Methylphenidate is an effective and safe agent in the treatment of ADHD. However, treatment should always be provided as part of a multimodal treatment plan.
The prevalence of attention-deficit/hyperactivity disorder (ADHD) in childhood and adolescence is comparable internationally and has been 3.5-5% for decades [1,2]. It is thus one of the most common disorders in child and adolescent psychiatry in general and a regular topic in the consultations of family doctors and pediatricians. The symptoms and consequences of ADHD affect school development, social interaction and also the entire family life. It is not always easy for the treating physicians to decide when which treatment is indicated. Within the framework of the guidelines, which provide for multimodal treatment, the indication of the various treatment steps is presented. Knowledge of symptomatology and diagnosis is critical for potential ADHD medication.
Clinical image
The core symptoms of ADHD are inattention, hyperactivity and impulsivity. Depending on the classification system, the symptoms all occur together (ICD-10; [3]) or as a presentation of predominant core symptoms, e.g., predominance of symptoms of inattention or hyperactivity-impulsivity (DSM-5; [4]). Decisive for the diagnosis are the impairment of everyday coping and the suffering caused by the symptoms.
The symptomatology often leads to discussions whether it is still age-appropriate “lively” behavior. The clarification should always consider various aspects. This includes a third-party assessment by parents and teachers, a self-assessment, and neuropsychological testing. Symptoms must have appeared before the age of seven (ICD-10) or before the age of twelve (DSM-5) and in different situations (school, leisure, family) and must have been present for at least six months. Intelligence and general development should be examined to rule out under- and overachievement. Somatic causes such as thyroid dysfunction, hearing and visual disturbances must be excluded. The diagnostic process also includes the survey of environmental conditions. Is the symptomatology aggravated by chronic quarreling in the family or bullying at school? Such factors must be reduced before opting for intensive therapy with medication [5]. Common comorbid or secondary disorders, such as anxiety disorders, depressive episodes, and social behavior disorder, as well as partial performance disorders (e.g., dyslexia), should be assessed to develop an individualized treatment plan. The presence of comorbid disorders is the rule, not the exception.
When is medication used?
After the diagnosis has been made, the child and the parents should be informed in detail about the disorder and the multimodal treatment (overview 1) , in accordance with the child’s age. Advantages and disadvantages of all non-drug and drug treatments will be discussed. Parents and child should have time to understand and weigh the information. If such a detailed consultation is waited for too long and only started when the “pressure in the system” is too great, parents often have the feeling that they were no longer able to decide freely, because, for example, school or after-school care was threatened.
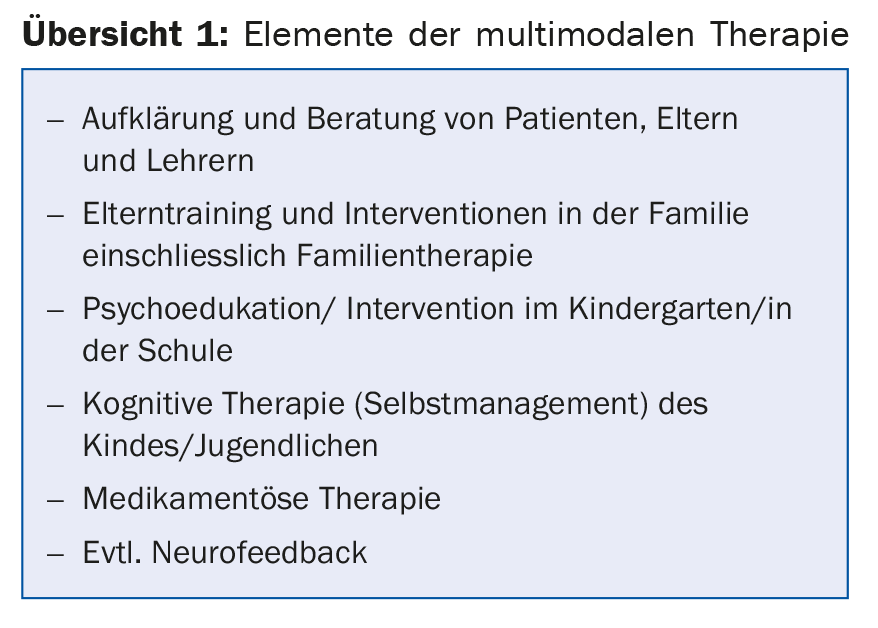
Medication is given only when the symptoms of ADHD are severe and other measures have failed to adequately support the child. This may mean that the child can no longer attend mainstream school without treatment, or may not meet class goals despite being gifted. It may mean that the disruptive behaviors are so pronounced that a child cannot be socially integrated. Treatment is always based on current guidelines [6,7].
