Due to the different ages and biological developmental stages (maturity stages) of growing patients, recognizing and treating a fracture in childhood is not always easy. It takes some experience to distinguish a fracture/fissure from physiological changes in the growing skeleton. The infantile elbow in particular, with its multiple bone cores, presents a challenge. This article is about the upper extremities. The second part on the lower extremities will appear in the next HAUSARZT PRAXIS.
The likelihood of a child sustaining a fracture between 0 and 16 years of age is reported to be approximately 27% in girls and 42% in boys [1].
Both the epiphyseal joints (growth plates) and the different biology of the child’s bone compared to the adult must be taken into account when treating fractures in children.
The child’s bone is much more elastic than that of an adult and the bone strength is lower. The periosteum (bone skin) is still very thick in the child. As a result, children have fewer comminuted fractures but more frequent osseous ligament/muscle avulsions. Also, for the reasons mentioned above, shaft fractures are much more common in children than joint fractures.
If the growth plate is also affected in a fracture, the risk of growth disturbance (growth arrest vs. increased growth) must be considered here. However, depending on the fracture pattern, the growth plates may also correct a posttraumatic deformity during further growth by remodeling [2]. It should be noted here that so-called remodeling does not work equally well on all bones and a certain residual growth of the joint must still be present in order to effect corrections. Basically, most of the growth in the upper extremity occurs eccentrically (upper arm: 80% of length growth proximal humeral epiphysis; forearm: 80% of length growth distal radial/ulnar epiphyseal fossa) and concentrically in the lower extremity (thigh: 70% length growth distal femoral epiphysis; lower leg: 55% length growth proximal tibial epiphysis). Thus, the greatest remodeling potential is to be expected here.
According to a database from the University Hospital Mainz with 2750 fractures, the most frequently affected region for fractures in children is the forearm (38%). The upper arm is affected in only 13.8% of cases, with the largest proportion of fractures occurring near the elbow (10.4%).
If the growth plate is involved in a fracture, it is classified according to the Salter-Harris classification [1]. Recently, the Association for Osteosynthesis (AO) has developed the “AO Pediatric Comprehensive Classification of Long-Bone Fractures” (PCCF) [3], which is comparable to the AO classification for adults.
In the case of an epiphyseal fracture, a potential articular fracture must be assumed and anatomic reduction/reconstruction should be attempted. Here, in the case of surgical interventions, screw osteosynthesis is often performed if the reduction cannot be held in plaster or the dislocation is >2 mm.
In metaphyseal injuries, the position should be axial, but some malpositioning may be tolerated here, depending on the location of the fracture and the growth potential of the joint. If conservative treatment is not possible, temporary Kirschner wire fixation is recommended here.
Diaphyseal fractures should be positioned correctly in terms of axis and rotation, especially in the forearm region, as otherwise restrictions in pro-/supination can occur even with axial misalignments >10°.
The further a fracture is from the adjacent growth plate, the less deformity can/must be tolerated. For shaft fractures, surgical treatment is the domain of elastically stable intramedullary nailing (ESIN) with titanium nails.
Special forms
Special forms of infantile fractures are the greenwood fractures, which represent incomplete fractures in which the periosteum is torn on the convex side and incomplete fracture healing with the risk of refracture can occur here due to a lack of compression. Therefore, these fractures should be completed (broken through). Here, potentially stable fractures can become unstable, so that they then also have to be osteosynthesized.
The more harmless bulge or compression fractures merely represent a plastic deformation of the elastic fetal bone and can usually be healed conservatively in a cast.
In all fractures where conservative treatment has been started but the fractures cannot be clearly assessed as stable, a radiological position check should be performed after five to seven days. If further dislocation occurs here, the treatment regime must be changed.
Clavicle fractures (Fig. 1)
Conservative treatment is usually indicated. Here, depending on the age of the child, immobilization for three to five weeks in a Mitella sling or backpack bandage is sufficient. During this time, active movements of the arm above the horizontal should be avoided so as not to provoke pain by co-rotation of the clavicle.

In patients who are very active in sports as well as massive shortening of the fracture >2 cm, surgical interventions can be offered as an alternative. Here, the ESIN technique represents the gold standard of surgical treatment. Plate osteosyntheses are used in children only very rarely and in exceptional cases.
