Diabetic ketoacidosis (DKA) is an acutely life-threatening complication of diabetes mellitus that occurs predominantly in type 1 diabetes, but is also increasingly occurring in people with type 2 diabetes. A special form is euglycemic DKA, which mainly occurs during therapy with SGLT2 inhibitors. Even though it has become rare and the mortality rate is now only just over 1%, these deaths are usually preventable. Timely diagnosis, standardized treatment protocols and, above all, prophylaxis are crucial for the prognosis.
You can take the CME test on our learning platform after you have reviewed the recommended materials. Please click on the following button:
Diabetic ketoacidosis (DKA) is an acute, life-threatening complication of diabetes mellitus that mainly occurs in type 1 diabetes, but is also increasingly occurring in people with type 2 diabetes. A special form is euglycemic DKA, which mainly occurs during therapy with SGLT2 inhibitors.
Even though it has become rare and the mortality rate today is just over 1%, these deaths are usually preventable. Timely diagnosis, standardized treatment protocols and, above all, prophylaxis – not least through the appropriate training of patients and doctors – are crucial for the prognosis.
Case study
23-year-old Beat R. has had type 1 diabetes since the age of 14. The student has been fitted with an insulin pump for 6 years and has been using an AID system for a good year, i.e. the insulin pump adjusts the insulin delivery to the blood glucose values. Mr. R. finds this very convenient and no longer worries so much about his diabetes, especially as he has exams coming up. After dinner, Mr. R. feels slightly nauseous and vomits several times during the night. He interprets this as an infection and doesn’t give it a second thought. The next morning he feels faint, the nausea has increased and the blood glucose concentration is 23.5 mmol/l. He calls for an insulin bolus. He calls for an insulin bolus of 8 units and decides not to go to work because of the infection, goes to bed and falls asleep. Around midday he wakes up with abdominal pain, his blood sugar is no longer measurable (with his CGM system this corresponds to >30 mmol/l). Beat R. now calls his family doctor. He urgently suspects ketoacidosis and therefore admits the patient to the nearest acute hospital via the ambulance service.
On arrival at the clinic, Mr. R. is somnolent but can be woken up. Blood sugar is 36.7 mmol/l, β-Hxdroxybutyrate is 6.3 mmol/l, bicarbonate is 6 mmol/l and pH is 7.1. Blood pressure is 100/60 mmHg.
Beat R. is admitted to the hospital’s intensive care unit due to severe ketoacidosis, after 3 days of standardized therapy he has fully recovered. Incidentally, the cause of the ketoacidosis was not an infection, but a pump malfunction to which the patient did not respond.
In the subsequent conversations, it turns out that Mr. R. was tired of the pump’s frequent alarms and mostly ignored them.
Epidemiology and clinic of hyperglycemic emergencies
