From the large cardiovascular endpoint studies EMPA-REG, CANVAS, and DECLARE, it is clear that SGLT2 inhibitors have a beneficial effect on heart failure. This was confirmed in the DAPA-HF study.
Compared with placebo, there was a significantly higher rate of reduction in cardiovascular mortality and acute heart failure, as reported by Prof. Roger Lehmann, MD, University Hospital Zurich [1]. These beneficial effects occurred consistently across all age groups and were statistically independent of diabetes status and general health [2,3].
Evidence of risk reduction from cardiovascular outcome studies.
Heart failure is a common, limiting complication of diabetes and increases the risk of mortality [4,5]. It is well established that different glucose-lowering drugs have different effects on heart failure risk [4,5]. In the EMPA-REG OUTCOME study, the relative risk reduction in heart failure-related hospitalization in type 2 diabetes patients treated with empagliflozin was 35% [6]. A risk reduction of 33% was demonstrated in the CANVAS study [7] and 27% in the DECLARE-TIMI study [8]. Based on these results, the following questions, among others, arise: Which forms of heart failure are positively influenced? Do the beneficial effects of SGLT2 inhibitors also occur in patients with established heart failure? Can non-diabetics with heart failure also benefit from the beneficial effects?
Need for optimized treatment options
In the aforementioned cardiovascular end point studies, 58 subjects had a diagnosis of heart failure at baseline. No further details on the heart failure phenotype have been reported [6–8]. That diabetes and prediabetic dysglycemia are very common in heart failure patients and are associated with an increased risk of cardiovascular mortality and hospitalization for heart failure is well known [9,10]. Consequently, there is a need for evidence-based treatment options that are both glucose-lowering and improve heart failure outcomes and, if possible, do not lead to weight gain or increased risk of hypoglycemia [2]. Previous findings suggest that the beneficial effects of SGLT2 inhibitors also occur in heart failure patients without manifest dysglycemia [2].
DAPA-HF study delivers forward-looking results
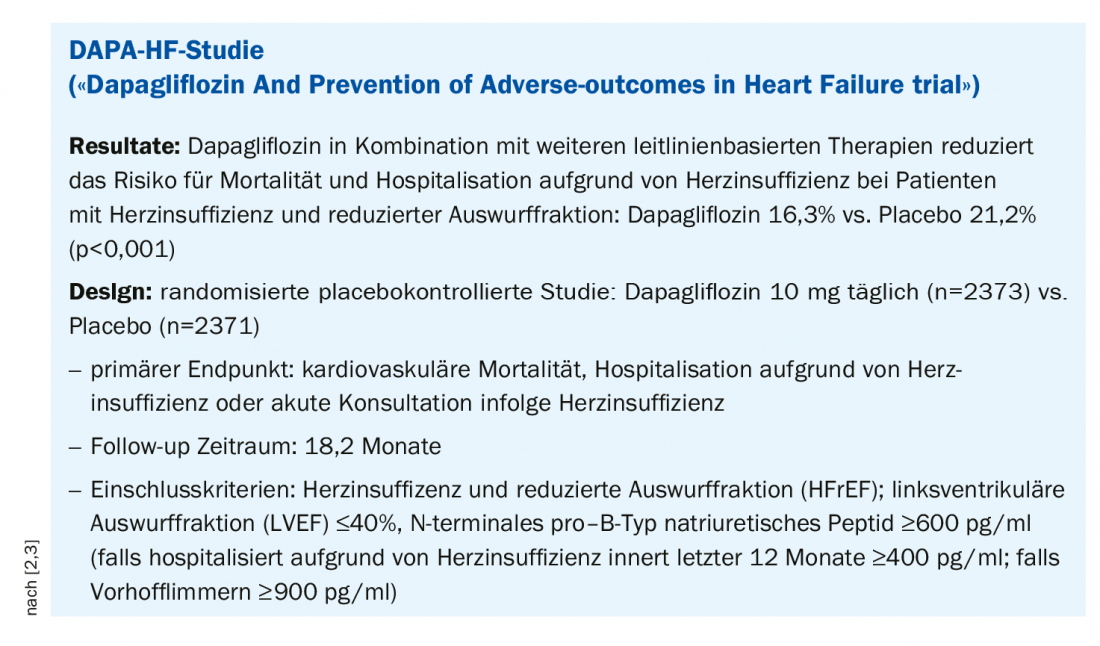
In this context, the prospective randomized, placebo-controlled Dapagliflozin And Prevention of Adverse-outcomes in Heart Failure trial (DAPA-HF) was designed to evaluate the effects of dapagliflozin on morbidity and mortality in patients with heart failure with reduced ejection fraction (HFrEF) (Box). The primary end point was defined as cardiovascular mortality, hospitalization for heart failure, or consultation for acute heart failure. The patient population included individuals with heart failure and reduced ejection fraction (HFrEF). A total of 4744 subjects were included with a left ventricular ejection fraction (LVEF) ≤40%; 42% were diabetic. Study participants were randomly assigned to dapagliflozin 10 mg daily (n=2373) or placebo (n=2371) conditions regardless of diabetes status [2,3]. The differences in the primary endpoint after a period of 18.2 months were significant (p<0.001): Dapagliflozin 16.3% vs. Placebo 21.2%. No serious adverse side effects occurred. Tolerability did not differ significantly as a function of subject age (mean age: 66 years) [11].
Source: FOMF Zurich
Literature:
- Lehmann R: Endocrinology, slide presentation, Prof. Roger Lehmann, MD, University Hospital Zurich, FOMF Internal Medicine, Update Refresher, Zurich, Dec 04, 2019.
- McMurray JJV: A trial to evaluate the effect of the sodium-glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF). European Journal of Heart Failure 2019; 21(5): 665-675.
- McMurray J: DAPA HF – The Dapagliflozin And Prevention Of Adverse-outcomes In Heart Failure Trial. Late-Breaking Science, ESC Congress 2019
- McMurray JJ, Gerstein HC, Holman RR, Pfeffer MA: Lancet Diabetes Endocrinol 2014; 2: 843-851.
- Seferović PM, et al: Eur J Heart Fail 2018; 20: 853-872.
- Fitchett D, et al: EMPA-REG OUTCOME® Trial Investigators. Eur Heart J 2016; 37: 1526-1534.
- Mahaffey KW, et al: CANVAS Program Collaborative Group. Circulation 2018; 137: 323-334.
- Wiviott SD, et al: N Engl J Med 2019; 380: 347-357.
- Kristensen SL, et al: CHARM Investigators and Committees. Cardiovasc Drugs Ther 2017; 31: 545-549.
- Kristensen SL, et al: PARADIGM-HF Investigators and Committees. Circ Heart Fail 2016; 9:e002560.
- Martinez FA, et al: Insights From DAPA-HF Circulation 2019; 140: 00-00. DOI: 10.1161/CIRCULATIONAHA.119.044133.
HAUSARZT PRAXIS 2020; 15(2): 38 (published 8.2.20, ahead of print).