Absolute indications for surgery are only open fractures with injuries to the vascular/plexus system and compromise of the skin by fracture fragments.
Humeral fractures
Because of its anatomic proximity to the proximal growth plate, treatment of the subcapital humerus fracture is the domain of conservative treatment in a Gilchrist bandage or orthogilet. In this case, malpositions of 40-70° angulation at most can be tolerated in the child <10 years. Likewise, ad latus malpositions as well as shortenings are remodeled.
In the case of excessive malalignment, especially in older children >12 years, closed reduction and ESIN treatment are also favored here.
Humeral shaft fractures are relatively rare and more commonly seen in association with traffic accidents. Here, too, can often be successfully treated conservatively with Gilchrist, or Orthogilet. Surgical indications are open fractures or, in the multiply injured child, improvement of the child’s mobilization by stable osteosynthesis. In that case, it is also treated with ESIN.
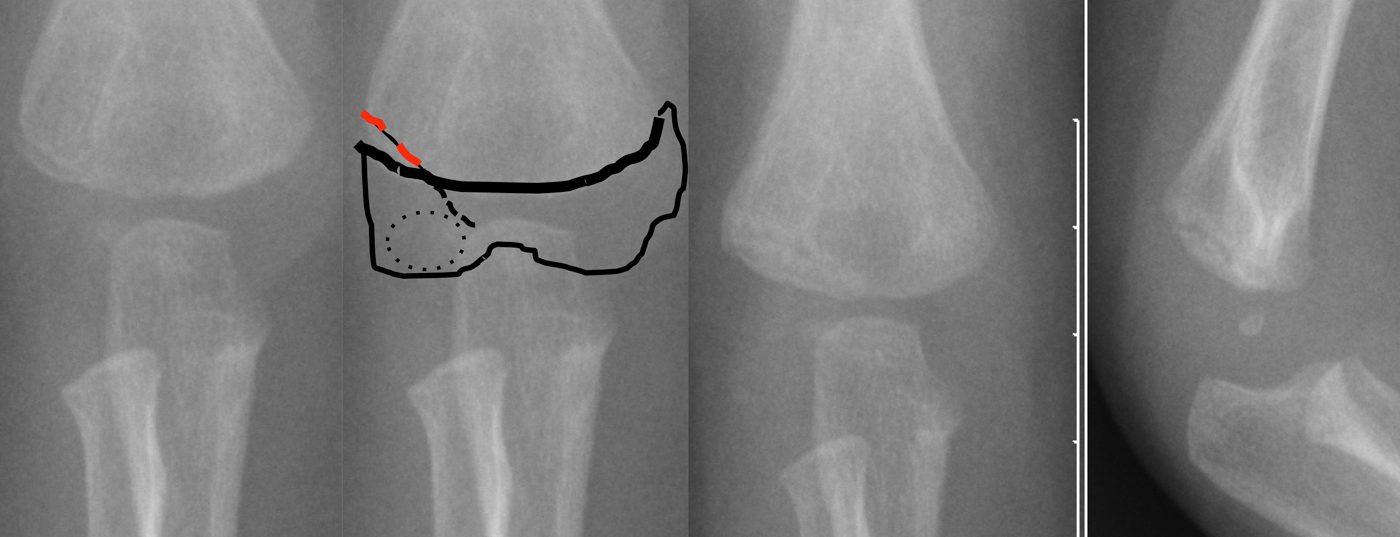
Fractures at the elbow (Fig. 2)
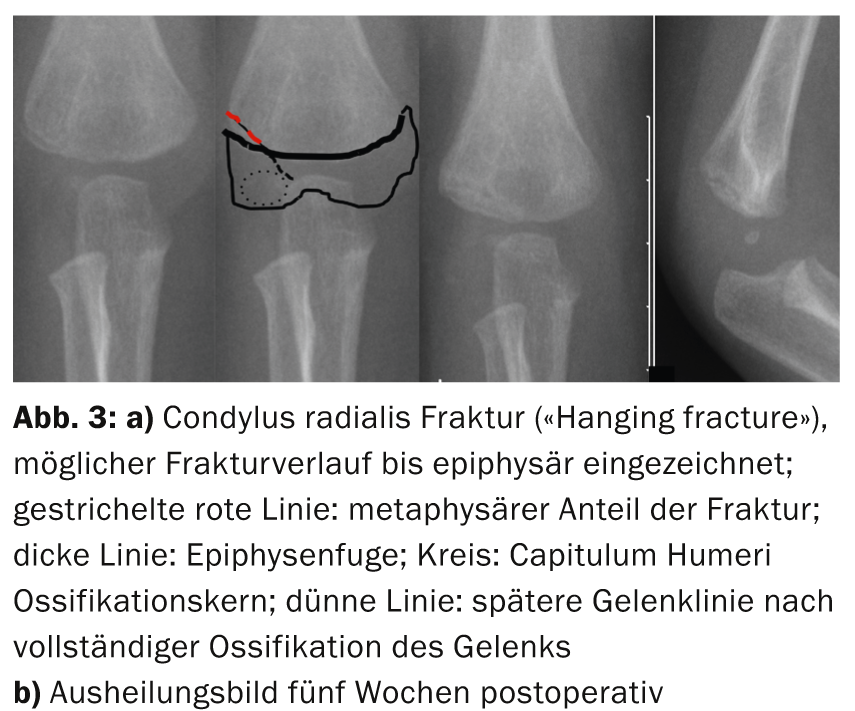
Condylus radialis fracture: This is an injury that can be underestimated due to the late complete ossification of the capitulum with the distal humerus.
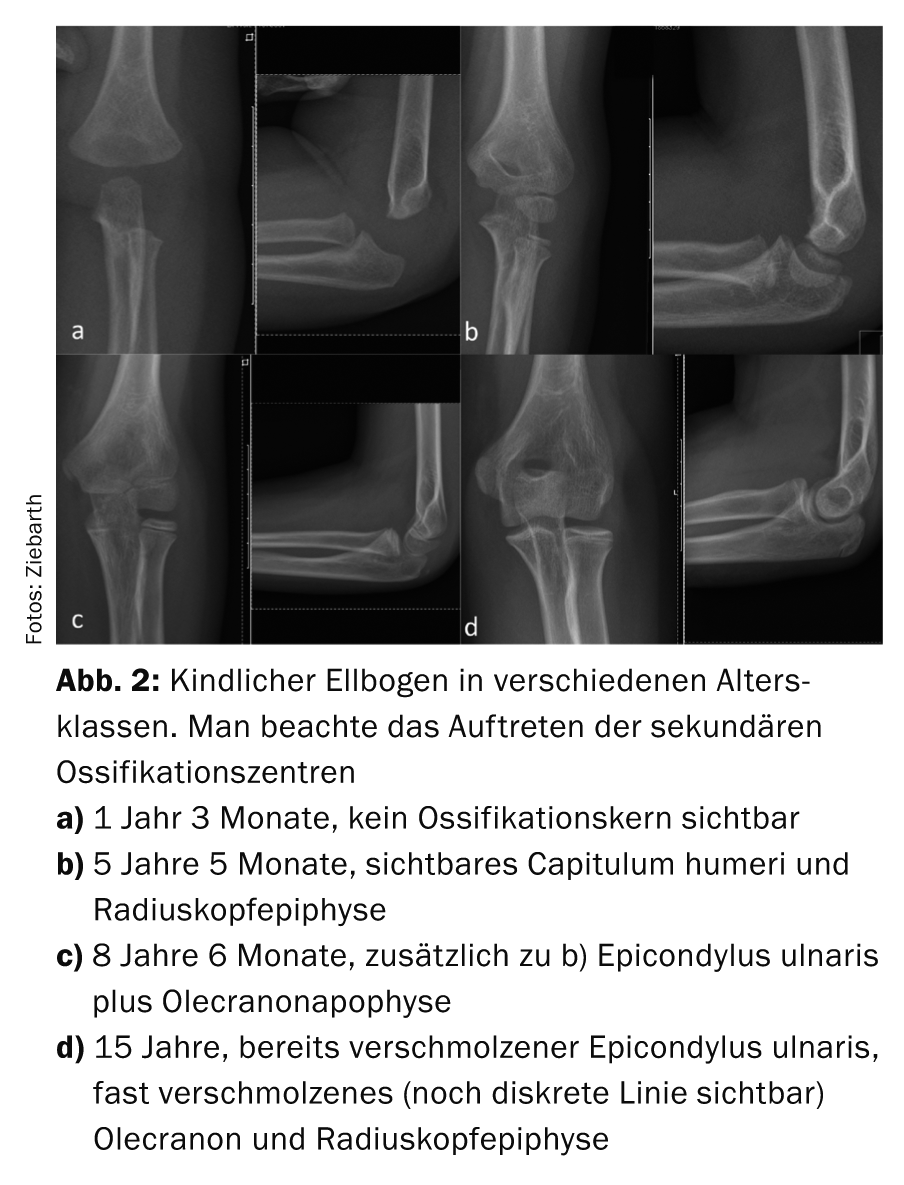
It must be remembered here that the course of the fracture can extend down into the joint and thus a primarily undisplaced fracture can also dislocate secondarily. Therefore, it is urgently necessary to perform a plaster-free control X-ray after four to five days to check the position. Dislocations <2 mm can be treated conservatively in an upper arm cast (Fig. 3), otherwise open reduction and Kirschner wire fixation is necessary.
