, adult patients with atopic dermatitis (AD) were recruited via internet panels for a web-based survey between July and September 2019 [1]. A total of 1988 AD patients from Germany, France, the United Kingdom, Belgium, the Netherlands, Italy, Spain, Canada, Australia, and Japan were included in the analysis. Inclusion criteria included age (≥18 to ≤75 years**) and current treatment. In addition to demographic information, disease characteristics, including patient-rated worst BSA (body surface area) in the previous year, treatment strategies (previous/current therapies, reasons for discontinuation, treatment of acute AD episodes), and treatment benefits (expectations of AD treatment and extent to which expectations were met) were recorded. Participants included in the analysis were on treatment with topical monotherapies (topical corticosteroids, calcineurin inhibitors) or conventional systemic therapeutics (cSys; systemic corticosteroids, immunosuppressants) or biologics (dupilumab$ only at this time) at the time of the survey. Participants who were currently receiving phototherapy or combination therapy with cSys and biologics were excluded.
** in Japan, the lower age limit was ≥18 years.
$ with or without topical treatments
More flares occurred with BSA≥10% with topical therapy alone
A BSA<10% was exhibited by 86.6% of the study participants [1]. In patients with a BSA ≥10%, the median disease duration was higher than in patients with a BSA<10%. The most commonly used AD therapies in both BSA groups were topical monotherapies (69.69%), followed by conventional systemic therapeutics (28.1%)-including corticosteroids (16%) and immunosuppressants (12.1%)-and biologics (2.3%). The average number of relapses in the past year was higher in patients with a BSA≥10% than in patients with a BSA<10%. Regardless of BSA involvement, most patients treated acute flares with topical medications (73.4%), followed by conventional systemic therapeutics (25.3%) and biologics (1.3%). Patients with a BSA≥10% used fewer topical monotherapies during a relapse compared with those with a BSA<10% (67.5% vs 74.1%), while the proportion of cSys treatments was higher (31.7% vs 24.6%).
Participants with a BSA ≥10% who were treated with topical monotherapy experienced more disease flare-ups and were more likely to discontinue topical treatment because of poor skin tolerance. This underscores the need for long-term systemic treatment solutions in these adult patients [2,3].
| Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by eczematous, intensely itchy, and often painful lesions that affect patients’ sleep, well-being, and quality of life [9]. Moderate-to-severe AD usually warrants systemic therapy and is defined as an Eczema Area and Severity Index (EASI) ≥16 or EASI <16 plus ≥1 of the following conditions: Localization to the face, hands, or genital area; itching with a numeric rating score (NRS). >7; Sleep disorders with NRS >7; Quality of life impairment with a Dermatology Life Quality Index (DLQI). >10 or a minimum involvement of ≥10% of the body surface area (BSA). [4,5,10,11]. |
To what extent were the expectations of the therapy met?
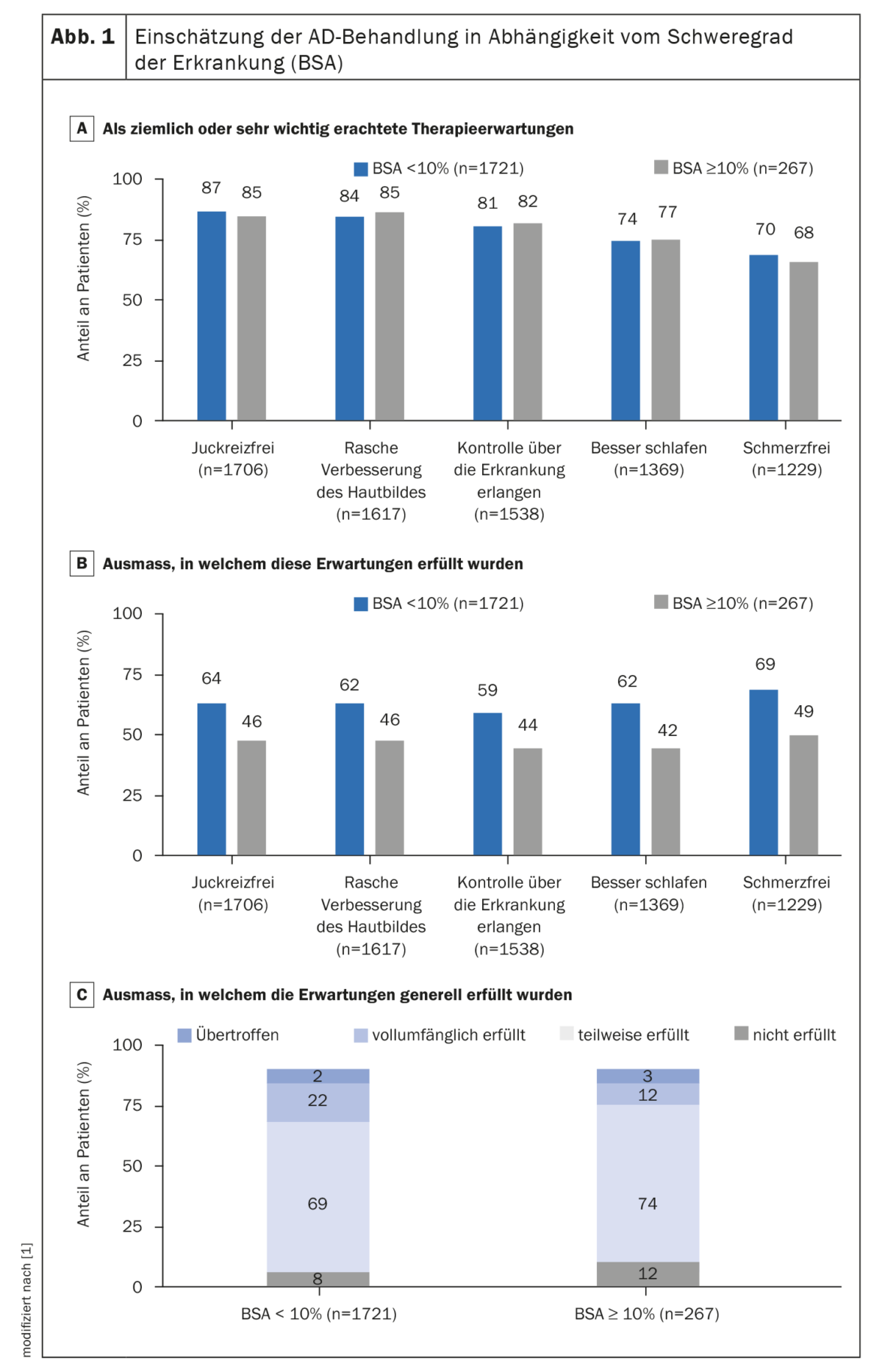
Regardless of BSA involvement, participants reported being itch-free, quickly getting a better skin appearance, having the disease back under control, sleeping better, and being pain-free as their most important expectations from treatment (Fig. 1A) [1]. Overall, 75% of patients reported that their expectations were only partially met or not met at all. Patients with a BSA≥10% were less likely to report that their expectations were fully met compared with patients with a BSA<10% (Figs. 1B, 1C) [1].