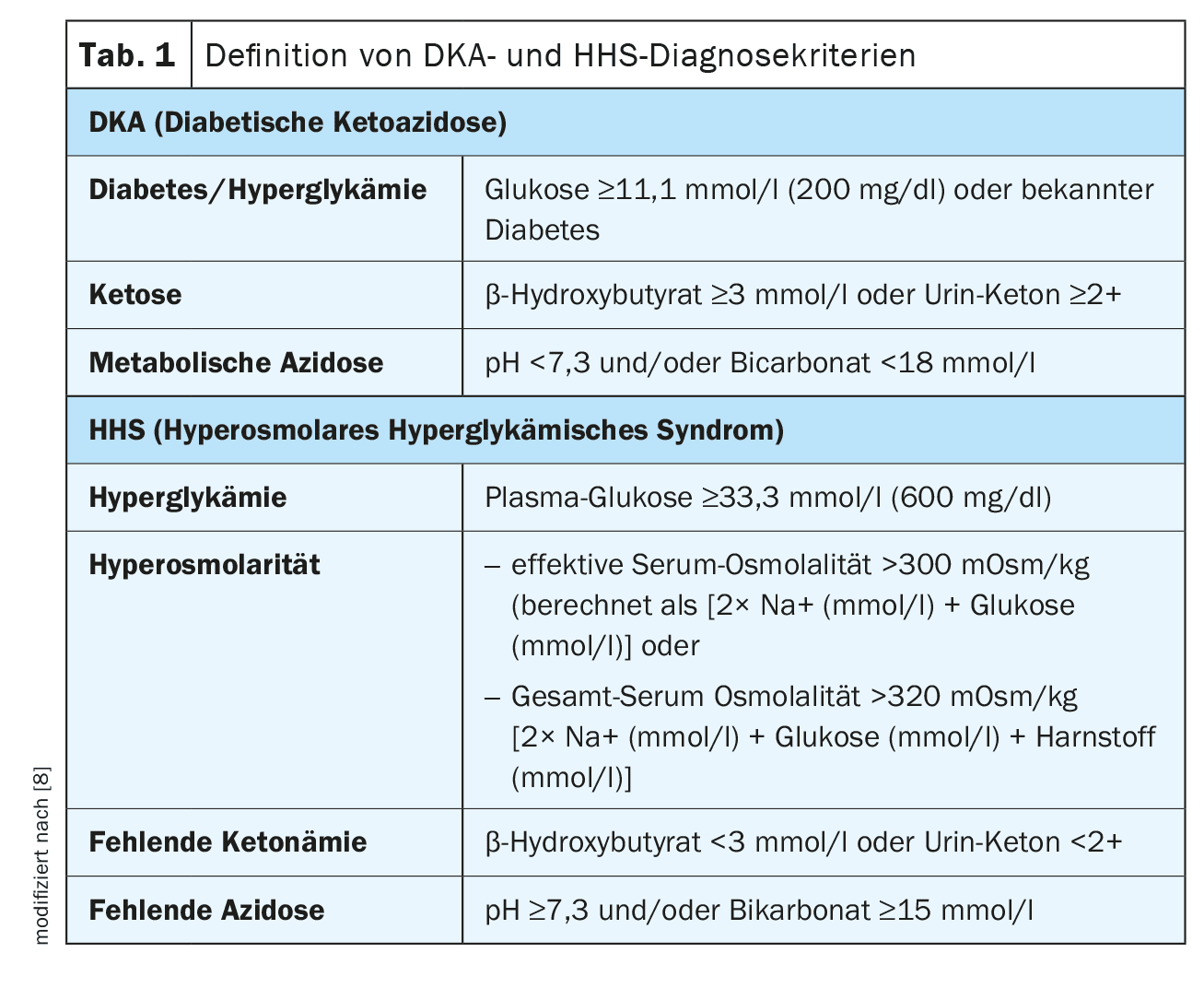
There are two forms of life-threatening hyperglycemic states. Diabetic ketoacidosis (DKA) occurs predominantly in people with type 1 diabetes and has a low mortality rate. Hyperglycaemic-hyperosmolar syndrome (HHS), on the other hand, usually occurs in people with type 2 diabetes and is still characterized by a high mortality rate. Mixed forms are very often found, especially in the presence of acute illnesses. These can often mask the clinical appearance of DKA, for example in the case of acute infections (gastroenteritis, pneumonia, urinary tract infection), other acute illnesses (e.g. myocardial infarction) or (planned) operations. It is therefore important to be aware of the possibility and to initiate diagnostic clarification in good time (Table 1).
Worldwide, hospital admissions for hyperglycemic derailments have increased significantly, with a particularly striking increase of >55% in the last ten years in the over 45s. In children and adolescents, DKA is the most common complication of diabetes. About every third manifestation occurs in the context of DKA.
Clinic
The symptoms are typically very variable, and the full clinical picture with dehydration, ketone odor, Kussmaul breathing and coma is rarely seen. Much more common are symptoms that can easily be mistaken for harmless illnesses – especially in children: Nausea, abdominal pain, vomiting are, well, common occurrences. This makes it all the more important to look out for accompanying abnormalities: Fatigue, drowsiness, but also states of confusion, weight loss, polyuria and polydipsia are also typical in the presence of DKA, but rarely occur in banal gastrointestinal diseases (Fig. 1).
In the case of a relative insulin deficiency, the triggering disease is usually in the foreground and the developing DKA may be masked. The differential diagnosis can be particularly difficult in critically ill patients or postoperatively – it is therefore all the more important to consider the possibility of ketoacidosis and to initiate the appropriate diagnostics. It must also be borne in mind that standard bedside glucose determinations do not always provide reliable results under intensive care conditions. If a diabetic metabolic derailment is suspected, a venous blood sample should always be taken to determine the glucose level.
Diagnostics
DKA is defined as a condition with hyperglycemia, ketonemia and metabolic acidosis. Depending on the degree of ketonemia and acidosis, 3 stages are distinguished (Table 2).
Unfortunately, a qualified diagnosis of diabetic ketoacidosis is hardly possible in outpatient practice, as there is usually no possibility for blood gas and acid/base analysis. This leaves only β-Hxdroxybutyrate in capillary blood as a reliable and immediately determinable parameter. However, this also means that only a suspected diagnosis can be made under outpatient conditions. If there is a well-founded suspicion of DKA, hospitalization is usually unavoidable.
