Cutaneous symptoms are of particular importance because they can be detected before systemic manifestations occur. Based on this, therapeutic measures relevant to the course of the disease can be initiated at an early stage.
Systemic sclerosis is a rare autoimmune disease that belongs to the group of collagenoses. The immune system attacks the body’s own connective tissue, which leads to an inflammatory reaction resulting in hardening of the skin, blood vessels as well as internal organs. Major symptoms appearing early in the course of the disease include Raynaud’s syndrome, digital ulcers, cutaneous sclerosis, calcinosis cutis, telangiectases, pruritus, and dyspigmentation. To date, disease management in this multisystem disease has been a major challenge.
Heterogeneous course and prognosis
Depending on the type of skin involvement, a distinction is made between limited systemic sclerosis (lSSc) and diffuse systemic sclerosis (dSSc) [1]. Patients with cutaneous fibrosis in the acral parts of the body (face and extremities distal to knees and elbows) are classified as lSSc (box: limited systemic sclerosis); presence of fibrosis in the trunk and proximal areas of the extremities is considered a criterion for dSSc(box: diffuse systemic sclerosis) [2]. Systemic sclerosis continues to be characterized by early mortality, with course and prognosis varying and depending on organ involvement. In lSSc, slow and late organ involvement is associated with a 10-year survival of more than 90% [3]. In dSSc, the prognosis is worse, due to rapid progression of skin and organ involvement including the cardiovascular system, lungs, kidneys, gastrointestinal tract, and central and peripheral nervous systems. The time lag between the onset of Raynaud’s syndrome and skin symptoms tends to be shorter in dSSc. The overall 10-year survival rate for dSSc ranges from 65% to 82% and is influenced by complications of various organ systems [3]. Another subtype is called systemic sclerosis without scleroderma (ssSSc) and affects approximately 5% of patients with SSc, it is a disease form with typical findings (positive autoantibodies, Raynaud’s syndrome, pulmonary involvement but without skin fibrosis [2].

Symptom-targeted therapy options
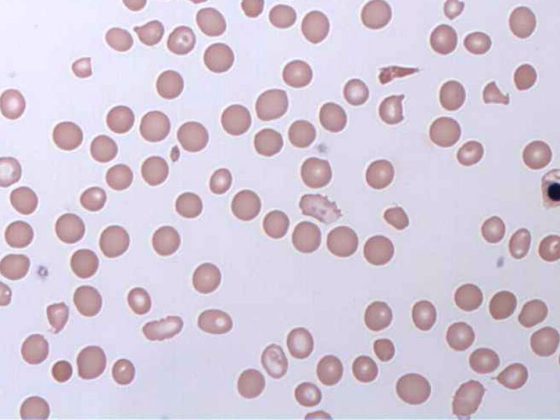
Systemic scleroderma is classified as a rheumatologic disease, but there is overlap with dermatology, as with certain other diseases (e.g., lupus erythematosus, dermatomyositis, Sjögren’s syndrome). Interdisciplinary treatment planning and implementation is recommended. Early diagnosis and interventions based on it can have a positive impact on disease progression [4]. If Raynaud’s syndrome is present, further investigations should be initiated. If no scleroderma-typical skin symptoms are present, laboratory examination and capillary microscopy (vessels of the nail bed) can provide diagnosis-relevant indications. Histopathological examination of biopsied skin reveals atrophic changes and increased collagen deposition.
Table 1 provides an overview of current treatment measures for some of the most common symptoms of SSc [2]. The therapy of this systemic disease is complicated and ranges from inhibition of autoimmunological processes to anti-inflammatory and organ-specific measures. Because the pathogenesis of SSc remains incompletely understood, treatment options are based on disease-modifying methods and organ-specific drugs. Treatment decisions should be based on a careful assessment of symptoms, course, and disease activity [2].

Glucocorticoids are advised in the presence of an inflammatory form of SSc-associated myopathy [2]. Arthritis in SSc usually requires disease-modifying antirheumatic drugs (DMARDs) or glucocorticoids. If peripheral vasculopathy and digital ulcers are noted, calcium channel blockers (nifedipine, amlodipine) are indicated. If response is poor, treatment with phosphodiesterase-5 (PDE-5) inhibitors may be considered. Intravenously administered prostanoids lead to a significant improvement in the healing process of digital ulcers and have a positive effect on the microcirculation. Immunosuppressants (e.g., MTX), cyclophosphamide, and mycophenolate mofetil have proven effective in treating skin fibrosis. In case of contraindications or lack of efficacy, low-dose glucocorticoids or the monoclonal antibody rituximab can be used [2].
Literature:
- Sticherling M: JDDG 2019; 17(7): 716-729.
- Sobolewski P, et al: Rheumatol 2019; 57(4): 221-233.
- Al-Dhaher FF, Pope JE, Ouimet JM: Semin Arthritis Reum 2010; 39: 269-277.
- Pearson DR, et al: Clinics in Dermatology 2018; 36(4): 459-474.

DERMATOLOGY PRACTICE 2020; 30(1): 22-23