Sleep serves the physical and psychological recovery as well as the strengthening of the hormone balance or immune system and the detoxification of the brain. But there are some things that can get in the way of restful sleep – obstructive sleep apnea, for example. If excessive daytime sleepiness persists despite adequate therapy, good advice is needed.
After a short After woke up unslept, is certainly every man ever. However, in patients with insomnia, hypersomnia and parasomnia, the body and brain cannot recover and detoxify sufficiently during sleep. The consequences can be serious and have an impact on the cardiovascular system. In addition, there is the psychological burden of excessive daytime sleepiness (EDS) on sufferers. This can have different causes. Obstructive sleep apnea (OSA) is often behind this. During sleep, the muscles and soft tissues of the upper airway slacken, blocking breathing. The body is no longer supplied with sufficient oxygen. In response, the brain sends a wake-up signal to prevent suffocation during sleep. Blood pressure, heart rate and muscle tension increase briefly. After the affected person has woken up briefly – usually unconsciously – and taken a breath, he or she falls back into sleep. For the body, however, these breathing stops lasting between 10-90 seconds mean stress. Loud snoring alternates with shallow breathing and breathing pauses hundreds of times in one night. This can be compounded by night sweats, sudden awakenings, a dry mouth upon waking, and headaches in the morning. Many more people suffer from OSA than is commonly assumed. Estimates suggest that 70-80% of patients are undiagnosed. Typical risk factors for OSA include narrowed upper airways, obesity, a family history of OSA, advanced age, or use of certain sedatives. Often, those affected themselves do not even notice the disease. Only the consequences are noticeable: including difficulty concentrating and excessive daytime fatigue.
EDS: A symptom with far-reaching consequences
EDS is not a disease in its own right, but a symptom of another disease, such as OSA. But narcolepsy or restless legs syndrome can also lead to EDSt. On the neurological level, diseases such as Parkinson’s disease, stroke, traumatic brain injury, CNS infections or neuromuscular diseases can be found. In addition, hypothyroidism, atypical depression, medication side effects, or substance abuse are associated with EDS.
Excessive daytime sleepiness refers to increased sleep pressure occurring during the day, as evidenced by an increased tendency to fall asleep, an irresistible need to sleep, or involuntary falling asleep in inadequate situations. Research has shown that 98.8% of all EDS patients fall asleep while relaxing, 64.6% struggle with unwanted sleep attacks during the day, and 38.2% have already unintentionally fallen asleep while driving. The disease burden is correspondingly high. If the underlying disease is treated adequately, the EDS will usually resolve. However, not always. Approximately 9-22% of OSA patients must be considered to have residual excessive daytime sleepiness (rEDS).
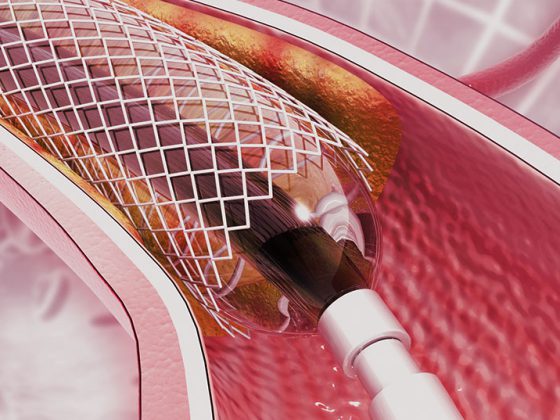
OSA therapy with the help of oxygen
CPAP (conitinuous positive airway pressure) therapy is currently considered the most effective treatment for OSA. During sleep, room air is administered at a slight positive pressure through a mask. This keeps the airways open and can reduce breathing cessations. Studies have shown that this can significantly improve the quality of life in about 70% of patients. However, wearing the mask at night is also quite challenging and is not well accepted or tolerated by all sufferers. In addition, attention should be paid to good sleep hygiene and a regular sleep rhythm. Chin bandages, bite splints or nasal plasters are also available, but have not yet been proven effective. The dual dopamine and norepinephrine reuptake inhibitor solriamfetol was approved as a completely new add-on therapy. It showed rapid improvement in sleep latency lasting over nine hours in OSA patients with rEDS. The effects are due to inhibition of norepinephrine and dopamine transporters in the central nervous system. This increases the concentrations of neurotransmitters in the synaptic cleft. Therefore, it must not be administered in combination with MAO inhibitors. The tablets are taken once a day. Possible side effects include headache, nausea, and lack of appetite.
Further reading:
- www.pharmawiki.ch/wiki/index.php?wiki=Solriamfetol (last accessed on 10.05.2022)
- Eckert DJ: Phenotypic approaches to obstructive sleep apnea – New pathways for targeted therapy. Sleep Med Rev 2018; 37: 45-59.
- Casale M, et al: Obstructive sleep apnea syndrome: from phenotype to genetic basis. Curr Genomics 2009; 10: 119-126.
- Young T, Skatrud J, Peppard PE: Risk Factors for Obstructive Sleep Apnea in Adults. JAMA 2004;291(16): 2013-2016.
- Gasa M, Tamisier R, Launois SH, et al: Residual sleepiness in sleep apnea patients treated by continuous positive airway pressure. J Sleep Res 2013; 22: 389-397.
- Ye L, Pien GW, Ratcliffe SJ, et al: The different clinical faces of obstructive sleep apnea: a cluster analysis. Eur Respir J 2014; 44: 1600-1607.
- Stuck BA, Arzt M, Fietze I, et al: Partial update S3 guideline sleep-related breathing disorders in adults. Somnology 2020; 24: 176-208.
- Fietze I, et al: Diagnosis and therapy of residual daytime sleepiness in patients with treated obstructive sleep apnea Somnology 2021; 25: 99-109.
- Schweitzer PK, et al: Solriamfetol for Excessive Sleepiness in Obstructive Sleep Apnea (TONES 3). A Randomized Controlled Trial. Am J Respir Crit Care Med 2019; 199: 1421-1431.
InFo NEUROLOGY & PSYCHIATRY 2022; 20(3): 22.