Safe contraception is a need for millions of people and a key contributor to improving women’s health. Every year, 70,000 women die as a result of unplanned, unwanted pregnancies and unsafe abortions. Doctors, especially gynecologists, are the experts on contraception. However, contraceptive counseling has become more complex, on the one hand with the variety of options, on the other hand also with the publications about the thromboembolic risk of the pills and the obligation to provide correct and comprehensive information.
For women of fertile age, unprotected sex, lack of access to contraceptives, and iron deficiency anemia are the three leading causes of death [1]. Medical advice is highly valued, as shown by the recently published BzGA study from Germany: teenagers want information about sexual issues primarily from doctors, and in the eyes of many adolescents, doctors are even more important as a source of information than parents, teachers or friends [2].
The importance of hormonal contraception
Approximately 80 million women worldwide use hormonal contraceptive methods, reflecting their importance to population health today. In recent months, however, many critical voices have been raised, especially regarding combined hormonal contraception and its risks, so that Swissmedic [3] and the SGGG [4] have published a summary of the current data situation and recommendations. This article is intended to provide the family physician with the tools for practical implementation.
Combined hormonal contraceptives: pill, patch and ring
Combined hormone preparations are those that contain both an estrogen and a progestin. The dosage form can be oral as a pill, transdermal as a patch or intravaginal as a ring.
While a wide range of different progestins, dosages, regimens and estrogens are available for the oral form, only one preparation each is available on the market for both the transdermal and intravaginal forms. Intravaginal contraception with the vaginal ring (EE, ethonogestrel) and transdermal application with the patch (EE, norelgestromin) may be advantageous, particularly with regard to compliance, and may also be used in the initial prescription. The progestins of both preparations belong to the so-called third generation.
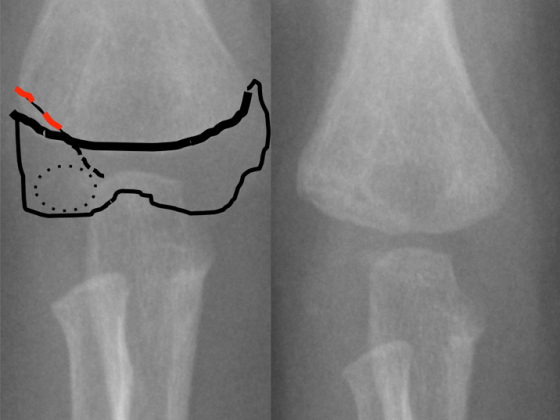
All combined preparations increase the risk of thromboembolism, although to varying degrees. However, the relative risk is lower than during pregnancy (Fig. 1).

Estrogen is primarily responsible for this increase in risk through its influence on liver metabolism. However, progestogens also influence blood clotting, which depends not only on the type of progestogen but also on its dosage, dosage form, and the presence and type of estrogen. This explains the importance of the choice of progestogen for the risk of thrombosis of combined pills.
In contrast, progestogen-only methods do not increase the risk of thrombosis according to current knowledge. This refers to the estrogen-free pill, the subcutaneous implant, and the intrauterine hormone systems Mirena® or Jaydess®. However, depot injection of MPA (three-month injection) should be used with caution in cases of increased cadiovascular risk or hypertension, as it may adversely affect the vascular situation, particularly in the arterial limb.
The consultation
In order to counsel the patient with a desire for a contraceptive, the physician requires a range of information. According to the Zurich Discussion Group, “In principle, before prescribing hormonal contraceptives (pill, vaginal ring, patch, injection, implant, IUS), a detailed personal and family history should be taken and risk factors, e.g., thrombophilia, liver disease, dyslipidemia, smoking, obesity, anorexia, competitive sports, and hypertension, should be assessed” [5].
The family history
According to current studies , a positive family history increases the risk of thromboembolism, independent of the presence of other risk factors. However, family history correlates less with known genetic thrombophilias. This means that even if the laboratory test is unremarkable, a positive family history must be included in the consultation as a risk factor. Unfortunately, it has not yet been clarified what is meant by a positive medical history. It is open whether, in addition to unprovoked thromboembolism of a first-degree relative, second-degree relatives, relatives of older age, and so-called provoked thromboembolism, such as after surgery, the puerperium, or air travel, should also be included.
