Scabies is by no means a disease of bygone days, but there is evidence of an increase in incidence in Central Europe. Children are a major source of infection, but the highly infectious skin disease affects all age groups. If an infestation has been detected, rapid action is important. Local therapy with permethrin is still considered an effective first-line therapy. Correct application is crucial for the success of the treatment. An observational study indicates that poor use of topical therapy is behind putative permethrin resistance.
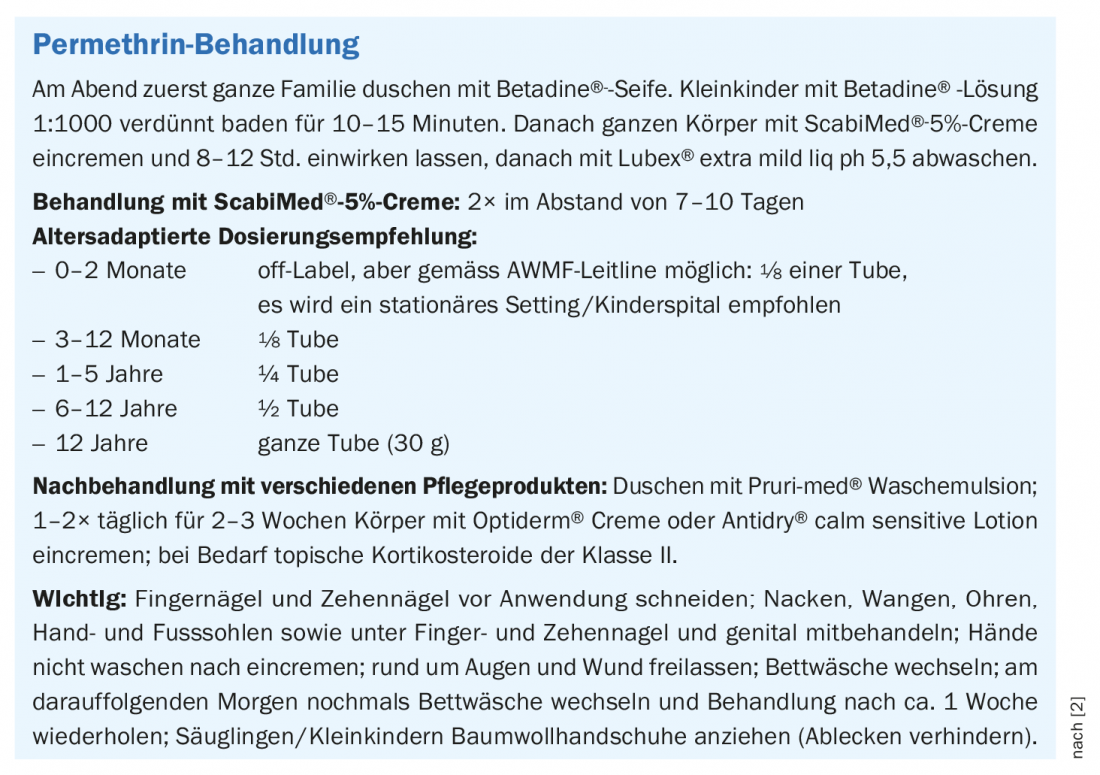
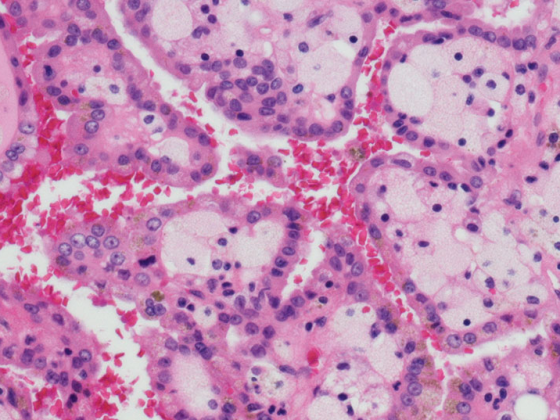
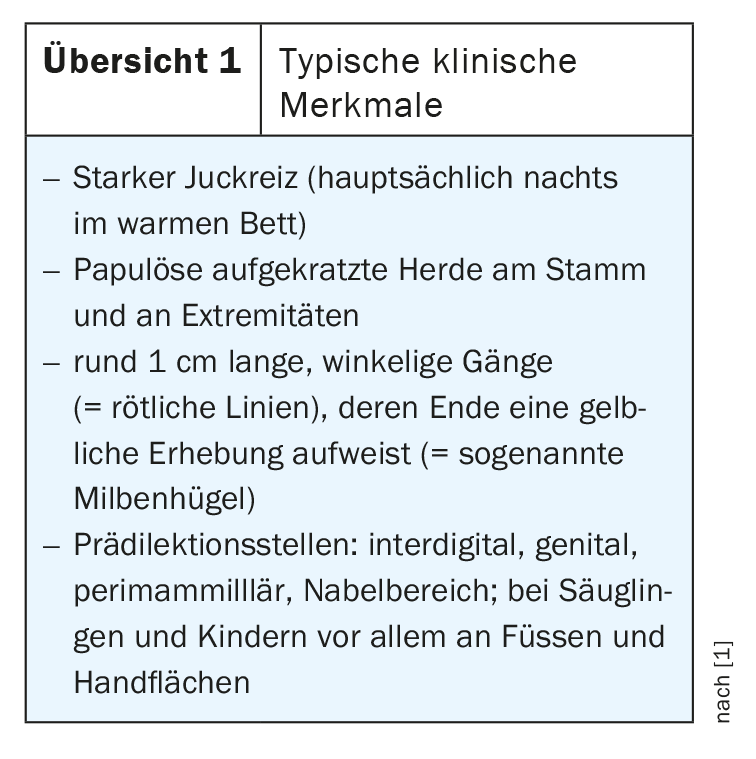
Infestation of the skin with the mite Sarcoptes scabiei causes intensely pruritic lesions with erythematous papules and ducts in the interdigital spaces, wrists, waist, and genitalia (Fig. 1). Clinical diagnosis is made by history and physical examination. In addition to typical skin changes at predilection sites (overview 1), infestation of contact persons and family members are indicative [1]. For the success of therapy, it is essential to include not only individuals but always all possible contacts in the treatment in order to prevent recurrences or further spread. Currently common treatment options in this country are permethrin 5% lotion or cream, and ivermectin is used for systemic therapy (box).
Topical antiscabiosa should be spread over the entire body from the mandible down. Correct application is crucial for targeted treatment, but is often a sticking point. That permethrin resistance exists is doubted by Prof. Antonio Cozzio, MD, Chief Physician, Clinic of Dermatology, Venereology and Allergology, Cantonal Hospital St. Gallen [2]: “Live Sarcoptes have been detected up to 36 hours after permethrin application, but so far there is no definite resistance,” he said.
Proven local therapeutic agent against scabies mites
In Europe, permethrin is considered the topical agent of choice for many forms of scabies and is recommended by guidelines regardless of age, as several studies have found superior efficacy compared to other topical agents or permethrin has been shown to be more feasible, and also well tolerated, with similar efficacy [3]. Permethrin is both scabicidal and ovocidal, so in uncomplicated scabies a single treatment is theoretically sufficient, but in practice two treatments have been shown to be effective [2]. The overall therapeutic goal is to kill the scabies mites and their larvae and eggs. Since mites are localized in the stratum corneum, they can be killed by topical antiscabiosa in most cases. Secondary therapeutic goals consist in the treatment of the often pronounced itching as well as of accompanying inflammatory symptoms and secondary infections.
