A number of risk factors are known to be associated with hand eczema, but there are few population-level studies to date. Against this background, a research team in Finland conducted a survey as part of a large-scale non-interventional cohort registry study to find out more about the links between the occurrence of hand eczema and environmental and lifestyle factors, as well as atopic predisposition.
Hand eczema (HE) is considered a common work-related skin condition and has a significant impact on socio-economic aspects and quality of life [1–3]. In terms of pathomechanism, HE is an inflammatory disease with a chronic, recurrent course and multifactorial etiology. A history of atopic dermatitis (AD) is known to be an endogenous risk factor for HE, while wet work, exposure to irritants and contact sensitization are exogenous risk factors [4]. In previous studies, the risk factors for HE were mostly investigated in a cross-sectional design, but there is a lack of longitudinal data. And although AD is a known risk factor, the link between HE and other atopic diseases has not been extensively studied. Koskelo et al. attempted to fill this research gap. with their study based on the “Northern Finland Birth Cohort 1966 Study” register [4].
| Hand eczema (HE) was a common phenomenon in this middle-aged population. Atopic diseases, female gender, obesity and parental allergy were found to be significant risk factors for HE. HE was less common in people who reported moderate or high levels of physical activity. The study authors point out that it is important in clinical practice to consider all atopic diseases – not just AD – and also to take lifestyle factors into account as possible risk factors for HE. |
| according to [4] |
Study design
The entire data set of the “Northern Finland Birth Cohort 1966 Study” (NFBC1966) comprises 12,055 mothers with 12,058 children born alive in 1966 [4]. The latter were regularly followed up on the basis of health questionnaires and clinical examinations. Four large follow-up surveys were conducted when the cohort members were 1, 14, 31 and 46 years old. The parents of the cohort members were also followed up using national registers and medical reports [5,6]. As part of the 46-year follow-up, the study participants completed a comprehensive questionnaire containing 132 questions on physical health, lifestyle and environmental factors, as well as socioeconomic status (SES) [4]. The item on hand eczema (HE) was: “Do you have HE or have you ever been diagnosed or treated by a doctor?”. In addition, there were two questionnaire items each on asthma, allergic rhinoconjunctivitis and atopic dermatitis. Firstly, a self-assessment and secondly, an external assessment by a doctor, e.g. “Have you had asthma in the last 12 months?”/”Have you had asthma in the past?” and “Have you been diagnosed or treated for asthma by a doctor?”. The same questionnaire was used to collect information on the ownership of pets and livestock, mold exposure in the home and symptoms at home or at work related to mold exposure.
A questionnaire was sent to 10,321 study participants who lived in Finland and whose address was known. Of these, 66.2% were aged between 45 and 46 and answered the questionnaire. Of the respondents, 3715 (54.4%) were women. The analysis of the survey was published in the journal Contact Dermatitis in 2022 [4].
Results at a glance
Hand eczema was reported in 13.3% of the 6830 returned questionnaires. HE occurred more frequently in women than in men (16.1% vs. 10.0%) (OR 1.73; 95% CI: 1.49-2.0; p<0.001). HE was slightly more common in people with primary and secondary education (13.8%) than in people with tertiary education (12.6%), but this relationship was not statistically significant.