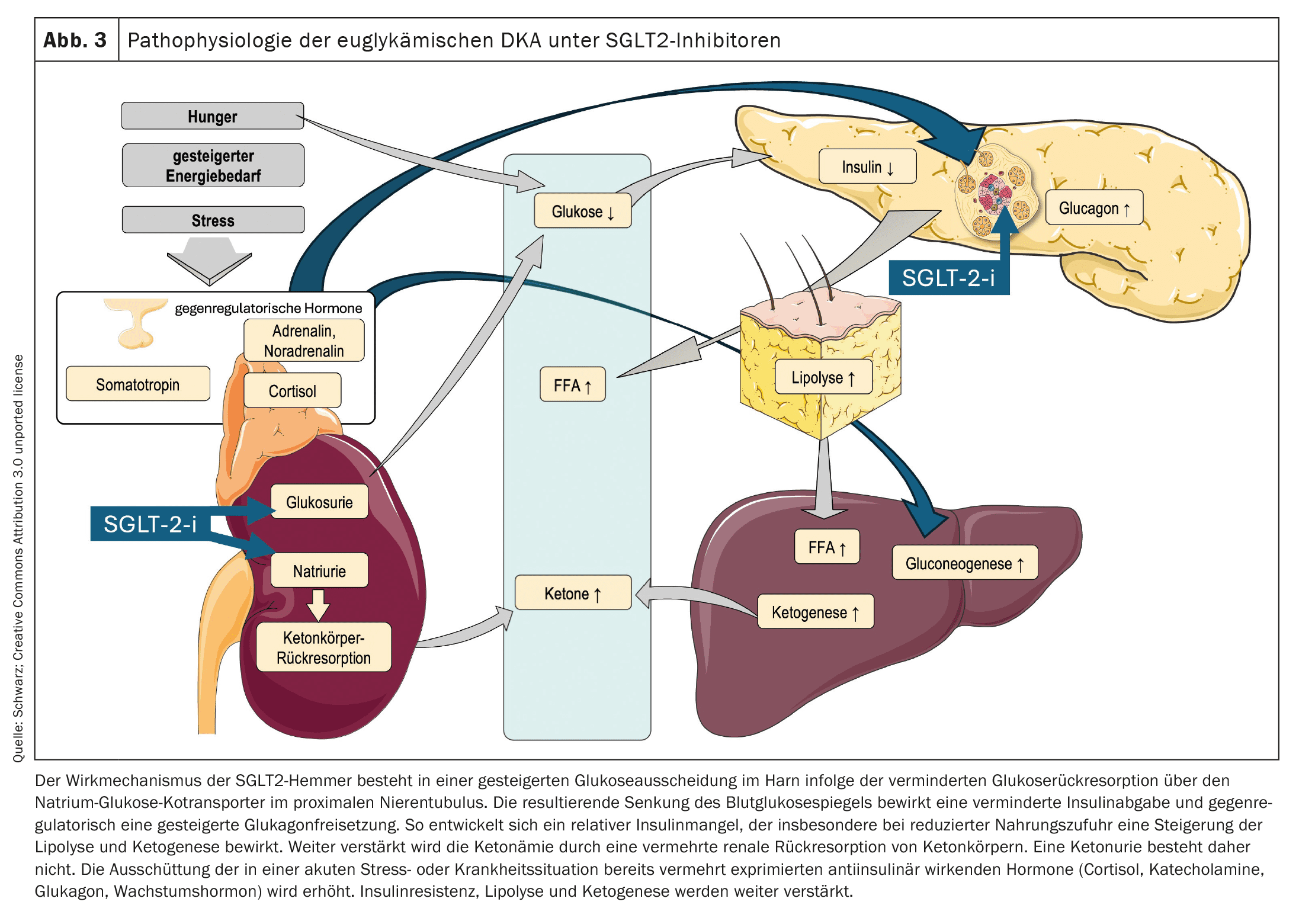
A special form is euglycemic diabetic ketoacidosis (EDKA). This is often recognized late (due to the unremarkable blood sugar) and is therefore often severe. Particularly under therapy with SGLT2 inhibitors, in pregnant women with gestational diabetes or pre-existing diabetes mellitus, in people with diabetes and additional liver disease and also in younger patients with type 1 diabetes, metabolic acidosis occurs with a serum bicarbonate level <10 mM without the blood glucose levels being significantly elevated. This is also the reason why the BG value was lowered from 14 to 11 mmol in the latest recommendations.
To avoid this complication, patients must be informed to pause the medication in question, e.g. during acute infections, before surgery under general anesthesia, but also during periods of fasting. As a supporting tool, the SGSE has created a “Sick Day Rules” card that can be given to patients as part of such instructions.
