At the 2017 joint annual meeting of the Swiss Society of Paediatrics (SSP) and the Swiss Society for Allergology and Immunology (SSAI), PD Dr. Kathrin Scherer, Dermatology, University Hospital Basel, spoke about problems in skin prick testing, intradermal testing and patch testing of patients with allergies. She gave a practical update on the questions: How to test? Where to test? Test with what?
Skin testing for allergies is significantly influenced by the diagnostic technique (test instruments and their handling), by the immunological situation of the patient (general and local at the skin test site), and by the allergen preparation (concentration, standardization).
How to test?
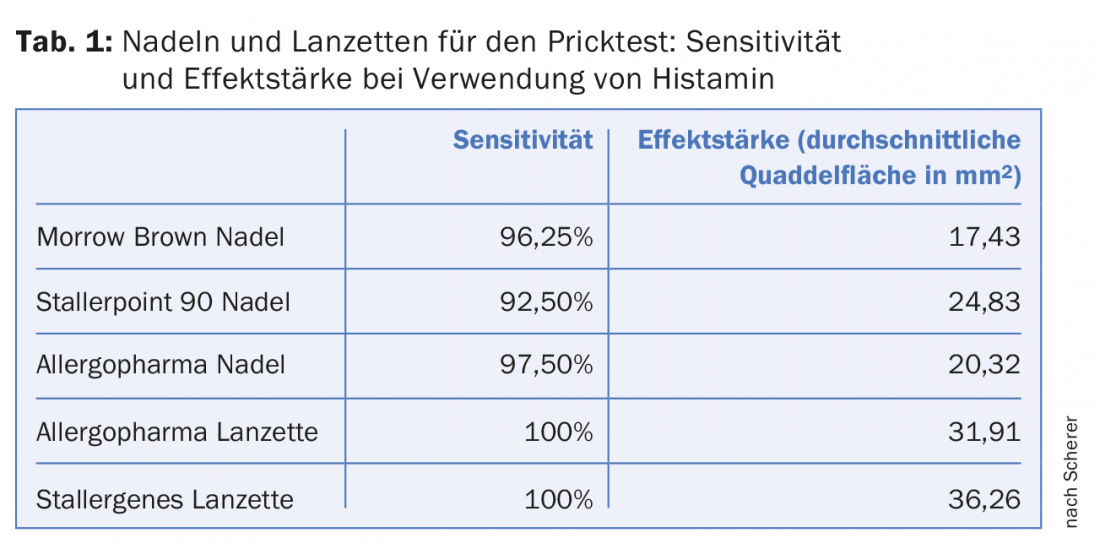
The effect size of skin prick tests depends on the test instrument used, the speaker reported. Lancets are superior to needles in terms of sensitivity and efficacy, but are more difficult to handle. The technique recommended by the manufacturer must be followed carefully when handling all test instruments in order to obtain good results. Even small variations in handling can cause variations in the size of the wheal. In a comparative study of three different prick test needles and two lancets conducted in Basel, the lancet from Stallergenes resulted in the largest wheals (using histamine volar on the forearm). Both lancets yielded larger wheals than the needles (Tab. 1). Testing was performed on the forearm and upper back of 20 medical student volunteers with histamine 1%, codeine phosphate 9%, and NaCl 0.9% (negative control). Sensitivity was slightly lower with prick test needles than with lancets. Larger wheals were obtained with histamine than with codeine. Histamine wheals were significantly larger on the forearm than on the upper back.
Prick test results are more positive on the volar forearm than on the upper back. This is likely due to the difference in mast cell density at the two test sites. Calculation of mast cell density resulted in considerable differences between the forearm (mast cell density total 211 mast cells per mm2, in papillary dermis 120 mast cells per mm2) and the upper back (total 172, in papillary dermis 70 per mm2) [1]. These calculations are based on punch biopsies taken from various body sites. The greatest mast cell density was found on the nose and the whole head, slightly lower on the hands and feet, followed by the forearms, the upper back, and finally the abdomen [1]. Different from prick testing were the results of a study with intradermal testing conducted in Basel in 24 volunteers [2]. Here, larger wheals resulted on the upper back than on the volar forearm and lateral upper arm. Moreover, codeine resulted in larger wheals than histamine. These differences between prick test and intradermal test results cannot be fully explained, she said.