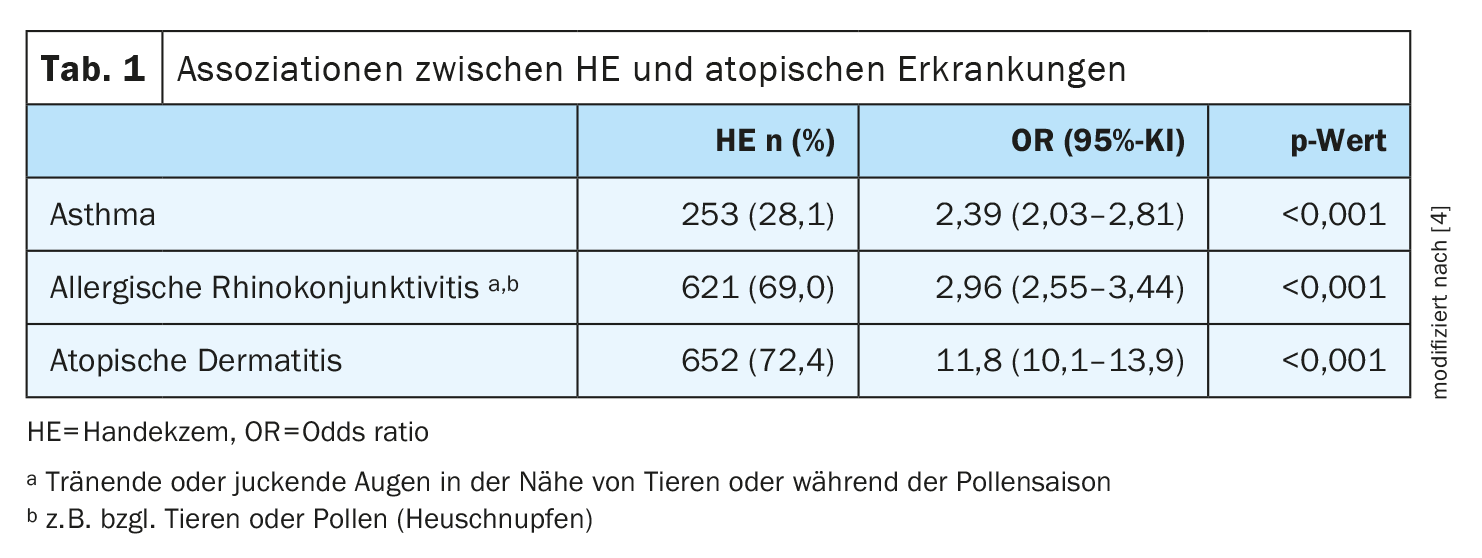
Atopic diseases: People with atopic diseases showed an increased risk of developing HE. There was a strong correlation between HE and asthma, allergic rhinoconjunctivitis and AD (each p<0.001) (Tab. 1). After adjusting for female gender, SES, BMI, maternal BMI, parental allergy, physical activity, living on a farm, mold exposure, and symptoms due to mold in a multivariable logistic regression analysis, all factors remained associated with HE. Even after further adjustment for AD, asthma and allergic rhinoconjunctivitis, the majority of other atopic diseases (AD, asthma and allergic rhinoconjunctivitis) remained associated with HE (p<0.001; p= 0.003 and p=0.02, respectively). Gender had no influence on the relationship between atopic diseases and HE.
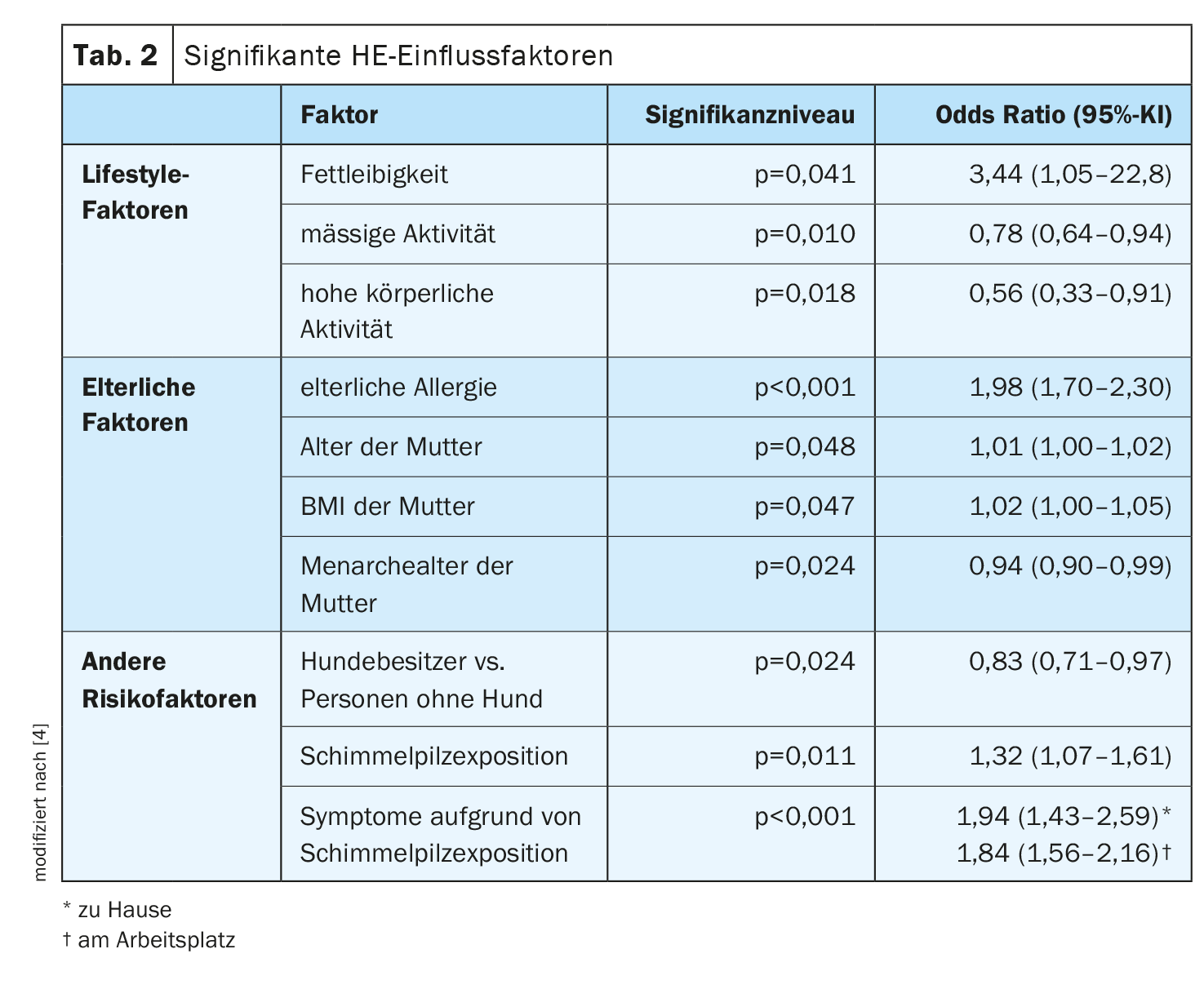
Lifestyle factors: Obesity was associated with HE (p=0.041) (Table 2) . Individuals who reported moderate or high physical activity had a lower risk of developing HE (p=0.010 and p=0.018, respectively) than those who were less active. HE was reported slightly more frequently by former and current smokers than by people who had never smoked, but this association was not statistically significant (p=0.193). People with moderate or heavy alcohol consumption were less likely to report HE than people with light alcohol consumption or never drinkers, but this association was not statistically significant (p=0.213).
Parental factors: Parental risk factors for hand eczema in offspring were also analyzed. It was found that a parental allergy significantly increased the risk of HE (p<0.001) (Table 2). Accordingly, maternal factors such as age, BMI and age at menarche also significantly increased the risk of HE in the offspring; i.e. the higher the expression of the parameters mentioned, the higher the risk (p=0.048, p=0.047 and p=0.024 respectively). There was no correlation between maternal tobacco smoking, parental asthma, birth weight, parity, gestational age and HE of the offspring.
