After HIV has lost much of its terror in recent years, the Swiss are once again taking more risks in their sexual behavior. Contraception is gladly dispensed with once in a while. Other diseases such as chlamydial infections, gonorrhea and syphilis have become significantly more important.
In the last decade, the number of reports of so-called “sexually transmitted infections” (STI) has more than doubled in Switzerland; only in the case of HIV has the situation remained stable so far. The most common STDs are chlamydial infections. “Today, as a rule, people no longer die from HIV. Since 1995, or rather since the introduction of highly effective drugs against HIV, the disease has clearly lost its terror, which is why more people are having unprotected sex again and thus more cases of other STIs are occurring. Sexual risk behavior has increased sharply,” explained speaker Prof. Philip Tarr, M.D., co-chief physician and head of Infectious Diseases and Hospital Hygiene, Baselland Cantonal Hospital, Bruderholz.
This also serves as an explanatory model in the many chlamydia reports. In addition, it can be assumed that the inhibition threshold for diagnostics is low. “We test more frequently and thus find more (asymptomatic) cases,” is the hypothesis. But why is there so much testing for chlamydia? First, chlamydia mainly affects young women and can lead to infertility and ectopic pregnancy. This scares many patients, but also doctors. Second, 85-90% of affected individuals have no symptoms and can only be detected by testing. “However, severe reproductive complications following chlamydial infections are much rarer than previously thought,” he said. “This is shown by large studies and meta-analyses on the topic.” Whether or not chlamydia screening is done, pelvic inflammatory diseases (PID) are decreasing in many countries. Overall, the numbers are so low that comprehensive screening would not be profitable. Screening young, sexually active, asymptomatic women for chlamydia can therefore not be recommended in view of the high costs of a screening program and the insufficient data available (Table 1).

With regard to chlamydia diagnostics, the urine sample in women is less sensitive than a vaginal/cervical smear. In men, a urethral or meatus smear appears to be similarly sensitive to first-stream urine.
Treatment is with doxycycline 100 mg 1-0-1 for seven days or azithromycin 1000 mg as a single dose. The latter should not be given for rectal infections. The trend in the future could be toward preference for doxycycline (topic of discussion at present). The advantage of azithromycin is that it is administered once and can therefore be taken directly in front of the doctor. Unlike gonococci, there is no known resistance in chlamydia treatment.
Gonorrhea
In the last ten years, gonorrhea reports in Switzerland have tripled. Men are affected more often than women, MSM (men who have sex with men) more often than heterosexuals. “Gonococcal urethritis is asymptomatic more often than one might think, especially in women. Gonococcal proctitis/pharyngitis is asymptomatic in over 90% of cases, but is an important reservoir in terms of partner infection,” Prof. Tarr explained.
PCR can reliably detect the bacterium, but not its sensitivity to antibiotics. Due to the problematic resistance situation, a gonococcal culture should therefore always be additionally performed before any antibiotic treatment in symptomatic patients or asymptomatic sexual partners of gonorrhea patients. Only this allows resistance testing. In women, as with chlamydia, initial urine PCR is not recommended (insufficient sensitivity), but a vaginal/cervical swab is recommended. In men, a superficial meatus smear is probably equally sensitive as a (deep painful) urethra smear or first-stream urine.
Oral treatment is now no longer recommended because resistance to cefixime is increasing significantly around the world. Ceftriaxone 500 mg i.m. and azithromycin 1 g per os once are first-line agents for uncomplicated gonorrhea (also during pregnancy and lactation). Treatment of sexual partners is the same as for chlamydia. The risk of partners also being infected is very high (>50%), which is why partner therapy is an integral part. Therapy is generously retrospective, i.e. all sexual partners of the last 60 days. Diagnostic workup (PCR and culture) is recommended, but one should treat the same day without waiting for the result. Sexual contact is not recommended until asymptomatic and for seven days after the start of therapy. Because multiple infectious diseases are often present, one should look for other STIs such as chlamydia, syphilis, and HIV. It is worth taking a look at the vaccination card: Have you been vaccinated three times against HBV?
Syphilis – out of control?
With 50-75% of infected sexual partners, syphilis is a highly infectious STD. Even if sexual partners are asymptomatic on examination, approximately 30% will still develop clinically apparant syphilis without preventive therapy. Thus, after syphilis exposure, preventive treatment is recommended.
The FOPH abolished the reporting requirement for syphilis in the 1990s after the trend had been downward for several years. In the last few years, there was a sudden increase in the number of syphilis cases reported. Today, there are over 1000 cases per year and the situation seems to be out of control.
“In the last decade, an increase of four times was found in Swiss men,” the speaker said. “These form the main group, accounting for 89% of all cases in 2015, with 57% of syphilis patients reporting sex with men. Nevertheless, heterosexuals and women must not be forgotten.”
Genital herpes (HSV) – psychological stress
Most infections originate from asymptomatic individuals (although symptomatic individuals generally shed more virus). Because: only 10-25% of HSV 2-seropositive individuals know they have genital herpes and are contagious. Virus excretion occurs genitally even without symptoms – on average on 10-20% of all days. Overall, HSV 2 is more often responsible for genital manifestations than HSV 1; HSV 1 usually makes an orolabial clinic. It is often seen in the context of non-sexual infection in childhood, although this form of transmission has decreased, probably because of better hygiene conditions. More teens start HSV 1-seronegative in sexual activity. On the other hand, oral sex is practiced more frequently today than 25 years ago. Overall, genital HSV 1 is increasing.
