The majority of chronic wounds have vascular causes. If vascular therapy methods have been exhausted, innovative therapy strategies such as light therapy are becoming increasingly important. Light therapy – such as low-level laser therapy, photodynamic procedures, and water-filtered infrared – achieve effects independent of the vasculature and may therefore be a gamechanger in the treatment of chronic stagnant wounds. The biochemical and biophysical effects depend on the wavelength and range from promotion of angiogenesis and blood flow to anti-inflammatory, pain relief and anti-infective effects.
Chronic wounds are increasingly polycausal in nature, with a vascular etiology in the majority of cases, and it is not uncommon for current therapeutic strategies to reach their limits. Improvement of the wound situation is mostly dependent on a competent vascular system. Disturbances of the inflow, for example due to arteriosclerosis, are a major challenge. More complex reconstructive arterial procedures have finite rates of openness or are no longer possible. Thus, the “transport route vascular system” is almost blocked and not usable. Other ways have to be found to provide energy to the cells. This is where the fantastic possibilities of light therapy come into play. Light can develop its positive effects independently of the vascular system.
It is well known that light plays a central role in various biological processes. It influences, for example, the growth of plants, the behavior of animals and all human biorhythms. It has essential effects on our hormonal system and is significantly involved in the formation of essential substances, such as vitamin D.
In terms of medical history, the realization that light can have healing powers goes back to ancient Greece and was advocated by Hippocrates, the father of modern medicine, and also Galen.
Light therapy in medicine: a long success story
In the 19th century, Danish physician Niels Ryberg Finsen discovered that ultraviolet light could be effective in treating skin diseases such as lupus vulgaris and other forms of tuberculosis. For his groundbreaking discoveries in the field of light therapy, Finsen received the Nobel Prize in Medicine in 1903. Oscar Bernhard treated chronic wounds with the light of the sun in Samenda. Since the 1920s, the power of light has been used to treat jaundice in newborns. With the help of short-wave blue light, the bilirubin stored in the newborn’s skin is converted into a water-soluble form known as lumirubin, which can then be excreted via the bile and kidneys.
The first documented photodynamic therapy was performed by W.H. Goeckermann for psoriasis. In his scheme published in 1925, he recommended the combination of UV irradiation of the affected skin, which was previously rubbed with a coal/tar ointment. Photodynamic therapy, as a further development of phototherapy, gained momentum through the research activities of Dr. Hand Kuske, a clinic director in Bern. This founded the Psoralen UVA therapy (PUVA), which is still used today. Plant substances known as psoralen are used here as photosensitizers. In the 1980s, the use of brightness or light therapy became popular for treating seasonal depression, also known as winter depression. The therapy consists of exposing the patient to a bright artificial light source to improve mood.
Today, light therapy – either alone or in combination with a previously applied photosensitizer – is used to treat a variety of conditions, including skin diseases, sleep disorders, bipolar disorder, cancer, Alzheimer’s disease and more. Light therapy has evolved over the centuries and remains an important part of modern medicine
To date, UV-C irradiation of blood bags is performed. It is used to sterilize the blood and reduce the risk of infection during transfusions. In addition, light is used in surgery to cut or coagulate tissue. Here, lasers or other light sources are used to perform precise and minimally invasive procedures.
To understand the clinical potential of light therapy, it is worthwhile to look at the biochemical and biophysical basis of the many medically useful effects.
Electromagnetic radiation: wave-particle duality
Light can be considered both as a wave and as a particle. This concept is called wave-particle duality and is a fundamental principle of quantum mechanics. In quantum mechanics, light is described as a photon that has both a wave and a particle property. The choice of description often depends on the type of measurement made to study the behavior of light.
Light consists of electromagnetic waves that have different wavelengths and frequencies. In everyday life, light is often equated with visible light, which can be perceived by the human eye. However, visible light is only a small part of the electromagnetic spectrum (Fig. 1) and includes the wavelengths of about 400-700 nanometers (nm) [1]. The seven basic colors of visible light are: red, orange, yellow, green, blue, indigo, violet. Each color of the visible spectrum has a specific wavelength and frequency and affects our perception of and reactions to light in different ways. For example, blue light can boost energy levels and increase alertness, while red light can be calming and promote sleep. Other colors of the light spectrum also have specific biological effects and are used in various applications such as light therapy and photobiomodulation.