Other risk factors: A comparison between pet and livestock owners and people who did not have animals showed that dog owners had a lower risk of HE than people without dogs (p=0.024) (Tab. 2). The risk of HE was slightly higher among cow farmers than among cow owners, but this did not reach statistical significance (p=0.403). There was no correlation with the keeping of other farm animals or cats and HE.
Those who reported seeing or smelling mold in their home had an increased risk of HE compared to those who had not come into contact with mold (p=0.011) (Tab. 2). And people who reported experiencing symptoms or becoming ill at home or at work due to mold exposure were more likely to have HE than those who did not (p<0,001).
Literature:
- Agner T, Elsner P: Hand eczema: epidemiology, prognosis and prevention. J Eur Acad Dermatol Venereol 2020; 34(S1): 4-12.
- Moberg C, Alderling M, Meding B: Hand eczema and quality of life: a population-based study. Br J Dermatol 2009; 161(2): 397-403.
- Vindenes HK, et al: Prevalence of, and work-related risk factors for, hand eczema in a Norwegian general population (the HUNT study). Contact Dermatitis. 2017; 77(4): 214-223.
- Koskelo M, et al: Risk factors of hand eczema: A population-based study among 900 subjects. Contact Dermatitis 2022; 87(6): 485-491.
- Nordström T, et al: Cohort profile: 46 years of follow-up of the northern Finland birth cohort 1966 (NFBC1966). Int J Epidemiol 2022; 50(6): 1786-1787.
- University of Oulu: Northern Finland Birth Cohort 1966. University of Oulu.
DERMATOLOGY PRACTICE 2024; 34(1): 32-34