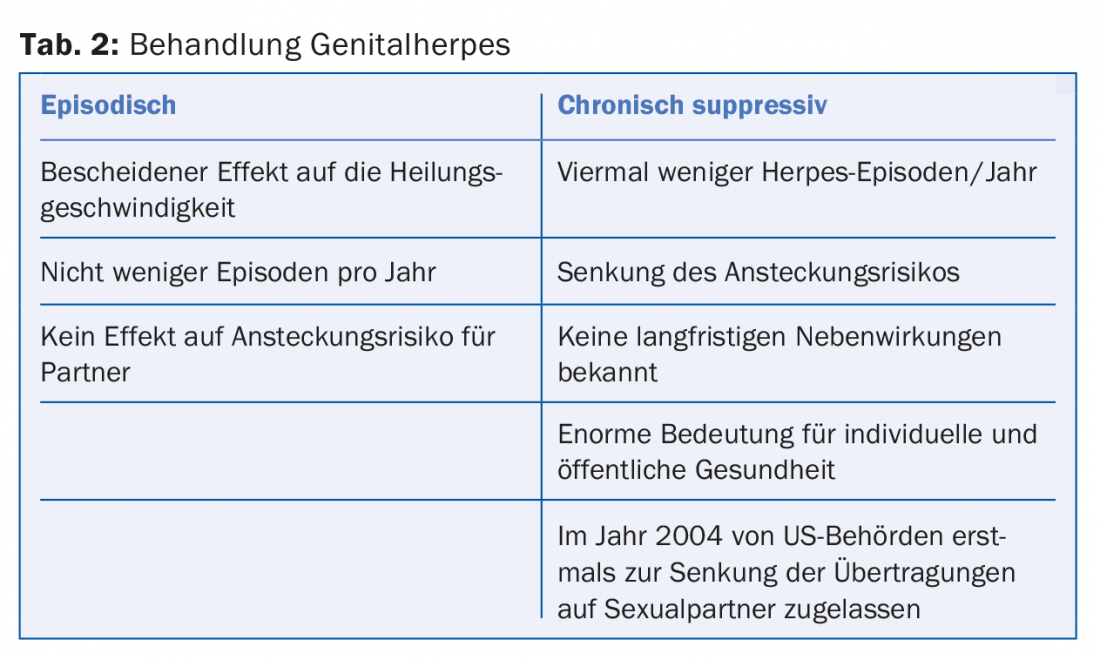
Herpes (genitalis) can be psychologically very stressful, which also has relevance for treatment. The episodic regimen of starting therapy at prodromes/symptoms is generally not very effective. In contrast, the established chronic suppressive regimen with daily use of a drug (in this case, e.g., Valtrex®) – comparable to, for example, blood pressure therapy – leads to four times fewer episodes/year and a lower risk of infection of sexual partners. This with a good safety profile and positive effects on psychological well-being. It is therefore used for frequent recurrences and psychological morbidity (Table 2). Evidence that local therapies are effective is lacking.
HIV – Key role of the primary care provider
“The FOPH sees an encouraging, albeit slight, downward trend in the number of new HIV diagnoses in Switzerland since 2009. Unfortunately, about one-third of all newly diagnosed HIV patients are already in a late stage. If these patients had been diagnosed with the disease five to ten years ago, they would have been spared a lot of trouble,” says Prof. Tarr. Today, hardly any “druggies” are infected with HIV, but mainly MSM and migrants from countries with high HIV prevalence (e.g. Africa). Older persons are particularly likely to miss HIV because less sex and therefore less sexual risk behavior is suspected. However, new diagnoses are not uncommon even in people over 50 years of age.
“Primary care physicians play a key role in diagnosis. They should be remembered for acute mononucleosis, prolonged or unclear disease, MSM, immigrants from high-endemic countries, and IV drug use.” In family practice, HIV testing should be done generously to avoid late diagnoses. There is no need for a written consent form or a detailed questioning of the sexual behavior, it is sufficient to inform the patient verbally that he/she will be tested for HIV. If the patient refuses, the test must be waived.
The rapid test costs the patient CHF 50 in cash and is anonymous. After 30 minutes, he receives the result (if HIV is present, the doctor comes for a venous blood sample). The “normal” HIV test is not anonymous. It includes a serology (ELISA) and – only in the sense of a confirmatory test – a viral load determination (PCR/HIV-RNA, except in cases of suspected HIV primoinfection, since in this case the HIV-RNA is already detectable, but the HIV serology may still be negative).
Today, over 90% of HIV-positive people in Switzerland receive appropriate therapy (usually a three-drug combination). Since 2010, there have been so-called “single tablet regimens”: Atripla®, later Eviplera® and Stribild® in 2013, Triumeq® in 2015, and since last year Genvoya®.
Source: General Internal Medicine Update Refresher, May 10-13, 2017, Zurich.
DERMATOLOGIE PRAXIS 2017; 27(3): 41-43











