Recent study findings show that diabetes remission can be achieved in overweight patients with early-stage type 2 diabetes through intensive nutritional therapy with sustained weight loss, and that some patients are able to maintain this remission over several years. Long-term data also confirm that remission has a favorable effect on diabetes-associated complications such as the incidence of cardiovascular disease and renal insufficiency.
A landmark study that showed that remission in type 2 diabetes (T2D) through dietary and behavioral changes is an achievable goal was the Diabetes Remission Clinical Trial (DiRECT), and data from the DiRECT extension phase published in 2024 show that it is possible to maintain remission for up to five years [1,2]. The original DiRECT study included a total of 306 patients aged 20-65 years who had been diagnosed with T2D in primary care within the previous 6 years and who did not require insulin [1]. The body mass index (BMI) at baseline was 27-45 kg/m2. The intervention consisted of discontinuation of glucose-lowering medication and intensive dietary therapy: the target was to abstain from solid food for 3-5 months and instead limit caloric intake to 825-853 kcal daily using specific substitutes, followed by 2-8 weeks of gradual resumption of normal meals in parallel with lifestyle counseling. The subjects in the control group, on the other hand, only received advice on weight reduction. After a period of 1 year, 46% of subjects in the intervention group achieved T2D remission and after 2 years this proportion was 36%. The mean weight loss over 2 years was 7.6 kg. T2D remission was defined as follows: HbA1c value <6.5% (<48 mmol/mol) at least two months after discontinuation of all antidiabetic drugs. In summary, the results of the DiRECT study after two years were remarkable. An extension phase was launched to clarify the question of how things look in the longer term.
5-year data from the DiRECT study gives hope
Some of the test subjects were followed up for a further three years as part of the DiRECT extension phase. While some received low-threshold lifestyle counseling during this period (extension group), the others were not subjected to any measures (control group) [2]. After 5 years, the average weight loss in the extension group (n=85) was 6.1 kg, with 13% (n=11) in remission. Compared to the control group, more HbA1c measurements were <48 mmol/mol (<6.5%; 36% vs. 17%, p=0.0004) in the extension group without the use of glucose-lowering medication (62% vs. 30%, p<0.0001) and the proportion of subjects in remission was also significantly higher in the extension group (34% vs. 12%, p<0.0001). A larger proportion of subjects assigned to the intervention arm in the original DiRECT study showed a weight reduction of >5% since baseline (61% vs. 29%, p<0.0001) and an HbA1c value <48 mmol/mol (29% vs. 15%, p=0.0002) or were in remission (27% vs. 4%, p<0.0001) compared to subjects in the control group. Table 1 shows the proportion of those who achieved a reduction in body weight of at least 10 kg since baseline during the entire observation period (years 1-5) [2]. Of those who were in remission in year 2 after baseline, 26% remained in remission after 5 years. Serious adverse events were less than half as common in the original intervention group (4.8 events per 100 patient-years) as in the control group (10.2 per 100 patient-years, p=0.0080).