Medication options in a multimodal treatment plan.
If the symptomatology is less pronounced, but the child is not able to complete homework in a reasonable time, for example, despite good working conditions, behavioral therapy methods should be used first (self-instruction training, reinforcement plans). When hyperactive behavior occurs in conjunction with oppositional and aggressive behavioral disorders in the classroom, a combination of school-based interventions by the teacher, self-management techniques (especially in older children and adolescents), and adjunctive pharmacotherapy should be sought. If these externalizing behavior disorders also occur within the family, family-centered interventions should be added. If the difficulties occur exclusively in the family context, it can be assumed that they are perpetuated by the family conditions. In this case, educational and psychological measures and possibly professional support within the family should precede or be combined with pharmacotherapy. In cases with severe impairment, medication is an effective way to quickly and sustainably reduce the pressure of suffering and to enable further educational and therapeutic measures – and above all a positive educational and social development of the child.
Choice of medication for ADHD
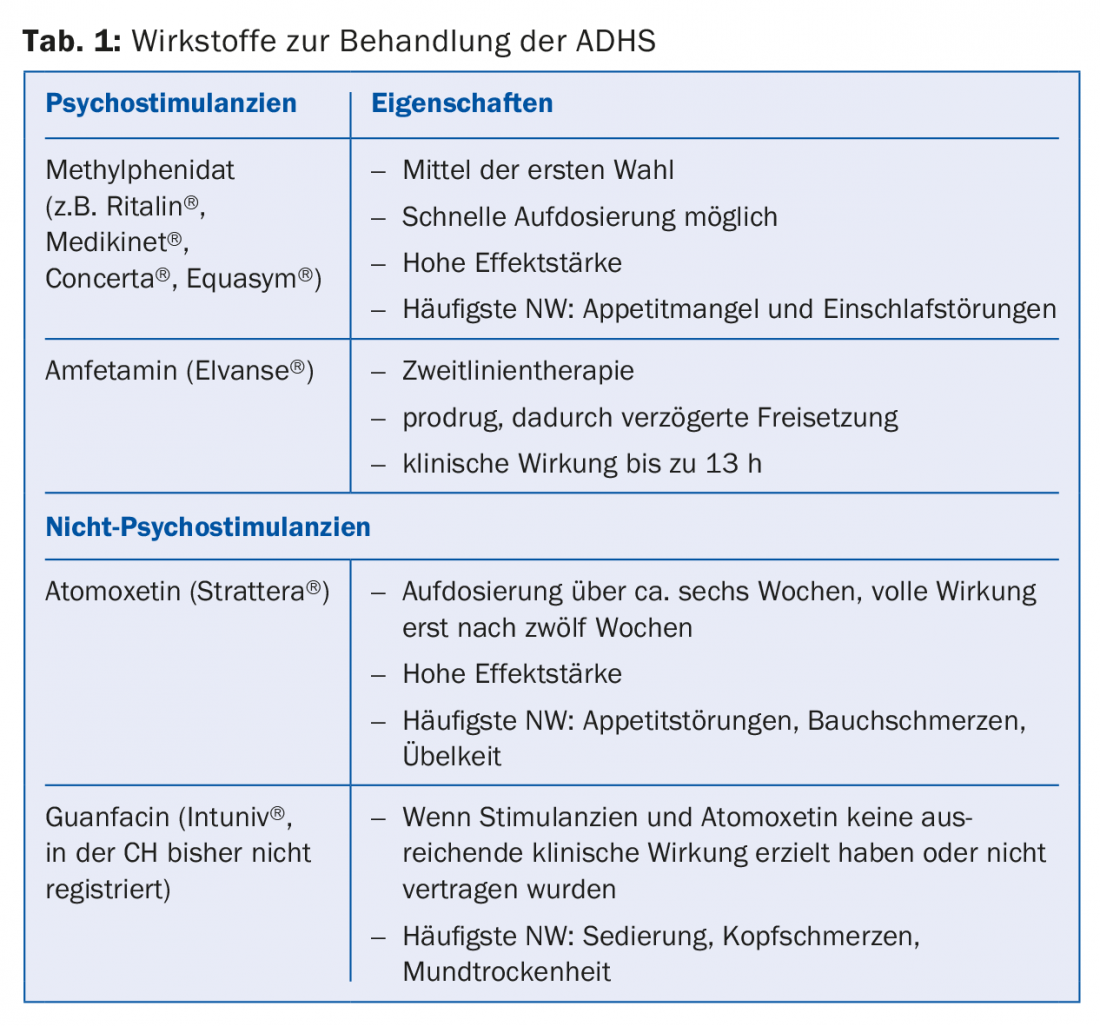
The drug of first choice is the narcotic (BTM)-required stimulant methylphenidate (MPH), most commonly known as Ritalin® (approved from the age of six for the treatment of ADHD).
Second-line medications include lisdexamfetamine, atomoxetine, or guanfacine when MPH is not sufficiently effective or side effects require a change in agent. Stimulants as well as atomoxetine and lisdexamfetamine have a level of evidence I for the treatment of ADHD [8].
Short-acting MPH (duration of action approx. four hours) is dosed within one to two weeks and achieves the desired effect in approx. 80% of patients [9,10]. After adjustment of the individual dosage (0.5-1 mg/kg/KG), the patient should usually be switched to a retard preparation. Depending on the product, an effect of eight to twelve hours is possible.