However, our body not only needs light to see, but also to maintain its bodily functions. In general, different wavelengths have different biochemical and biophysical effects. Therefore, nowadays not only a “full spectrum light” is applied, but increasingly light of a certain wavelength. Depending on the predominant symptom, the appropriate wavelength is selected. Each wavelength has its own special effect and also individual penetration depth. Short-wave light, such as blue or green, penetrates less deeply into tissue than long-wave light, such as red or near-infrared. In general, visible light can penetrate only a few millimeters deep into the skin, while near infrared light (“near infrared”) can penetrate up to a few centimeters deep into the tissue, depending on the intensity. The depth of penetration may also be influenced by other factors such as the nature of the tissue and the duration of application. To avoid causing damage to tissue, the laser light should be low energy. This is also referred to as “low-level” laser therapy.
Electromagnetic waves vs. biophotons
Electromagnetic waves and biophotons are both part of the same electromagnetic spectrum, which includes a wide range of frequencies and wavelengths. However, the difference between them lies in the way they are generated and used. Electromagnetic waves are generated by various sources, including technical devices and natural phenomena such as solar radiation. Biophotons, on the other hand, are produced by living cells and tissues and therefore have specific biological significance.
Biophotons are believed to play an important role in the transmission of information in biological systems, including the control of metabolic processes and the regulation of cellular activities. The study of the properties of biophotons and their interactions with biological systems is an important area of research that can improve our understanding of fundamental biological processes.
Biochemical and biophysical effects relevant to wound healing.
The biochemical and biophysical effects of light depend on the wavelength. There are numerous clinically relevant processes that are increasingly being better researched and are also very interesting for the field of wound management in particular.
Promotion of angiogenesis [2,3]: Angiogenesis is the biological process by which new blood vessels are formed from existing ones. Light may play a role in the regulation of angiogenesis, particularly in wound healing. Studies have shown that red and infrared light can promote angiogenesis by increasing the production of growth factors and cytokines needed for the formation of new blood vessels. Infrared light can also increase blood flow and oxygen levels in tissues, which also helps to promote angiogenesis. In addition, light can also inhibit angiogenesis. Blue light, for example, can reduce the formation of new blood vessels by increasing the production of nitric oxide, which constricts blood vessels and reduces the rate of blood flow. Overall, light can affect angiogenesis in different ways, depending on the wavelength and intensity of the light and the specific conditions in the tissue.
blood flow promotion [4]: In the human body, nitric oxide is produced by the endothelial cells of blood vessels and acts as an important messenger that promotes relaxation of blood vessel muscles and dilation of blood vessels to increase blood flow. This helps regulate blood pressure and can also be used in the treatment of diseases such as angina, pulmonary hypertension or PAOD. Blue laser light promotes the formation of nitric oxide and can therefore be used effectively in wounds with impaired circulation, such as pAVK.
anti-inflammatory effects [5]: In addition, there is evidence that certain wavelengths, such as blue light, may also have an anti-inflammatory effect. This is thought to be due to blue light’s ability to scavenge free radicals, thereby reducing oxidative damage and inflammation.
Anti-infective effects [6]: Light therapy can also be used in the treatment of infections, whether viral or bacterial. In particular, blue light is used here. The therapy can be applied both with and without photosensitizer. Most recently, blue laser light is making a splash in the treatment of Covid-19.
Pain relief [7,8]: Light therapy, especially red light, has been successfully used for years in the treatment of both acute and chronic pain conditions. One can think of sports injuries or chronic back pain or fibromyalgia.
Improving the appearance of the skin [9,10]: Light therapy is used in the cosmetic industry as a non-invasive and gentle method to improve the appearance of the skin. Light therapy can be used alone or in combination with other cosmetic treatments such as chemical peels or microdermabrasion to improve results. It is a safe and painless method that requires no downtime, so patients can usually resume daily activities immediately after treatment. There are several types of light therapy that can be used for cosmetic purposes, including red light, blue light and green light. Red light is often used to stimulate collagen production and improve skin tightening. It can also be used to improve the appearance of fine lines and wrinkles and reduce inflammation and redness. Blue light therapy is often used to treat acne because it has antibacterial properties and can help reduce the bacteria responsible for causing acne. Green light can be used to reduce pigmentation spots and lighten skin discoloration. It can also help improve circulation and promote skin health.