Laboratory examination
Since the ruling in Austria, according to which every patient must be informed of the possibility of a thombophilia screening before a pill is prescribed, the indication for laboratory testing is also discussed here again and again. In addition to a positive self-reported history or known family history of thrombophilia, a positive family history should also be considered an indication. On the other hand, the SGGG and the DGGG do not recommend general screening before prescribing combined oral contraception (COC), as the costs would exceed the benefits. Also, an unremarkable screening result may provide a false sense of security because other risk factors are not included in it. If a patient requests a blood test, care must be taken to ensure that it is carried out correctly, including with regard to the collection and dispatch of samples. In these cases, the examination is not a mandatory benefit of the insurance company, which should be pointed out to the patient in advance.
Age
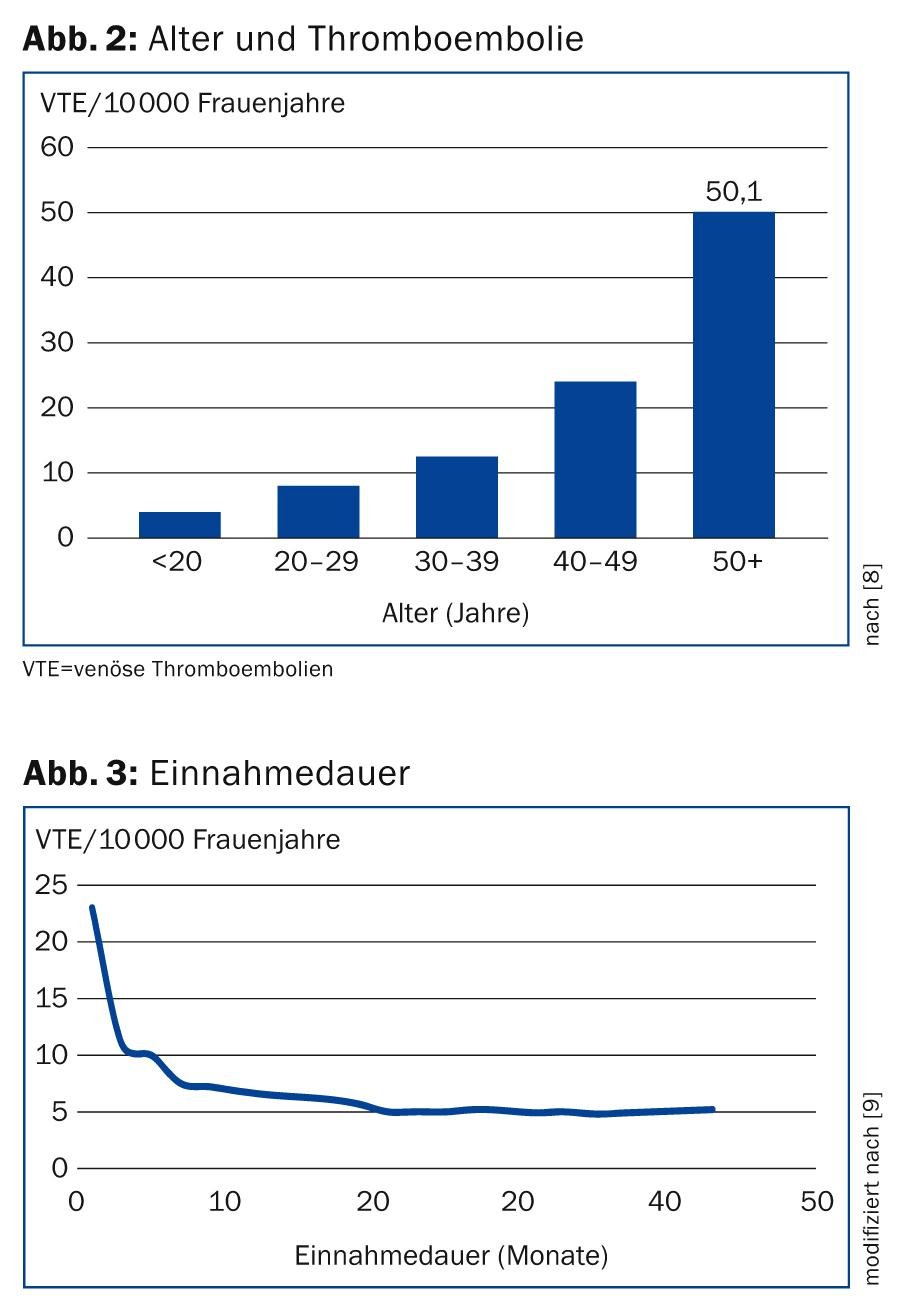
The patient’s age should be included in the consultation as a major risk factor. As shown in Figure 2, the vast majority of thromboembolism occurs beyond the fertile age and is therefore independent of contraception. In women seeking contraception, age must be considered but does not form an absolute contraindication to COC without an additional risk factor. In individual cases, it is acceptable to continue the pill until the onset of menopause if the patient has no other risk factors and wishes to do so. However, it is important to point out the general age-related increase in the risk of thrombosis. A new start is more critical, since the duration of use has a decisive influence on the incidence of thrombosis.