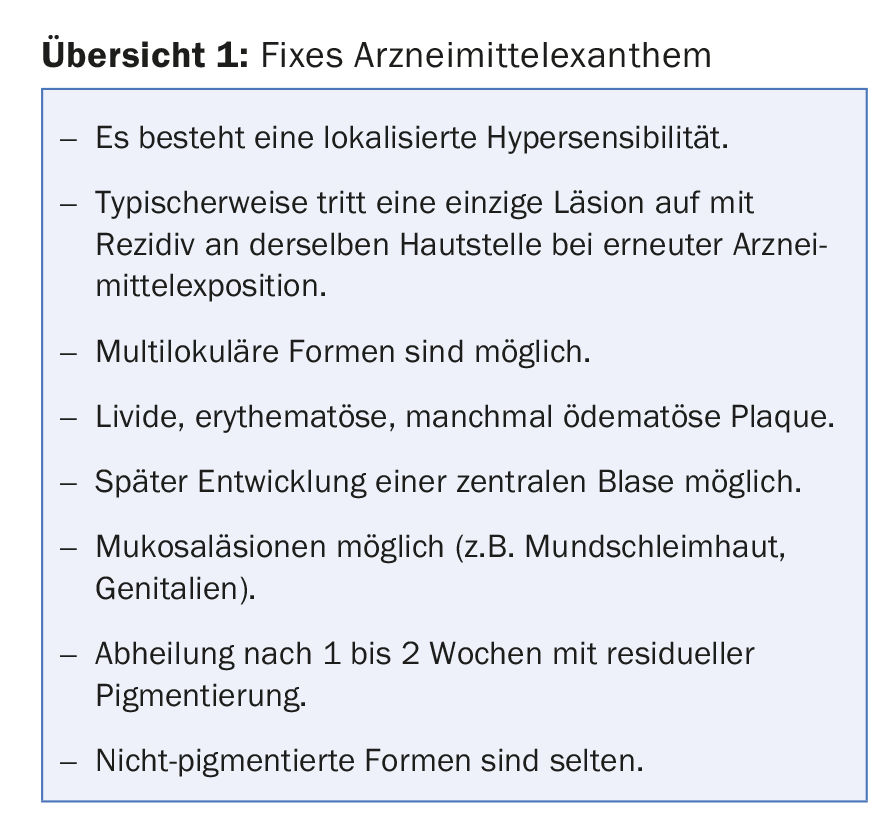
Patch tests to clarify delayed reactions are usually performed on the upper back. An exception to this rule is testing for fixed drug exanthema. Patch testing in the lesional skin area is considered more sensitive in fixed drug exanthema (Overview 1) compared with testing on the upper back. Therefore, due to the higher skin sensitivity, testing should be performed at the site of the original clinical lesion (possibly in addition to testing at the upper back).
The sensitivity of testing in lesional, pigmented skin is 40% to 50%, especially when testing nonsteroidal anti-inflammatory drugs (NSAIDs), she said. In Portugal, 52 cases (period 20 years) were retrospectively analyzed [3]. The trigger of fixed drug exanthema was clinically suspected to be NSAID in 90.4%. In 21 patients (40.4%), patch testing was reactive in lesional pigmented skin. In 20 of these patients, an NSAID (nimesulide, piroxicam, etoricoxib) was the responsible drug, and in one patient, the antihistamine cetirizine [3]. Similar to fixed drug exanthema, testing at the site of the strongest clinical reaction may be useful for certain other exanthems, the speaker reported. It is possible that the response of resident memory T cells is more active than that of circulating memory cells. Dr. Scherer demonstrated this with the example of an SDRIFE case after radiographic contrast agent administration (symmetrical drug related intertriginous and flexural exanthema). Patch testing with x-ray contrast on the upper back remained negative, as did intradermal testing with a late reading on the upper arm. In contrast, lesional intradermal tests with late reading were positive.
Test with what?
In skin testing, it is important to distinguish between irritant and true allergic reactions, especially when testing immediate-type allergies to substances that can cause skin irritation. Negative controls are helpful in testing. Irritating substances such as rifampicin or ciprofloxacin complicate the interpretation of intradermal test results. Very different non-irritative test concentrations are reported in the literature for ciprofloxacin, for example, the speaker reported. She drew attention to the fact that in practice, home-made dilutions are often inaccurate. More accurate results than with dilutions in the syringe can be achieved with dilution ampoules, he said. Test concentrations should be chosen differently depending on the initial clinical response. Lower skin test concentrations are generally recommended for immediate-type allergies than for delayed-type reactions. For example, intradermal testing with heparin for immediate type reactions is performed with 1:100 or 1:10 dilutions of the drug. In contrast, for delayed-type reactions, it is recommended to test with the undiluted drug. “When we test highly allergic patients, we need to be sure we are testing at concentrations that are not dangerous,” the speaker said.
Source: SSP/SSAI Joint Annual Meeting 2017, St. Gallen. Lecture: Kathrin Scherer, University Hospital Basel: “What’s new in allergy skin testing?”, June 1, 2017.
Literature:
- Weber A, et al: Pattern analysis of human cutaneous mast cell populations by total body surface. Br J Dermatol 2003; 148: 224-228.
- Scherer K, et al: Reaction pattern to histamine and codeine in a human intradermal skin test model. Clin Exp Allergy 2007; 37: 39-46.
- Andrade P, et al: Patch testing in fixed drug eruptions: a 20-year review. Contact Dermatitis 2011; 65: 195-201.
DERMATOLOGIE PRAXIS 2017; 27(4): 46-47