Improve the function of mitochondria [11]: Mitochondria are the power plants of the cell and play an important role in energy production in our body. Light can affect mitochondrial function by interacting with them in various ways. Certain wavelengths of light, especially red and near-infrared light, improve mitochondrial function through positive action, particularly in the respiratory chain region. Increased energy production in the form of ATP enables and enhances multiple energy-dependent intracellular processes.
Influencing stem cells [12]: Light can affect stem cells through various mechanisms, such as activating enzymes that promote stem cell differentiation or modulating signaling pathways involved in the regulation of cell differentiation. It has been shown that light can promote stem cell proliferation and improve cell survival. For example, one study showed that irradiating stem cells with red and infrared light can increase their survival rate and promote their differentiation into neuronal cells. There is also evidence that light can enhance stem cell migration and promote their integration into tissue. This could potentially lead to new approaches in regenerative medicine that use light therapy to promote the activation of stem cells to repair damaged tissue.
Examples of modern forms of light therapy
Photomodulation and photodynamics are two different methods of light therapy. Photomodulation (also called low-level laser therapy or cold laser therapy) refers to the use of low-level laser or LED lights to stimulate or inhibit cells in the body. This type of therapy is used to treat pain, inflammation, muscle and joint problems, and to promote wound healing. Photomodulation usually uses red or infrared light.
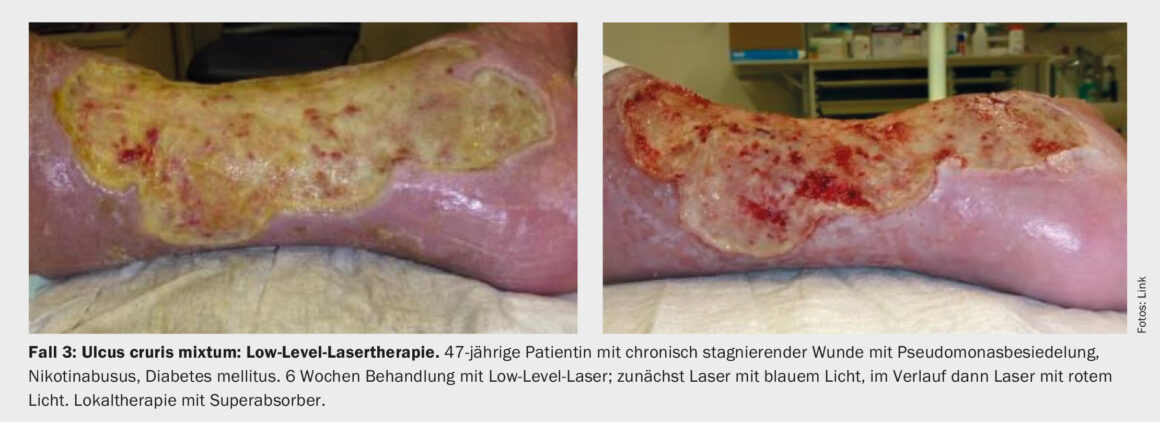
Case studies 1-3 show concrete clinical application possibilities in the field of wound management in acne inversa, venous leg ulcer and mixed leg ulcer.
Low-level laser therapy (LLLT), also known as cold laser therapy or weak laser therapy, is a form of laser therapy that uses a weak laser that has a low power in the milliwatt range. Unlike other types of lasers used to destroy or cut tissues, the low-level laser’s energy is too weak to damage cells or tissues. Instead, the laser light is used to stimulate or inhibit biological processes in cells. Low-level laser therapy is used in medicine to treat a variety of conditions, including pain, inflammation, arthritis, back pain, wound healing, neurological disorders, acupuncture, pain management, lymphedema, psoriasis and tinnitus. Laser therapy can also be used for cosmetic applications such as skin rejuvenation, cellulite reduction, hair loss and scar treatment.

The light from the low-level laser penetrates the skin and stimulates the mitochondria in the cells to produce ATP (adenosine triphosphate), which is necessary for energy production in the cells. This process can help repair and regenerate damaged tissue, promote circulation and reduce inflammation. Low-level laser therapy is a non-invasive, painless and safe treatment method that is usually without side effects.

