In gastrointestinal functional diagnostics, such as high-resolution manometry, great progress has been made in recent years. The new technologies provide an objective description of gastrointestinal function and often an explanation for the patient’s symptoms. The results of the tests often have a direct influence on the choice of specific therapeutic measures. The tests help to establish a diagnosis. This can be therapeutic, even if no specific treatment is available (yet). Patients who know the cause of their symptoms can usually cope better with their situation.
In the first part of this review, a structured approach to the examination of patients with gastrointestinal symptoms was outlined. In the second part, the possibilities of a specialized clarification of patients are presented, in whom no cause of the symptoms could be found with routine clarifications.
Pharyngeal and esophageal dysfunction
In pharyngeal dysphagia, videofluoroscopy is the primary investigation. It allows visualization of the structure and function of the oropharynx and identifies any aspiration. If this examination is not diagnostic, high-resolution manometry with impedance may help to further clarify the dysfunction [26]. For esophageal swallowing problems, new catheter and manometry systems with up to 36 sensors allow seamless imaging of pressure conditions throughout the esophagus. Certain catheters can measure impedance so that, in addition to pressure, bolus passage can be documented [6,27]. An important finding of these combined studies is that dysphagia and other esophageal symptoms are rarely caused by abnormal motility alone. Most often, symptoms do not occur until a motility disorder is accompanied by bolus retention or reflux [27].
The new technique results in a new definition of motility disorders, which is defined in the “Chicago Classification” [28]. For this purpose, examination and evaluation must be carried out according to standardized algorithms. A new feature compared with conventional manometry is the definition of certain motility disorders by objective numerical values, which have been shown in studies to have high interobserver agreement and diagnostic accuracy [29,30]. The new classification makes a clear distinction between severe motility disorders of undisputed clinical significance and abnormalities occasionally seen in healthy individuals.
In the first case (e.g., achalasia, spasms), targeted treatment is indicated. Based on high-resolution manometry (HRM), three subtypes of achalasia can be distinguished [31]. These differ significantly with respect to the therapeutic success of Heller myotomy or pneumatic balloon dilatation [31,32]. Type 2 achalasia responds well to both therapeutic modalities; therapeutic success is less consistent in type 1 achalasia (often with dilatation of the esophagus). In this case, surgical myotomy of the esophagus is the most likely option. In type 3 achalasia (spastic achalasia), this may be combined with dilatation of the esophago-gastric junction (EGJ dilatation) with botulinum toxin injections of the tubular esophagus as an alternative at best. The long-term results of the still experimental peroral esophageal myotomy (POEM) are still unclear.
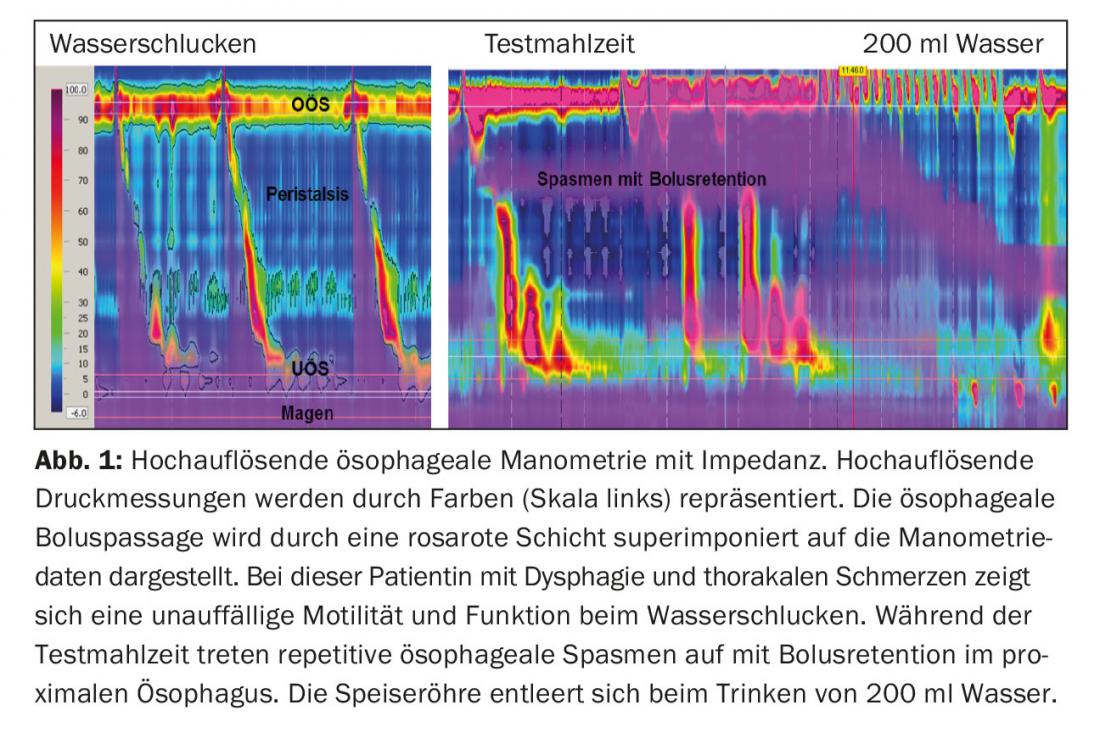