Incidence of thrombosis according to duration of use
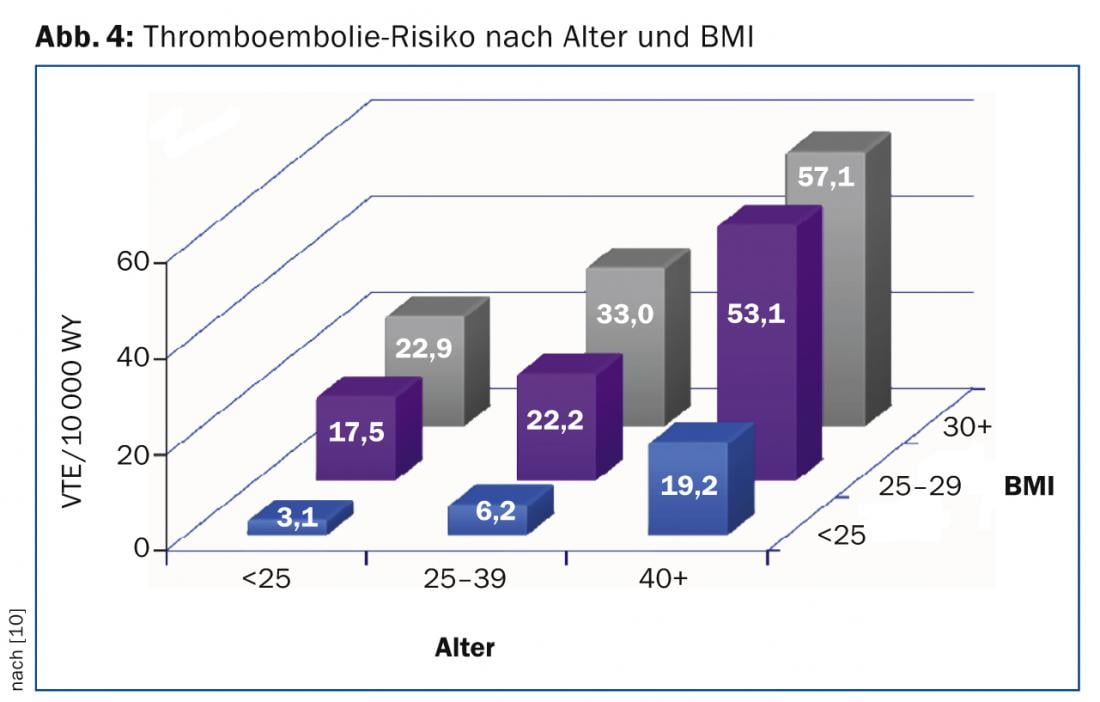
The duration of use has a significant impact on the incidence of thrombosis. Thus, more than half of thromboses under OC occur in the first six months, and most frequently in the first three months. Therefore, especially when a pill is prescribed for the first time, the patient must be informed of possible symptoms of thrombosis or pulmonary embolism (Fig. 3).
Teenagers
A special counseling situation arises for adolescents, who differ from adults in various ways and require different priorities.
The desire for safe contraception and counseling should be supported in all cases and adolescents encouraged to do so.