Ulnar epicondyle fracture: This is an avulsion injury of the forearm flexors or a direct avulsion after elbow dislocation. Fracture progression occurs through the joint, so even a “normal” ulnar humeral epicondyle can sometimes be misinterpreted as fractured by the untrained. The traction of the flexors often distalizes the fracture fragment from the humerus, so that open reduction and screw osteosynthesis is not infrequently indicated here.
If the fracture is only slightly dislocated, it can be treated conservatively in a humeral cast.
Supracondylar humerus fractures
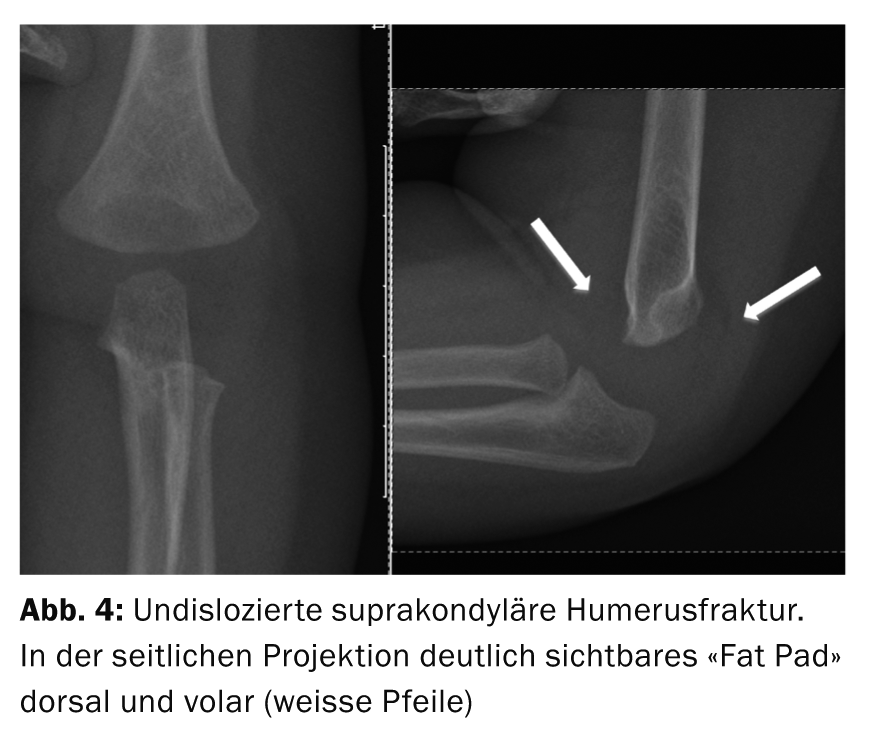
Between the ages of zero and seven years, this is the most common fracture location in children [4]. The fracture mechanism occurs by falling on the outstretched arm. This results in a typical gentle posture. The fracture is classified according to the extent of dislocation according to Gartland. In general, these fractures can also be classified as extension or flexion injuries depending on the tilt of the distal fracture fragment. Undislocated fractures can easily be overlooked. Here it is advisable to also look for indirect fracture signs such as the “fat pad”, which represents an outpouching of the joint capsule (joint effusion) in a dorsal and volar direction (Fig. 4).