Hyperglycemia and its pathophysiology: an overview
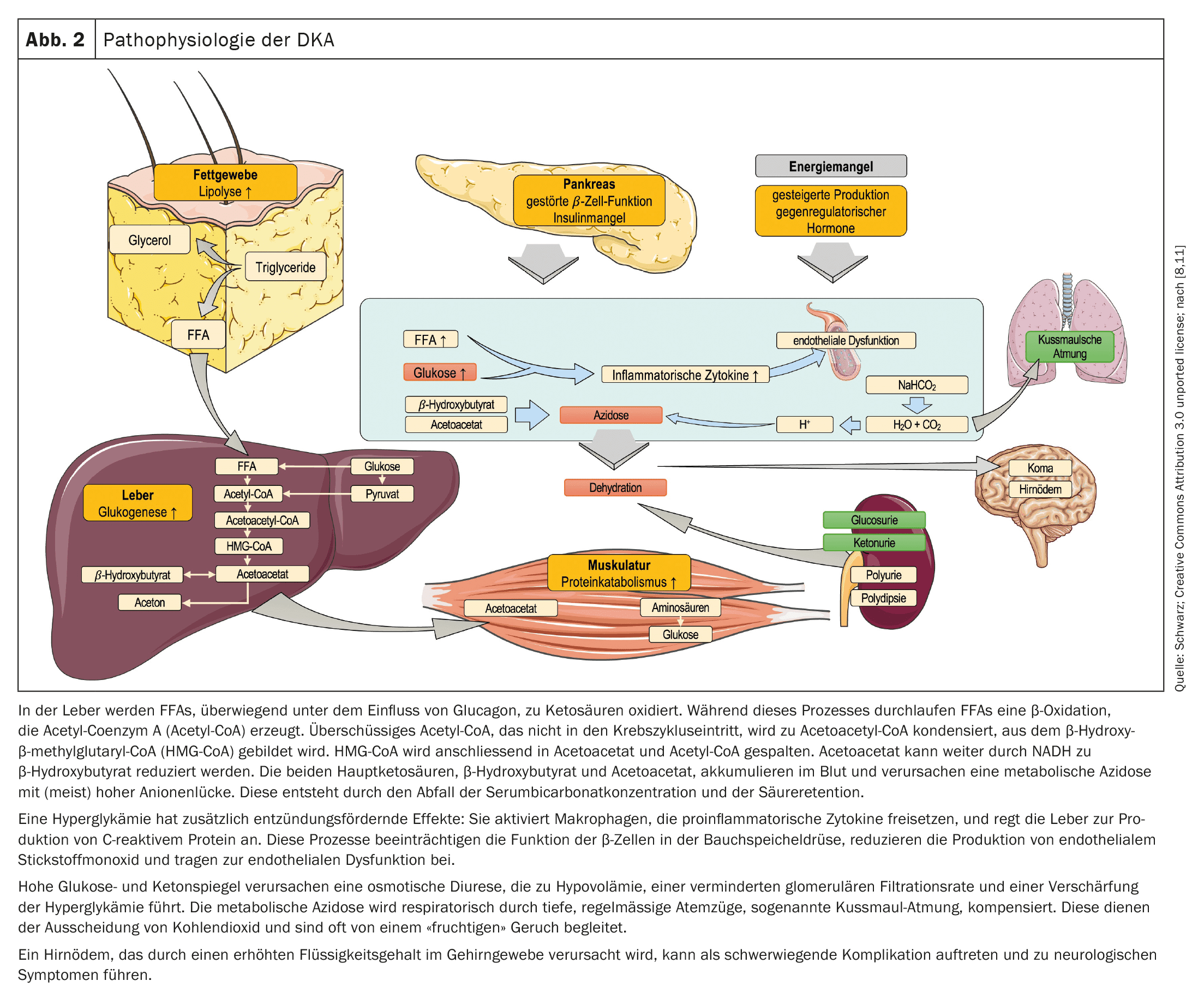
Hyperglycaemia occurs in the case of insulin deficiency due to three main processes: increased gluconeogenesis, accelerated glycogenolysis and impaired glucose utilization in peripheral tissues. The drop in insulin concentration in combination with an increase in counter-regulatory hormones (glucagon, adrenaline, noradrenaline, cortisol and growth hormone) activates the hormone-sensitive lipase in adipose tissue. This leads to the breakdown of triglycerides into glycerol and free fatty acids (FFAs) (Fig. 2).
The pathophysiology of euglycemic ketoacidosis with SGLT2 inhibitors is not yet fully understood. It is still unclear whether SGLT2 inhibitors can be the cause of the development of DKA or whether they merely mask hyperglycemia by increasing glucose excretion. Possible mechanisms are shown in Figure 3.