For adolescents in particular, the benefits of contraception far outweigh the risks. Nevertheless, the indication must be made carefully even in young female patients.
Negative associations should be avoided, as they have an unfavorable impact on compliance. Although the risks of hormonal contraception should be discussed and symptoms of complications mentioned, the positive effects of the pill should be in the foreground. Adolescents need confidence in the method they are using on a daily, weekly, or monthly basis; irregular use is not a viable method.
During counseling, STI should be discussed and the condom recommended in addition to contraception.
The main part of the information we give to adolescents should be related to the concrete use of the contraceptive method, such as starting the method, procedures in case of forgetting, in case of vomiting or in case of side effects.
For adolescents under 16 years of age who want the pill without parental guidance, judgment must be assessed and recorded in the medical record.
Obesity
Overweight and obesity are independent risk factors that must be considered in counseling. Especially for women with BMI above 35, intrauterine contraception is often recommended (Fig. 4).
Which pill for which patient?
Actually, it’s quite simple. According to SGGG and Swissmedic, a second-generation preparation should always be used in the first prescription, i.e. a preparation containing LNG. For adolescents under 18 years, a preparation with 30 μgEE is recommended. Now, however, the consultation is usually a bit more complex, because women bring different conditions with them. Therefore, the differences between the preparations and their indications are highlighted here.
The estrogen component: Today, in addition to ethinylestradiol (EE), the natural estrogens estradiol (E2) and estradiol valerate (E2V) are available for combined contraception. The two available preparations are the four-phase pill Qlaira® (E2V, Dienogest) and the single-phase preparation (24/4 ininnamate regimen) Zoely® (E2, NOMAC, approved for women 18 years and older).