Photodynamics, on the other hand, is a special form of light therapy in which a light-activated substance (photosensitizer) is applied or injected onto the body. The photosensitizer is taken up and accumulated by certain cells in the body. Subsequently, the tissue is irradiated with a light of a specific wavelength to activate the photosensitizer. This leads to the formation of oxygen radicals and other reactive oxygen species that can destroy cancer cells and other diseased tissues. Photodynamics is used primarily to treat cancer, but can also be effective for some bacterial infections and skin diseases.
Overall, both photomodulation and photodynamics use the positive effects of light on the body to treat disease.
Water-filtered infrared (wIRA) is a form of infrared radiation in which the radiation is modified by a special filtering process. The aim of filtering is to reduce the water vapor content in the air and thus achieve a higher penetration depth of radiation into the tissue. Furthermore, wIRA is less sensitive to skin surface coatings such as sweat and sebum and therefore allows for greater radiation efficacy when treating deeper tissue layers.
Take-Home Messages
- The majority of chronic wounds have vascular causes (e.g. venous leg ulcers, mixed leg ulcers). When the possibilities
of more complex reconstructive arterial interventions have been exhausted, alternative treatment options must be used. - Innovative light therapy options may be a gamechanger in the treatment of chronic stagnant wounds. The wide range of biochemical and biophysical effects of electromagnetic radiation is increasingly being researched and successfully applied clinically, including in the field of wound management.
- Light and laser therapy can be used to boost wound healing in a variety of ways. Depending on the wavelength and other parameters, the effects range from promotion of blood flow and angiogenesis, to anti-inflammation and pain relief, to improvement of mitochondrial function and other relevant processes.
- Modern methods of light therapy for indication areas in wound management include, for example, low-level laser therapy (LLLT), photodynamic methods and water-filtered infrared (wIRA).
Literature:
- Geng Z, et al: Advances in Visible Light Communication Technologies and Applications. Photonics 2022; 9(12): 893.
https://doi.org/10.3390/photonics9120893 - Dungel P, et al: Low level light therapy by LED of different wavelength induces angiogenesis and improves ischemic wound healing. Lasers Surg Med 2014; 46(10): 773-780.
- Rohringer S, et al: The impact of wavelengths of LED light-therapy on endothelial cells. Sci Rep 2017 Sep 6; 7(1):10700.
doi: 10.1038/s41598-017-11061-y. - Barolet AC, Litvinov IV, Barolet D: Light-induced nitric oxide release in the skin beyond UVA and blue light: Red & near-infrared wavelengths. Nitric Oxide 2021 Dec 1; 117; 16-25.
- Honmura A, et al: Therapeutic effect of Ga-Al-As diode laser irradiation on experimentally induced inflammation in rats. Lasers Surg Med 1992; 12(4): 441-449.
- de Matos BTL, et al: Photobiomodulation Therapy as a Possible New Approach in COVID-19: A Systematic Review. Life (Basel) 2021 Jun 18;11(6): 580. doi: 10.3390/life11060580.
- Ross G: Photobiomodulation Therapy: A Possible Answer to the Opioid Crisis. Photobiomodule Photomed Laser Surg 2019; 37(11): 667-668.
- Kisselev SB, Moskvin SV: The Use of Laser Therapy for Patients with Fibromyalgia: A Crit-ical Literary Review. J Lasers Med Sci 2019 Winter; 10(1): 12-20.
- Huang A, et al: Light emitting diode phototherapy for skin aging. J Drugs Dermatol 2020; 19(4): 359-364.
- Hamilton FL, et al: Laser and other light therapies for the treatment of acne vulgaris: systematic review. Br J Dermatol 2009; 160(6): 1273-1285.
- Hamblin MR: Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem Photobiol 2018; 94(2): 199-212.
- Amaroli A, et al: Near-Infrared 810 nm Light Affects Porifera Chondrosia reniformis (Nardo, 1847) Regeneration: Molecular Implications and Evolutionary Considerations of Photobiomodulation-Animal Cell Interaction. Int J Mol Sci 2022; 24(1): 226.
DERMATOLOGIE PRAXIS 2023; 33(2): 6–10