Undislocated or only slightly dislocated (mainly extension injuries) supracondylar humerus fractures can be treated conservatively in a humeral cast. Particularly in young patients and in extension injuries, therapy with the Blount sling is an alternative (cuff and collar), as here reduction of the fracture can be achieved by flexion in the elbow joint.
Since supracondylar fractures may not infrequently be associated with vascular/nerve lesions, close examination for motor and sensory function of all three nerves (median, ulnar, radial) and monitoring of peripheral circulation are very important. However, it should be noted that loss of function of a nerve or nerves, whether purely sensory or even partially motor, is not an indication for surgical exploration of the nerve during osteosynthesis. Recent literature as well as our own experience show that the majority of sensorimotor deficits disappear spontaneously within the following three to six months, and that a pulseless but rosy recapillarizing arm or hand is no longer an absolute indication for vascular exploration [5].
Radius neck/head fractures
Such fractures must always be sought if, despite adequate trauma, the supracondylar region and the condyles/epicondyles appear radiologically inconspicuous. In this case, sometimes only a small compression of the neck of the radius may be present and indirect fracture signs should be looked for as mentioned above (Fig. 4).
If pro/supination is unrestricted, immobilization for one to two weeks in an upper arm plaster splint is sufficient. In the case of dislocated fractures, closed reduction and fixation using ESIN is indicated; in this case, postoperative immobilization is no longer required.
Special forms of elbow injuries
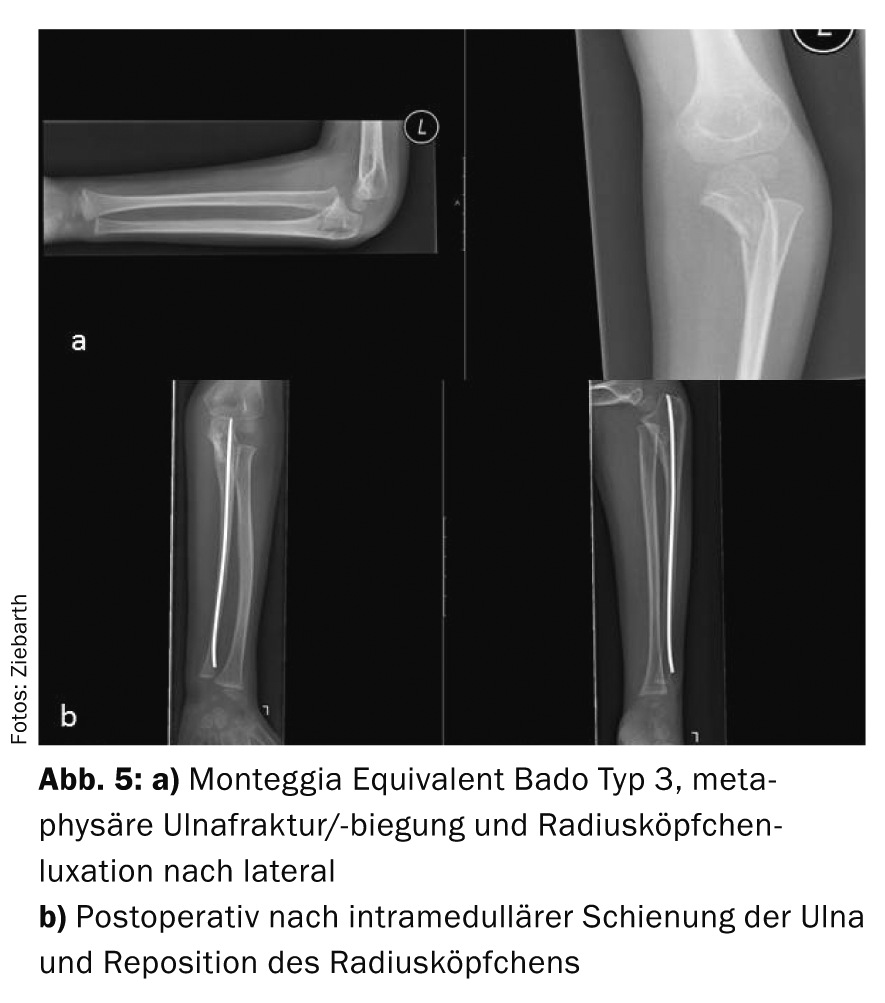
Such can be: Monteggia injuries or Monteggia equivalent injuries. This involves a fracture of the proximal ulna and radial head dislocation. Fractures are classified according to the direction of dislocation of the radial head (Bado type 1-4) [6]. In this case, referral to the Children’s Hospital should always be made because the therapy is exclusively surgical. It is important for the practitioner that in proximal ulna fractures, the position of the radial neck or the radial spine is always taken into account. -head (depending on the age of the child and ossification status) is checked. Here, the proximal radius must always be centered on the capitulum humeri in all planes. This also applies to ulnabowing or olecranon fractures (Fig. 5).