Estradiol and estradiol valerate, unlike EE, show less pronounced metabolic effects and weaker induction of individual estrogen-dependent proteins. To what extent this will prove favorable in the clinic remains to be seen; until then, the same contraindications apply as for preparations with EE.
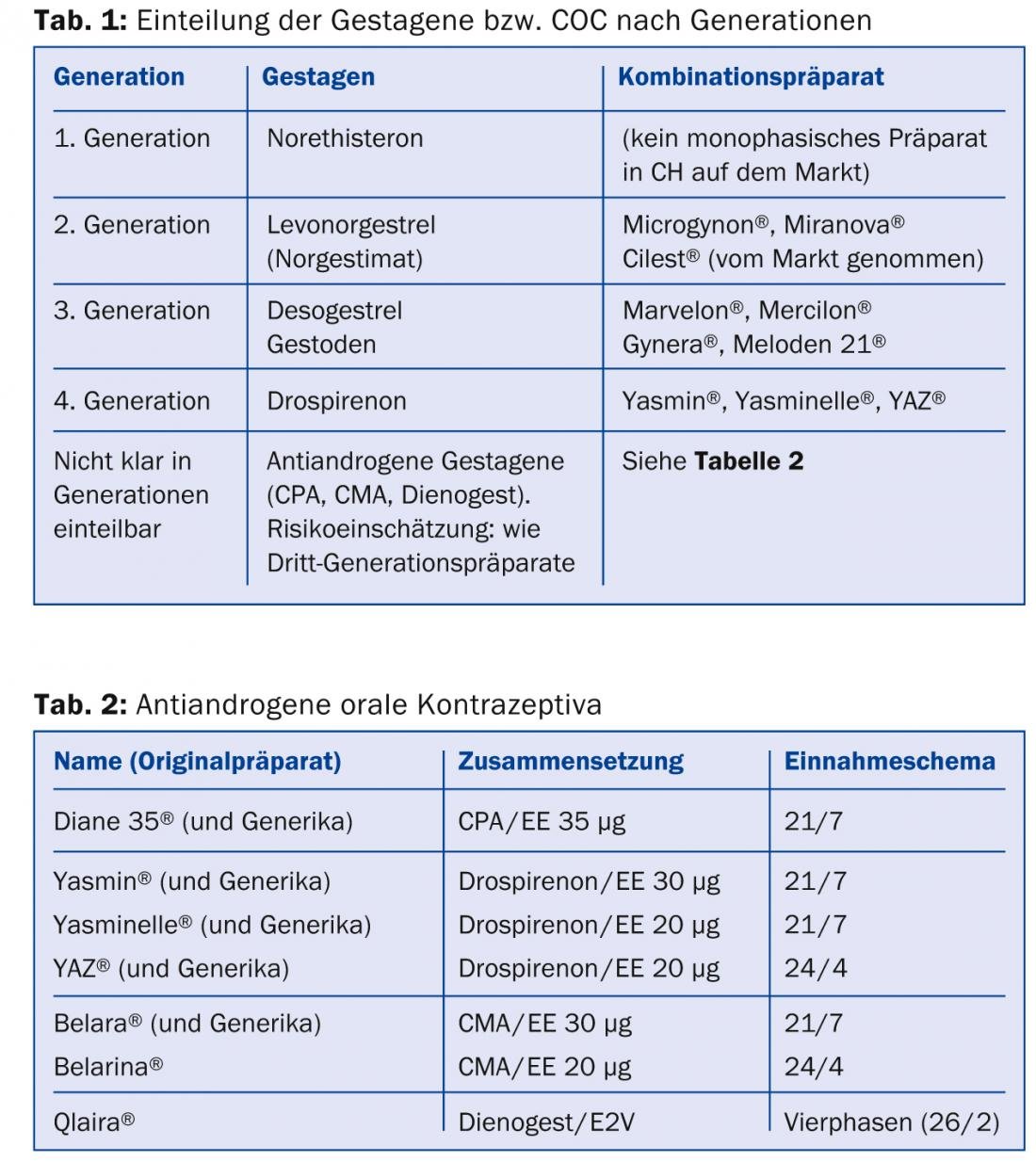
The progestogen component: Progestogens comprise a larger number of quite different substances. They can be classified according to their origin, their partial effects or receptor activity or also according to so-called generations, which refer to the time of their market introduction and not to a property per se. (Tab. 1). Although the further development of progestins from the second to the third generation was accompanied by a number of favorable properties, it led to a slight increase in the risk of thromboembolism according to current knowledge. Similarly, the antiandrogenic combination pills appear to have a higher risk of thrombosis. For example, recent studies in large numbers of patients show an increase in relative risk by a factor of 1.6-2 for third- and fourth-generation progestogens and antiandrogenic pills, respectively (Fig. 4), compared with the levonorgestrel-containing pill. However, the second-generation pill showed the greatest increase in risk at 50 μgEE, demonstrating the importance of estrogen (Fig. 5).
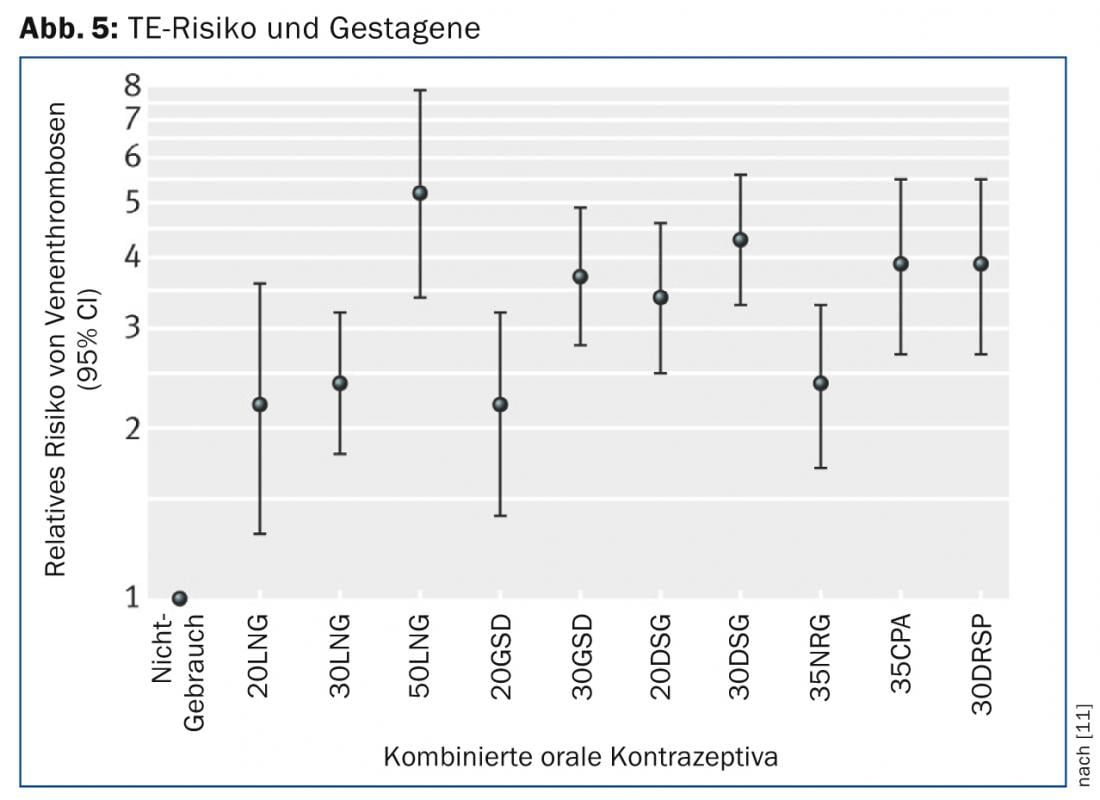
The recommendation to generally select a second-generation preparation as the first prescription is derived from these studies. However, it is permissible to choose an antiandrogenic preparation, a third-generation preparation, or a transdermal or intravaginal route if indicated and informed. If side effects occur, it is possible to switch to another preparation on the occasion of the second control, which reduces the initial risk according to current knowledge. An intake regimen 24/4 (24 monophasic pills, 4 placebos) results in a shortened pill break with less hormonal fluctuation, which can be used therapeutically for premenstrual syndrome [6]. According to the SGGG recommendation, justification should be provided in the medical record if a pill other than a second-generation pill is chosen.