A weakness of the current HRM protocol is that in the absence of severe dysmotility, the cause of symptoms cannot be explained. The reason for this is that few patients have dysphagia when swallowing water. Recent studies have used HRM (often together with impedance) to investigate complex esophageal function during eating [33,34]. If esophageal function is examined during eating, most symptomatic motility disorders can be visualized (Fig. 1) . In one study, it was shown that clinically relevant EGJ outflow obstruction could often be detected in patients with dysphagia after fundoplicatio with a test meal. The majority of these patients were successfully treated with balloon dilatation of the fundoplicatio cuff [34]. A prolonged post-meal HRM examination may reveal the cause of refractory reflux symptoms and other postprandial symptoms. This examination is particularly important when distinguishing between typical reflux events and behavioral disorders, e.g., rumination syndrome or supragastric belching [24].
Gastroesophageal reflux disease
In European countries, 5-15% of the population report suffering from heartburn or other stomach complaints at least two to three times a week [1]. Gastroesophageal reflux disease (GERD) is diagnosed based on symptoms and endoscopy [35]. In cases of poor symptom response to high-dose proton pump inhibitors (PPI), modern functional diagnostics can provide a differentiated and clinically relevant differential diagnosis. A management algorithm for refractory patients, based on the guidelines of the German Society of Gastroenterology, is shown in Figure 2.

Endoscopically proven mucosal lesions in the esophagus allow the diagnosis of erosive reflux disease or, at best, Barrett’s esophagus. Non-erosive reflux disease (NERD) is defined as reflux disease without an endoscopically detectable lesion. Based on these criteria, NERD is the most common form of GERD, accounting for up to 70% of patients with typical reflux symptoms. The accuracy with which GERD can be diagnosed based on typical reflux symptoms or improvement of symptoms on PPI is limited. Typical symptoms – gastric burning and acid regurgitation – were present in only 49% of NERD patients in one study, in whom reflux disease was confirmed by 48-hour BRAVO pH metry. Conversely, up to 23% of patients with classic reflux symptoms do not have pH-metrically proven reflux disease [36]. This percentage is even higher (up to 75%) in patients with atypical reflux symptoms such as epigastric pain, chronic cough or other throat complaints [37]. These facts clearly show that only objective physiological measurements can distinguish GERD patients from those with functional GI disorders.
Formally, GERD should be diagnosed using pH-metry or combined intraluminal impedance analysis and pH-metry (MII-pH). To optimize the diagnostic sensitivity of the examinations, they should be performed without PPI medication [38]. The advantage of combined analysis with impedance allows detection not only of acid reflux but also of so-called non-acid reflux. In patients who have persistent symptoms on PPI, nonacid reflux causes up to 50% of typical reflux symptoms and 25% of atypical symptoms (cough) [37,39]. Impedance analysis also allows to detect the movement of air in the esophagus. This allows objective diagnosis of aerophagia or supra-gastric burping, even if pH-metry is negative [40].
In approximately 10% of patients, catheter-based esophageal examination cannot be performed because of intolerance. About the same number of patients are unable to eat, work, or sleep as usual during the examination because of local discomfort, so the examination often yields false negative results. In these situations, wireless pH metry (BRAVO) is a good alternative [41]. Another advantage of catheter-free systems is the ability to extend the examination for up to 96 hours. This increases the likelihood that any relationship between reflux events and symptoms can be demonstrated [42].