Second choice is the non-BTM atomoxetine, a norepinephrine reuptake inhibitor that achieves a 24-h sustained effect. After a longer dosing phase, the full effect unfolds after about twelve weeks. Lisdexamfetamine is also subject to BTM and has been approved in Switzerland since March 2014 for the treatment of ADHD in children and adolescents. It is a so-called prodrug, which is only hydrolyzed to the active substance in the body. This results in a significant time delay of the maximum drug concentration and a clinical duration of action of up to 13 hours.
Effect and side effect of MPH
The current Cochrane analysis [11] basically confirms the very good efficacy of MPH. Appetite and sleep disturbances are common, but the side effects are considered to be of little overall danger. The quality of the available studies and meta-analyses is criticized, especially with regard to their study design. For its part, however, the Cochrane analysis has attracted much criticism.
Gerlach et al. [10] indicate that treatment with MPH has not only been shown to be clinically successful over a long period of time, but has also been able to reduce comorbid disorders (e.g., depression, addictive disorders, trauma sequelae). Furthermore, to date, non-pharmacological treatment options have not been sufficiently effective in most cases. Weight, growth, pulse and blood pressure should be checked regularly while under medication. The adverse effects mostly occur in a dose-dependent manner. The lack of appetite also subsides as the effect wears off, and the children then usually have more appetite again in the afternoon. If the parents adjust to this with an appropriate snack, the weight can usually be kept stable. In case of new onset of sleep disturbances, it is advisable to check the time of intake and possibly bring it forward.