Forearm fractures
In the case of dislocation <10°, conservative treatment in an upper arm cast is possible. If the stability of the fracture is not confirmed, a control X-ray is indicated after five to seven days.
Due to the low remodeling potential even in smaller children, the indication for osteosynthesis by means of ESIN is generously given here [7]. Nowadays, the ESIN technique is a simple and safe method for these fractures and plaster immobilization is no longer necessary postoperatively. In the case of malpositions >10° of radius or ulna on the forearm, the turning movement (pro-/supination) can be significantly compromised, which can be very disturbing for the patient in some cases.
Distal metaphyseal forearm fractures
This is the most common skeletal injury in childhood. Both bones (radius and ulna) or only the radius may be affected. Due to the very good remodeling potential of the distal radialphysis joint, tilts of 30-40° in the sagittal plane can be accepted here, especially in younger children. Immobilization is performed in an upper arm cast.
Closed reduction and plaster immobilization is indicated for dislocated fractures. Only in exceptional cases is a Kirschner wire fixation or an external fixator indicated, usually for very unstable fractures of both forearm bones.
Hand/Finger Injuries
These are often low-displacement fractures that can be treated with immobilization in an aluminum splint or Edinburgh cast. In this case, only the joint fractures and fractures with rotational malalignment should be surgically corrected and referral to the pediatric traumatologist is recommended in this case.
Kai Ziebarth, MD
Literature:
- Beaty JH, Kasser JR: Rockwood and Wilkins’ Fractures in Children. LWW Seventh Edition 2009.
- Stilli S, et al: Remodeling and overgrowth after conservative treatment for femoral and tibial shaft fractures in children. Chir Organi Mov 2008 Jan; 91(1): 13-19. doi: 10.1007/s12306-007-0003-6. epub 2008 Feb 10.
- Slongo TF, Audigé L, AO Pediatric Classification Group: Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF). J Orthop Trauma 2007 Nov-Dec; 21(10 Suppl): S135-160.
- Cheng JC, Shen WY: Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma 1993; 7: 17.
- Weller A, et al: Management of the Pediatric Pulseless Supracondylar Humeral Fracture: Is Vascular Exploration Necessary? J Bone Joint Surg Am 2013 Nov 06; 95(21): 1906-1912.
- Bado JL: The Monteggia lesion. Springfield: Thomas, 1962.
- Colaris JW, et al: Risk factors for the displacement of fractures of both bones of the forearm in children. Bone Joint J 2013 May; 95-B(5): 689-693.
CONCLUSION FOR PRACTICE
- Fracture recognition and adequate therapy are sometimes difficult due to the special characteristics of the infantile bone.
- The indication for conservative treatment can be more generous in children than in adults, since remodeling is possible due to the open growth plates.
- The indication of conservative therapy and thus acceptance of a deformity should take into account not only the chronological age of the patient, but also the localization of the fracture and the biological age of the patient (stage of maturity, joint condition).
- If in doubt, immobilization of the fracture in a cast and referral to a pediatric traumatologist is recommended.
- The treatment scheme for operative and conservative therapy of fractures of growing age is available at the pediatric surgical outpatient clinic at the Inselspital Bern.
HAUSARZT PRAXIS 2014; 9(5): 28-32