Look ADEAD: Remission reduces diabetes-associated complications
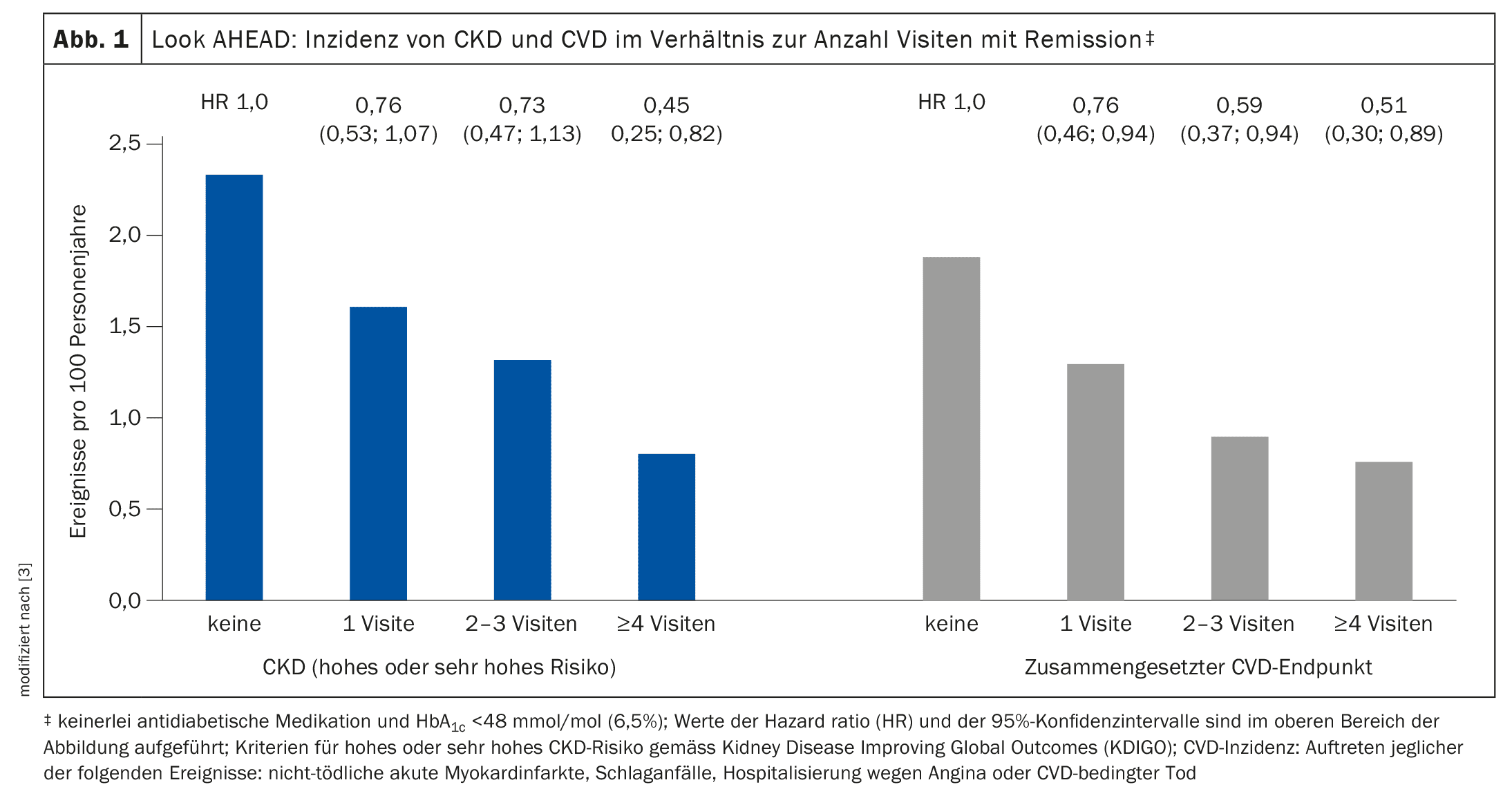
The randomized controlled multicentre Look AHEAD study investigated the effect of intensive lifestyle intervention (intensive group) compared to standard diabetes care and education (standard group) on the incidence of cardiovascular disease (CVD) and chronic kidney disease (CKD) in 45-76-year-old T2D patients with overweight or obesity** over a period of 12 years [3]. The criteria for high or very high CKD risk are based on the definition according to Kidney Disease Improving Global Outcomes (KDIGO). A proportion of 12.7% of the analyzed sample (n=4488) met the criteria for T2D remission in at least one of the follow-up visits. Remission was defined as no antidiabetic medication and HbA1c <48 mmol/mol (6.5%). The prevalence of T2D remission 4 years after baseline was 7.2% in the intensive group, which was 3.5 times higher than in the standard group (2.1%) and approximately twice as high 12 years after baseline (3.7% vs. 1.95%). Further analysis showed that participants with evidence of remission during follow-up had a 33% lower rate of CKD (HR 0.67; 95% CI: 0.52-0.87) and a 40% lower rate of the composite CVD endpoint (HR 0.60; 95% CI: 0.47-0.79). This is based on multivariate analyses adjusted for HbA1c, blood pressure, lipid levels, CVD history, diabetes duration and intervention arm compared to participants without remission. The criteria for high or very high CKD risk are based on the KDIGO definition; CVD incidence refers to the occurrence of non-fatal acute myocardial infarction, stroke, hospitalization for angina or CVD-related death. The extent of the risk reduction was greatest in participants with signs of long-term remission. According to the authors, the fact that study participants with T2D remission had a significantly lower incidence of CKD or CVD can be explained by improvements in weight, fitness, HbA1c and LDL cholesterol.
** BMI ≥27 kg/m2 for insulin-dependent T2D and BMI ≥25 kg/m2 for the other subjects
Congress: Internist update
Literature:
- Lean ME, et al: Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomized trial. Lancet 2018; 391(10120): 541-551.
- Lean ME, et al: 5-year follow-up of the randomized Diabetes Remission Clinical Trial (DiRECT) of continued support for weight loss maintenance in the UK: an extension study. Lancet Diabetes Endocrinol 2024; 12(4): 233-246.
- Gregg EW, et al: Look AHEAD Research Group. Impact of remission from type 2 diabetes on long-term health outcomes: findings from the Look AHEAD study. Diabetologia 2024; 67(3): 459-469.
- KDIGO 2024 clinical practice guideline for the evaluation and man agement of chronic kidney disease. Kidney Int 2024; 105(4S): S117-S314. https://doi.org/10.1016/j.kint.2023.10.018.
- “Diabetology/Nutritional Medicine”, Prof. Andreas Hamann, DGIM Internists Update, livestream, 22-23.11.2024.
HAUSARZT PRAXIS 2025; 20(1): 18-20 (published on 22.1.25, ahead of print)