Note: A lack of insulin leads to hyperglycaemia and, as glucose is not absorbed into muscle and fat cells, to an intracellular glucose deficiency. This increases the concentration of counter-regulatory hormones. Energy is now mainly produced through ketogenesis, triggered by lipolysis, in which triglycerides are broken down into free fatty acids and glycerol. The resulting ketone bodies lead to metabolic acidosis and can be detected in the blood and urine. Hyperglycemia causes osmotic diuresis, fluid and electrolyte losses and the risk of dehydration.
Causes
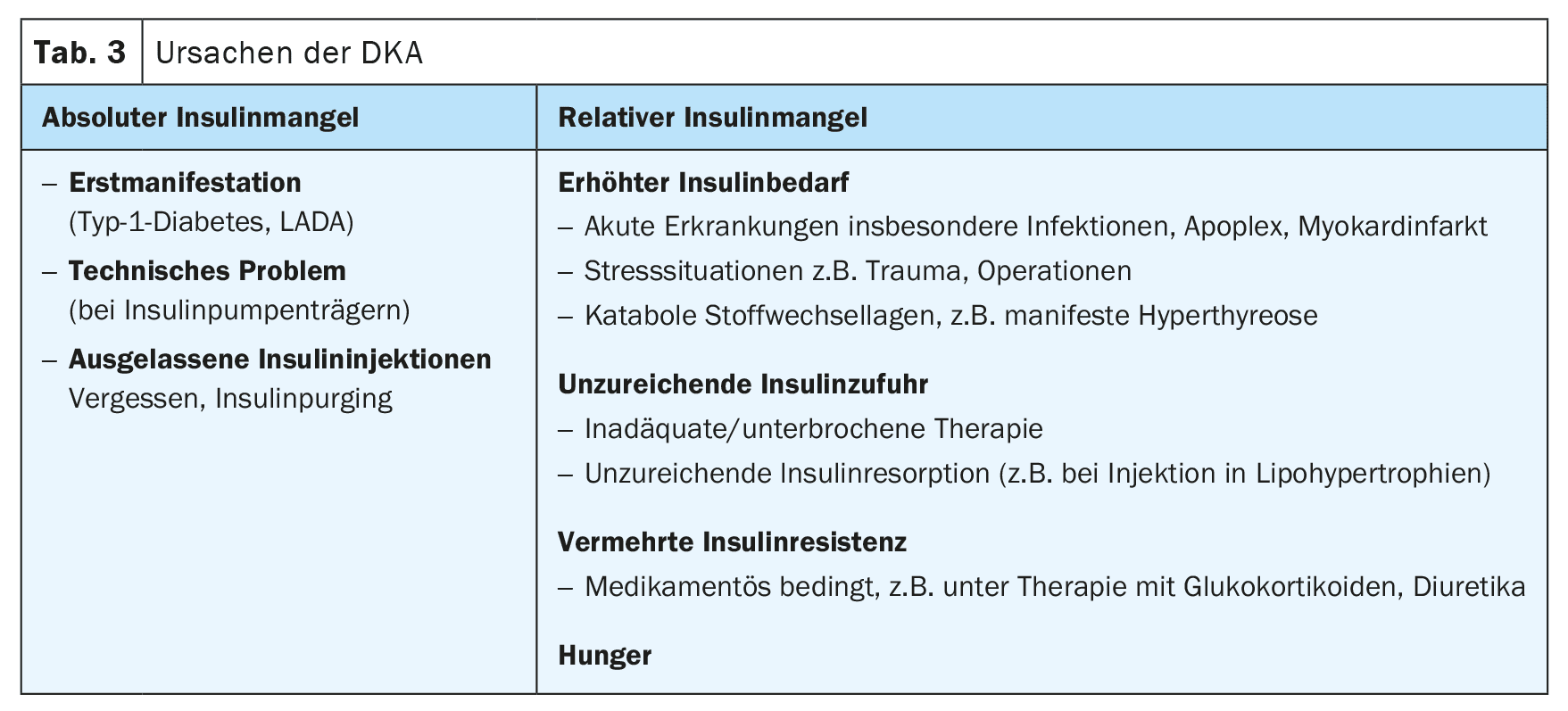
The prerequisite for the development of DKA is an insulin deficiency. As with the initial manifestation of type 1 diabetes, this can be caused by a lack of or insufficient insulin intake or by an increased requirement, e.g. in acute illnesses or operations (Table 3).