Application errors when applying cream can reduce treatment success
A recent study of scabies patients showed that up to 30% of the body surface was not creamed, including predilection sites [4]. The subjects were instructed to apply a cream without permethrin, in which a fluorescent dye had been mixed.optimally according to instructions for a test run of the treatment. As it turned out, of the 21 study participants examined, not a single one had applied cream to the entire surface of their bodies despite appropriate instruction.
On average, 6% of the body surface area remained untreated, with a range of 2-30%. While the cream had been applied to the hands and fingernails as instructed, the malleolus, interdigital spaces, and axillary region – all frequently Sarcoptes scabiei infested locations – were among the most frequently untreated areas of the body. “Even though we tell people how important it is that they put lotion on everywhere, they don’t succeed,” Prof. Cozzio explains. A large part of the so-called Permethrin resistance was due to insufficient application. The expert advises at least two treatments with permethrin to optimize the effect, even if a single treatment is theoretically sufficient. In addition, should also be followed up with topical steroids for 1-2 weeks. “Follow-up is important because Sarcoptes is killed but can persist in the epidermis for up to 4 weeks and still produce pruritus through a type IV reaction,” explained Prof. Cozzio.
In summary, the reasons for an inadequate response to permethrin treatment are more likely to be poor creaming than effective permethrin resistance, summarizes Prof. Cozzio. In first and second relapses, the combination of ivermectin and permethrin is useful to optimize the probability of successful therapy. However, this is not indicated as a first-line treatment (for fear of permethrin resistance), the speaker said.
Congress: Dermatology Focus 2021
Literature:
- Scabies: physician fact sheet,%C3%(last accessed 07/14/2021).
- Cozzio A: News from the clinic and news from the pediatric dermatology publications. Prof. Antonio Cozzio, MD, Dermatology Focus, March 11, 2021.
- Sunderkötter C, et al: S1 guideline on the diagnosis and therapy of scabies – abridged version. J Dtsch Dermatol Ges 2016; 14(11): 1160-1171.
- Nemecek R, et al: Application errors associated with topical treatment of scabies: an observational study. J Dtsch Dermatol Ges 2020; 18(6): 554-559.
DERMATOLOGIE PRAXIS 2021; 31(5): 59-60 (published 8.10.21, ahead of print).