In patients with reflux symptoms and pathologic acid exposure in the esophagus, the diagnosis of NERD is clear. Positive association of symptoms and acid or nonacid reflux episodes (even in the absence of pathologic acid exposure) leads to a diagnosis of hypersensitive esophagus, another form of NERD. If both pathologic reflux and an association of reflux with symptoms can be ruled out, a diagnosis of “functional heartburn” is made. This distinction in classification is clinically relevant. If the diagnosis of GERD is supported by pathologic gastroesophageal reflux or positive symptom association on pH-metry, patients with NERD or hypersensitive esophagus respond equally well to medical or surgical therapy as patients with erosive reflux disease [43–46].
Disturbances of the intestinal transit time and digestion
Abnormal gastric and intestinal motility and function is present in gastroparesis, functional dyspepsia, and irritable bowel syndrome. Measurements of delayed or accelerated gastric emptying and small intestinal transit time by scintigraphy, C13 breath tests, or the new Smartpill may be diagnostically important (e.g., for the diagnosis of gastroparesis or “gastric dumping” syndrome) [47,48]. However, if it is not a distinct clinical picture, the association of symptoms with the result of transit determination is weak and the result has no influence on the clinical treatment concept [49,50]. Other sophisticated methods for assessing various motor and sensory GI functions (e.g., gastric barostat, MRI) provide more relevant information, but unfortunately are not available in clinical practice [51]. New scintigraphic methods are under development; they record gastric filling (accommodation) and measure gastric emptying with a simultaneous assessment of symptoms [52].
Hydrogen-based breath tests are commonly used to document lactose or fructose malabsorption. Bacterial fermentation of unabsorbed or insufficiently absorbed carbohydrates in the small intestine results in the formation of hydrogen in the colon. This diffuses very quickly into the blood and can be detected promptly in the breath. If the hydrogen content in the breath increases after the ingestion of lactose or fructose and typical complaints (flatulence, abdominal cramps, borborygmus, diarrhea) occur at the same time, proof of lactose or fructose intolerance is assured. Lactulose or glucose breath tests can be used to detect bacterial overgrowth in the small intestine. Lactulose breath tests can also be used to assess orocecal transit time and demonstrate whether hydrogen-producing flora are present in the colon.
In recent years, these indications have been questioned due to the inherent weaknesses of the tests. False negative results of breath tests occur when hydrogen-producing bacteria are absent in the cecum (simultaneous determination of methane only slightly increases sensitivity). When detecting bacterial overgrowth with the lactulose test, false positive results are not uncommon because of the high variability of intestinal transit time [53]. The clinical relevance of these study results is also controversial. Up to 20 g of lactose (400 ml of milk) is often well tolerated by healthy subjects, even if lactase deficiency is genetically present [54]. Patients who overreact to small amounts of lactose in the majority of cases suffer from irritable bowel syndrome and also react to fructose and other fermentable carbohydrates and polysaccharides (FODMAPs).
A further development of the lactulose/FODMAP breath test is the combination with scintigraphy. Here, lactulose is radioactively labeled and, in addition to determining hydrogen in the breath, a scintigraphic image of the abdomen is taken at regular intervals. The movement of lactulose through the gastrointestinal tract thus becomes visible. This method improves specificity and sensitivity of the test while allowing association of intestinal symptoms to fermentation and the location of any bacterial overgrowth [53].
Another application of the 13C breath test is for the diagnosis, respectively eradication control, of Helicobacter pylori. After administration of urea labeled with 13C, the ureases of Helicobacter pylori form 13CO2, the increase of which in the breath indicates colonization of the stomach with these bacteria. Sensitivity and specificity are excellent and replace histological procedures. Therefore, the 13C breath test can be well used to detect Helicobacter pylori infection in the absence of an indication for endoscopy [55]. The most important influencing factor regarding the validity of the test is the pH of the stomach. Therefore, if possible, therapy with PPI should be suspended at least seven days before a scheduled Helicobacter pylori breath test.