Therapy
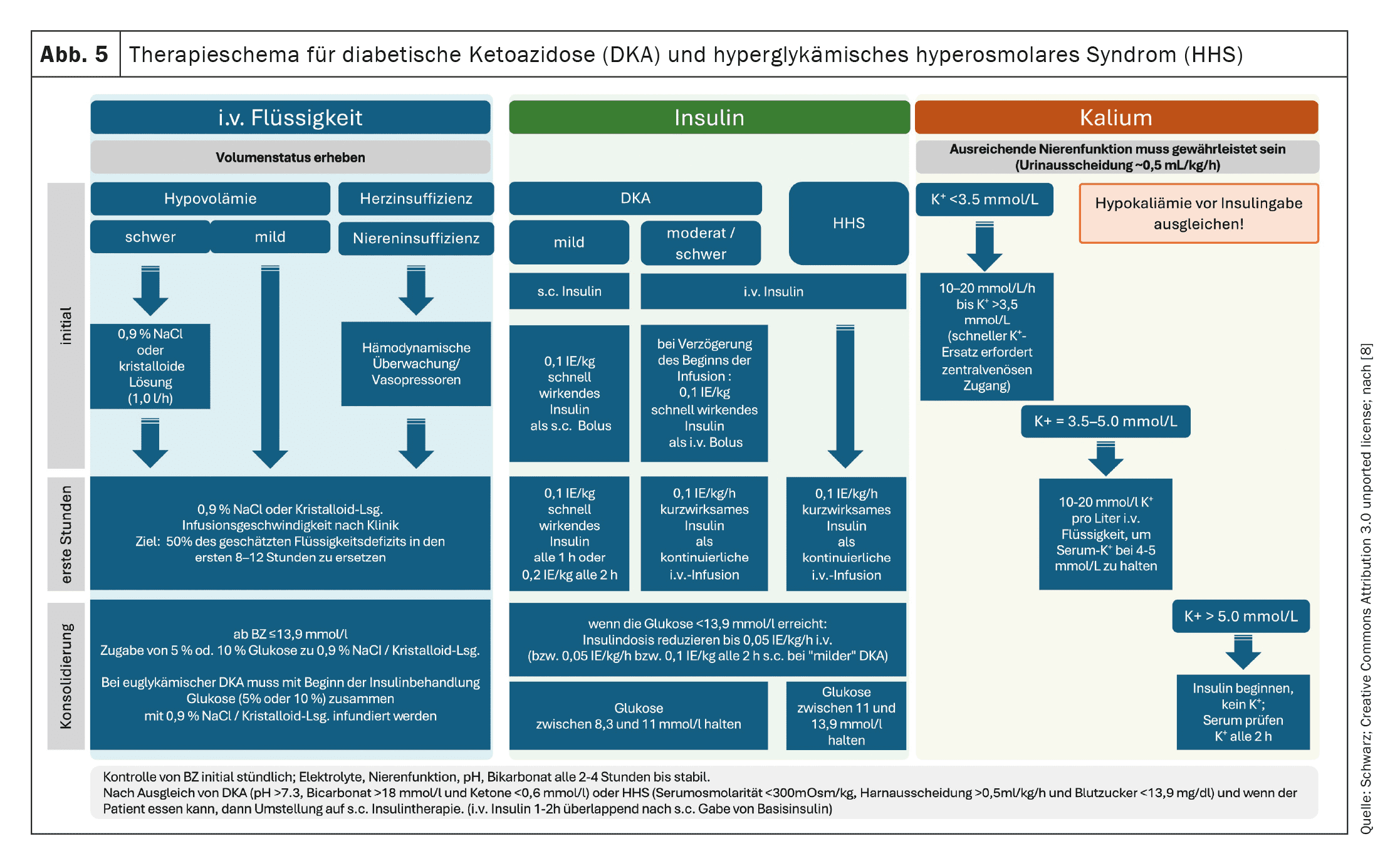
In all cases, therapy is based on compensating for the fluid and electrolyte deficit and the insulin deficiency. Thrombosis prophylaxis should also be considered, particularly in cases of exsiccosis.
If a patient presents to the practice with suspected DKA, the first thing to be done (in addition to measuring vital parameters and an indicative clinical examination) is to determine glucose (from venous plasma) and β-hydroxybutyrate (practice laboratory, the results must be available after 15 minutes at the latest). The inability to diagnose acidosis on an outpatient basis usually leaves little room for maneuver. If there is no ketoacidosis but only ketonemia (β-HB <3 mmol/l), outpatient treatment can be given (Fig. 4, 5). Patients with elevated ketone levels should also be treated according to this scheme if a medical consultation is not or not immediately possible. This requires the patient to be informed and instructed accordingly (see Prophylaxis).