The specific recommendation is:
- Initial prescription for uncomplicated patient: 2-generation pill LNG, 30 or 20 μgEE.
- Desire for natural estrogens: Qlaira®, Zoely®
- In case of acne, seborrhea, hirsutism: antiandrogenic pill (Tab. 2), or if only mild symptoms, impure skin: possibly third-generation pill (after clarification risk of thrombosis)
- Compliance problems with daily intake: Nuvaring®, Evra® patch
- Compliance problems with the intake break: 24/4 regimen: Belarina®, YAZ®, Zoely®, possibly Qlaira®.
- PMS, PMDD: YAZ®, possibly Belarina® (24/4 regimen).
- Hypermenorrhea: Qlaira®.
- Intermediate bleeding: 30 mcgEE.
Ruth Draths, MD
Literature:
- Word Health Organization: www.who.int/reproductivehealth/publications/family_planning/en/
- Adolescent sexuality: representative repeat survey of 14- to 17-year-olds and their parents. BZgA Cologne 2010.
- Swissmedic: Ärztezeitung 2014; 95: 105. www.swissmedic.ch.
- SGGG: www.sggg.ch/Expertenbrief 35. www.sggg.ch.
- Birkhäuser M, et al: Gynecologist 2012; 53(9): 846-849.
- Rapkin AJ: J Reprod Med 2008; 53: 729-741.
- ACOG Committee Opionion Number 540: Obstet Gynecol 2012; 120: 1239-1242.
- Rabe T, et al: J Reprod Endocrine 2012; 9: 20-63.
- Dinger J, et al: Eur J Contracept Reprod Health Care 2010; 15 (Suppl 1): 43.
- Dinger J: Abstract Congress European Society of Contraception, Prague 2008.
- Stegeman, et al: BMJ 2013; 347: f5298.
CONCLUSION FOR PRACTICE
- Before each prescription of a pill, a detailed consultation and education is mandatory.
- All combined preparations increase the risk of thromboembolism, but to varying degrees.
- Estrogen is primarily responsible for this increase in risk, but progestins also influence blood clotting.
- According to current knowledge, progestogen-only methods do not increase the risk of thrombosis.
- Positive family history, overweight, obesity, and age are independent risk factors that must be considered.
- In the initial prescription, a second-generation preparation is recommended without additional indication.
HAUSARZT PRAXIS 2014; 9(5): 34-38