Anorectal dysfunction
The continence apparatus, consisting of the rectum and the anal sphincters, is a complex organ system that, in interaction with the pelvic floor, enables defecation and fecal continence. Anal dysfunction is common, especially in women after vaginal births and in the elderly, although many patients do not talk about it because of shame. Fecal incontinence, in particular, is often not reported unless the physician specifically asks about it. Standardized questionnaires and the “Bristol Stool Score” can provide good help. A careful history is important, especially with questions about abdominal and gynecologic surgery, medications (opioids, laxatives), vaginal deliveries, and stool consistency and frequency.
The main indications for anorectal function diagnosis are fecal incontinence, frequent urge to defecate, constipation refractory to therapy and defecation disorders. For the clinical evaluation of these complaints, the combined use of different examination methods is important, such as endoanal ultrasound, anal manometry, rectal barostat measurement and MRI-defecography [56]. Modern, high-resolution anal manometry can demonstrate the function of the sphincter ani internus and externus more accurately and reliably than conventional manometry [57]. In patients with continence problems, anal manometry is combined with endoanal ultrasound so that the structure of the anal sphincter can also be assessed (Fig. 3). These examinations can provide important clues to the etiology of passive, active (urge), or combined fecal incontinence. A functional defecation disorder in the sense of dyssynergic defecation (e.g. paradoxical contractions) can also be recorded. Rectal barostat measurement, usually performed in the same session as anal manometry, provides information about the distensibility and capacity (capacitance) of the rectal reservoir and the sensitivity of the rectum [57]. For example, patients with small rectal volume and low sensitivity may have difficulty maintaining continence even with normal sphincter function.

The result of these tests usually leads to rational treatment of incontinence. Specialized physiotherapy with biofeedback is highly effective in patients with an intact sphincter who are unable to maintain clamping pressure for prolonged periods of time, and also in patients with urge incontinence due to visceral hypersensitivity [58,59]. However, this form of treatment is of little use in pathology that cannot be improved by training (e.g., insufficiency of the sphincter ani internus muscle or severely impaired rectal awareness) [59]. Surgical reconstruction of the anal sphincter is usually only useful in patients with weak clamping pressure due to a major tear in the external sphincter. In special situations, implantation of a pacemaker for sacral neurostimulation may be helpful.
The balloon expulsion test, in which patients are asked to expel a balloon filled with air or water within one minute, provides additional clues as to whether a functional or a structural voiding disorder is present [60]. For defecation disorders caused by pelvic floor dyssynergy, biofeedback treatment is effective [61]. If high-resolution anal manometry and rectal testing are unremarkable and a structural cause of voiding dysfunction is suspected, MRI defecography may be helpful [62]. If this shows a retinating rectocele with intussusception or severe pelvic floor decensus, surgical repair should be discussed.
If no anorectal pathology can be detected and a so-called “slow transit constipation” is a differential diagnosis, the determination of the transit time is helpful (radiodense markers or scintigraphy). In this case, therapy consists of intensifying laxative measures or prokinetic therapy. If the transit time is also normal, the most likely diagnosis is irritable bowel syndrome or impaired perception of the anorectum. In these cases there is often a psychosocial problem, and unfortunately often mental or sexual abuse. This should be asked.
Conclusion
Symptoms caused by abnormal GI motility and function are common. The very nonspecific presentation of symptoms, the lack of a definitive diagnosis by endoscopy and other tests, the coexistence of psychosocial factors, and often the lack of specific therapeutic options often make the management of these so-called functional gastrointestinal disorders very difficult. Initial evaluation of these patients must exclude life-threatening disease and a decision must be made as to whether further investigation is necessary or whether empiric therapy cannot be attempted. In the past, the importance of the functional laboratory for diagnosis and treatment planning in functional diseases was quite low. New technical developments such as high-resolution manometry have led to both a better understanding of the pathophysiology of GI complaints and new, objective classifications of motility disorders. The results of these tests often have a direct influence on the choice of specific therapeutic measures. A definitive diagnosis may be therapeutic in itself, even if no specific treatment is (yet) available. Patients who know the cause of their symptoms are more satisfied, better able to cope with their situation, and are significantly less likely to visit their family doctor or gastroenterologist than patients without this knowledge [64].
Literature list at the publisher
HAUSARZT PRAXIS 2015; 10(12): 32-36