If the level is >3 mmol/l, DKA is likely and therefore hospital treatment is usually mandatory. Until transportation (by ambulance), oral fluid intake is stopped, a large-volume venous access is established and the infusion of isotonic, balanced crystalloid solution (0.9% NaCl only if not available) is started. The infusion rate should be 1 l/h. The use of “physiological” saline solution not only has the disadvantage over balanced solutions that there is a risk of hyperchloremic metabolic acidosis with large volumes, it also contains no potassium, although this is needed. However, targeted compensation of the potassium loss caused by the insulin deficiency can only take place under inpatient conditions.
Patients with mild DKA can be treated on a normal ward or, if necessary, in the emergency outpatient department, provided that it is possible to stay there for several hours. For moderate and severe cases, care in an intermediate care or intensive care unit is recommended.
Monitoring is carried out continuously on the monitor according to a standardized protocol, with heart rate, respiratory rate and blood pressure being checked every 30 minutes and GCS being determined every hour. Laboratory checks should be carried out every hour (glucose) and every 2-4 hours (electrolytes, renal function, venous pH, osmolality).
The fluid deficit should be corrected within the first 24 to 48 hours. An initial rate of 500-1000 ml/h during the first 2-4 hours is recommended. However, caution should be exercised with rapid fluid administration in people with heart or kidney disease, pregnant women, the elderly or people with serious co-morbidities. Heart failure and/or end-stage renal disease should be treated carefully with smaller boluses of isotonic or crystalloid solutions (e.g. 250 ml each). It has long been assumed that cerebral edema can be caused by too rapid rehydration. The pathophysiological mechanism underlying diabetic ketoacidosis-induced cerebral edema is controversial. The risk of brain damage is neither influenced by the infusion rate nor by the sodium chloride concentration.
Typically, the plasma glucose concentration drops to <11 mmol/l or <200 mg/dl before the ketonemia subsides. It is therefore necessary to give additional glucose from this level to prevent hypoglycemia and allow insulin administration to continue.
Most patients with DKA initially have normal to elevated potassium levels. As a result of acidosis and insulin deficiency, there is a shift of potassium ions from the intracellular to the extracellular space. Osmotic diuresis and increased potassium excretion in the urine contribute to further depletion of potassium stores. Therefore, potassium supplementation should be started together with insulin administration, even if serum potassium levels are normal, to prevent hypokalemia. If serum hypokalemia is present at the time of DKA diagnosis, potassium supplementation should be initiated along with fluid administration and the initial insulin infusion should be delayed. Potassium administration should be maintained until potassium levels normalize, renal function is normal and urination is intact.
Hyponatremia is also common in DKA. It is caused by the redistribution of water from the intracellular to the extracellular space. Due to the osmotically active glucose, there is no hypoosmolality. The resulting isotonic/hypertonic hyponatremia does not require therapy. It is therefore necessary to calculate the corrected serum sodium concentration. Correction is only necessary if this results in a sodium deficiency. Bicarbonate administration for the treatment of metabolic acidosis is generally not advisable, with the exception of life-threatening hyperkalemia and severe acidosis (pH <6.9).
Insulin should be administered at least 1 hour after the start of fluid resuscitation. After an initial bolus (not recommended for pediatric patients), normal insulin or a short-acting analog insulin should be administered via perfusor. In mild DKA, insulin can also be administered subcutaneously. The insulin infusion rate should not be reduced until the ketoacidosis is corrected or nearly corrected.
DKA is treated if the following criteria are met:
- No gastrointestinal symptoms, oral administration of food and medication is possible
- the blood glucose concentrations are less than 11 mmol/l or 200 mg/dl
- β-hydroxybutyrate <0.6 mmol/l
- venous pH ≥7.3 or bicarbonate ≥18 mmol/l.
When switching from intravenous insulin to subcutaneous injections, one should not proceed too hastily; an overlapping changeover is necessary. A long-acting analog insulin (Glargine U100 or U300 or Degludec, but not Icodec) should be given 1 to 2 hours before the end of the insulin infusion. The optimum time for ending the i.v. insulin administration is before a meal, at which time s.c. insulin is administered for the first time. insulin is then administered for the first time.
Prophylaxis
Diabetic ketoacidosis is a rare event and fortunately most people with diabetes never experience it. However, those who are admitted to hospital with DKA have a very high risk of recurrence. As every DKA is a serious and, even today, potentially fatal complication, prevention is particularly important. Support and education are the cornerstones of management rather than the need for a different insulin regime.
People with psychosocial problems, mentally ill people and socially disadvantaged groups are particularly at risk. The use of alcohol and cannabis also increases the risk of ketoacidosis. These patients in particular are more difficult to reach with our usual care scenarios and training measures. Psychological support is indicated, but is generally impossible for capacity reasons.