New strategies
Relatively new is the treatment with sustained-release guanfacine. The European Medicines Agency approved it in September 2015 for the treatment of ADHD in children aged six and older. Guanfacine is not a stimulant. It was developed as an antihypertensive and has a blood pressure lowering effect. Treatment may be given when treatment with stimulants (methylphenidate, amfetamine) is not an option, was intolerable, or proved ineffective. Treatment with guanfacine may also be considered for comorbid tic disorders. Side effects, in addition to blood pressure lowering, are mainly sedation and dry mouth.
What are the limitations of drug treatment?
Unfavorable school and psychosocial conditions in the family, which can hardly be changed, influence the success of drug therapy. However, they should not discourage it. The child must not be deprived of the opportunity for positive development. If adverse drug reactions persist (e.g., lack of appetite, difficulty falling asleep, headache, high blood pressure), the dose should be monitored and adjusted, the preparation changed if necessary, and a change of active ingredient attempted in the next step. Serious side effects that prevent drug treatment are very rare. A pre-existing tic disorder is not a contraindication; it can very rarely be aggravated by psychostimulants, and can also be ameliorated, especially with atomoxetine and guanfacine.
If the adolescent and/or parents or persons living in the household have known or suspected substance abuse, stimulants requiring BTM should not be prescribed in order to prevent the risk of abuse. For parents who themselves have untreated ADHD or other mental disorders, compliance must also be conscientiously assessed.
Table 1 summarizes the agents used to treat ADHD.
Take-Home Messages
- Methylphenidate is an effective and safe agent in the treatment of the core symptomatology of ADHD.
- Treatment should always be given only as part of a multimodal treatment plan.
- The diagnosis of ADHD and comorbid disorders should be made or reviewed by an experienced child and adolescent psychiatrist or pediatrician.
- “Trial medication” to verify the diagnosis should be avoided.
Literature:
- Polanczyk GV, et al: Annual Reaseach Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 2015; 56(3): 345-365.
- Polanczyk GV, et al: ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol 2014; 43(2): 434-442.
- Dilling H, et al. (Eds.): International classification of mental disorders; ICD-10 chapter V (F) – Clinical diagnostic guidelines. Bern: Huber 2016.
- American Psychiatric Association: DSM-5 Diagnostic and statistical Manual of Mental Dis- orders;4th ed. Washington DC: American Psychiatric Press 2013.
- Walitza S: ADHD in children. Diagnosis and therapy. InFo Neurology & Psychiatry 2012; 10(3): 14-17.
- German Society for Child and Adolescent Psychiatry: Guidelines for diagnosis and treatment of mental disorders in infancy, childhood and adolescence: ADHD in children, adolescents and adults. 2007. revised 2014. New version expected in 2017. www.dgpjp.de
- National Institute for Health and Clinical Excellenc (NICE): Methylphenidate, atomoxetine and dexamfetamine for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Technology appraisal guidance [TA98]. London: NICE 2006. www.nice.org.uk
- Walitza S, Berger G: (New) medications for ADHD. Pediatricians Switzerland 2016; (1): 22-23.
- Walitza S, et al: Psychostimulants and other drugs used in the treatment of attention-deficit/hyperactivity disorder (ADHD). In: Gerlach M, et al. (Eds.): Neuro/psychotropic drugs in childhood and adolescence. 3rd ed. Berlin: Springer 2016; 289-331.
- Gerlach M, et al: What are the benefits of methylphenidate as a treatment for children and adolescents with attention-deficit/hyperactivity disorder? ADHD Atten Def Hyp Disord 2017; 9: 1-3.
- Storebø OJ, et al: Methylphenidate for attention-deficit/hyperactivity disorder in children and adolescents: Cochrane systematic review with meta-analyses and trial sequential analyses of randomised clinical trials. BMJ 2015; 351: h5203.
HAUSARZT PRAXIS 2017; 12(8): 15-18