The main reason for discontinuation of previous AD treatment was inadequate skin tolerance in 31.9% of patients. Other reasons for discontinuation of previous treatments included physician recommendations (26.3%), failure of the drug to persist (26.5%), and slow onset of action of the drug (24.9%). When patients were asked to indicate reasons for discontinuing treatments by drug class, topical preparations were discontinued primarily because of insufficient freedom from manifestations (35.5%), cSys treatments primarily because of physician-recommended changes in treatment (29.4%), and biologics primarily because onset of action was too slow (32.3%).
Those with body surface involvement of ≥10% reported lower treatment satisfaction. Overall, this study indicates that there is an unmet medical need in the field of AD treatment.
Discussion
To achieve adequate control of moderate/severe AD, a personalized treatment strategy is recommended taking into account various factors such as BSA, relapse frequency, quality of life, and specifics of each systemic therapy option [2,4–7]. That most adult patients’ expectations were not met or only partially met in this study, and a higher proportion of patients with a BSA ≥10% reported that their treatment expectations were not met, may be related to inadequate symptom control with topical monotherapy.
The study authors emphasize that it is important not to withhold systemic therapy from patients who are eligible for it. Furthermore, they point out that combination therapies may be useful to achieve the intended therapeutic goals [2,7,8]. The authors cite the relatively small number of participants under biologics treatment, self-reported BSA participation, and possible selection and information bias as methodological limitations. Because the survey was conducted in 2019, it does not fully reflect the current treatment environment, he said.
Nevertheless, the study results are informative as they demonstrate that itch relief and improvement of skin appearance as primary goals in the therapy of atopic dermatitis are often not achieved with topical treatment alone and it may be important not to miss the time for systemic therapy.
Literature:
- Augustin M, et al: Real-World Treatment Patterns and Treatment Benefits among Adult Patients with Atopic Dermatitis: Results from the Atopic Dermatitis Patient Satisfaction and Unmet Need Survey. Acta Derm Venereol 2022; 102: adv00830.
- Boguniewicz M, et al: Expert perspectives on management of moderate-to-severe atopic dermatitis: a multidisciplinary consensus addressing current and emerging therapies. J Allergy Clin Immunol Pract 2017; 5: 1519-1531.
- Fougerousse A-C, et al: Use of systemic medications for treating adult atopic dermatitis in France: results of a practice survey. Clin Cosmet Investig Dermatol 2021; 14: 179-183.
- Wollenberg A, et al: Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol 2018; 32: 657-682.
- Wollenberg A, et al: ETFAD/EADV Eczema task force 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. J Eur Acad of Dermatol and Venereol 2020; 34: 2717-2744.
- Simpson EL, et al: When does atopic dermatitis warrant systemic therapy? Recommendations from an expert panel of the International Eczema Council. J Am Acad Dermatol 2017; 77: 623-633.
- Fougerousse A-C, et al: Use of systemic medications for treating adult atopic dermatitis in France: results of a practice survey. Clin Cosmet Investig Dermatol 2021; 14: 179-183.
- Bieber T: Atopic dermatitis: an expanding therapeutic pipeline for a complex disease. Nat Rev Drug Discov 2022; 21: 21-40.
- Augustin M, et al: Characterizing treatment-related patient needs in atopic eczema: insights for personalized goal orientation. J Eur Acad Dermatol Venereol 2020; 34: 142-152.
- Calzavara Pinton P, et al. Diagnosis and management of moderate to severe adult atopic dermatitis: a Consensus by the Italian Society of Dermatology and Venereology (SIDeMaST), the Italian Association of Hospital Dermatologists (ADOI), the Italian Society of Allergy, Asthma and Clinical Immunology (SIAAIC), and the Italian Society of Allergological, Environmental and Occupational Dermatology (SIDAPA). G Ital Dermatol Venereol 2018; 153: 133-145.
- Schmitt J, et al: Determinants of treatment goals and satisfaction of patients with atopic eczema. J Dtsch Dermatol Ges 2008; 6: 458-465.
DERMATOLOGIE PRAXIS 2023; 33(3): 20-21