The topic of “dealing with emergency situations” must be an integral part of regular diabetic training. Each patient should also receive an individualized emergency plan. The average daily insulin dose is also noted there. Users of an insulin pump (of any type, including AID) must know that they must never make the necessary corrections via the pump.
Conclusion
Diabetic ketoacidosis (DKA) is a potentially life-threatening emergency in people with diabetes mellitus. In 1/3 of cases, patients with type 2 diabetes are affected. It is usually triggered by infections and/or errors in insulin therapy. An absolute or relative insulin deficiency leads to uninhibited lipolysis and ketogenesis. The result is hyperglycemia, ketonemia and metabolic acidosis. Especially under therapy with SGLT2 inhibitors, hyperglycemia may be absent (euglycemic DKA).
The basis of therapy is volume substitution, insulin administration and potassium substitution, accompanied by close monitoring. Once the DKA has been corrected, the cause must be clarified. Good and repeated training is crucial for the patient’s prognosis. Information and knowledge of the disease are essential for the practitioner to make quick and correct decisions.
Take-Home-Messages
- Diabetic ketoacidosis (DKA) is a potentially life-threatening emergency in people with diabetes mellitus. Type 2 diabetics are affected in 1/3 of cases. It is usually triggered by infections and/or errors in insulin therapy.
- An absolute or relative insulin deficiency leads to uninhibited lipolysis and ketogenesis. This results in hyperglycemia, ketonemia and metabolic acidosis. Hyperglycemia can be absent, especially under therapy with SGLT2 inhibitors (euglycemic DKA).
- The basis of therapy is volume substitution, insulin administration and potassium substitution, accompanied by close monitoring. Once the DKA has been compensated, the cause must be clarified.
- Good and repeated training is crucial for the patient’s prognosis. On the part of the practitioner, information and knowledge of the disease are essential for quick and correct decisions.
| Images created using Servier Medical Art, licensed under Creative Commons Attribution 3.0 unported license. |
Literature:
- American Diabetes Association Professional Practice C. 16. Diabetes Care in the Hospital: Standards of Care in Diabetes-2025. Diabetes Care 2025; 48: S321-S334; doi: 10.2337/dc25-S016.
- Perschinka F, Koglberger P, Klein SJ, et al: Hyponatremia: Etiology, diagnosis and acute therapy. Med Klin Intensivmed Notfmed 2023; 118: 505-517; doi: 10.1007/s00063-023-01049-0.
- Stewart PA, Nestor CC, Clancy C, et al: The peri-operative implications of sodium-glucose co-transporter 2 inhibitors: a narrative review. Anaesthesia 2025; 80: 85-94; doi: 10.1111/anae.16461.
- Yan JW, Slim A, Van Aarsen K, et al: Balanced crystalloids (Ringer’s lactate) versus normal saline in adults with diabetic ketoacidosis in the Emergency Department (BRISK-ED): a pilot randomized controlled trial. Emerg Med J 2024; 41: 103-111; doi: 10.1136/emermed-2023-213290.
- Dhatariya K, James J, Kong MF, et al: Diabetes at the front door. A guideline for dealing with glucose related emergencies at the time of acute hospital admission from the Joint British Diabetes Society (JBDS) for Inpatient Care Group. Diabet Med 2020; 37: 1578-1589; doi: 10.1111/dme.14304.
- Tamsett Z, James S, Brown F, et al: Modifiable factors to prevent severe hypoglycaemic and diabetic ketoacidosis presentations in people with type 1 diabetes. Diabet Med 2024; 41: e15384;
doi: 10.1111/dme.15384. - Gupta A, Brazier B, Rengarajan L, et al: Determining factors influencing hospital stay for individuals admitted with diabetes-related ketoacidosis – findings from DEKODE length of stay quality improvement project. Clin Med (Lond) 2024; 24: 100255; doi: 10.1016/j.clinme.2024.100255.
- Umpierrez GE, Davis GM, El Sayed NA, et al: Hyperglycaemic crises in adults with diabetes: a consensus report. Diabetologia 2024; 67: 1455-1479; doi: 10.1007/s00125-024-06183-8.
- Sacks DB, Arnold M, Bakris GL, et al: Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Diabetes Care 2023; 46: e151-e199; doi: 10.2337/dci23-0036.
- Holt RIG, De Vries JH, Hess-Fischl A, et al: The Management of Type 1 Diabetes in Adults. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2021; 44: 2589-2625; doi: 10.2337/dci21-0043.
- Dhatariya KK, Glaser NS, Codner E, et al: Diabetic ketoacidosis. Nat Rev Dis Primers 2020; 6: 40; doi: 10.1038/s41572-020-0165-1.
InFo DIABETOLOGY & ENDOCRINOLOGY 2025; 2(1): 6-12