Research into treatments for chronic kidney disease has stagnated for a long time. Now there is good news. SGLT2 inhibitors and GLP-1 are promising hopefuls, as recent findings show.
Chronic kidney disease is a serious complication of type 2 diabetes and is associated with an increased risk of end-stage renal failure and a reduction in life expectancy by several years. That the SGLT2 inhibitors empagliflozin, canagliflozin, and dapagliflozin and the GLP1 agonists liraglutide and semaglutide reduce major adverse cardiac event (MACE) risk has been repeatedly demonstrated and replicated [1,2]. As a look at the data of different cardiovascular endpoint studies shows (EMPA-REG, CANVAS, DECLARE), SGLT2 inhibitors also reduce hard renal endpoints (doubling of creatinine, 40% decrease in eGFR, end-stage renal failure, renal mortality) by 40-50%, explains PD Dr. med. Harald Seeger from the University Hospital Zurich [3]. Globally, there is a trend toward an increase in the prevalence of type 2 diabetes and chronic kidney failure (CKD) [4,5]. According to data from the USA, about 30-50% of cases of CKD are caused by diabetes and about 50% of all diabetics develop CKD despite treatment [6–8]. Mortality and risk of cardiovascular complications depend on the extent of renal insufficiency and albuminuria. Thus, the worse the eGFR and the higher the albimunirie values, the higher the cardiovascular mortality risk [9]. “Regarding prophylaxis of cardiovascular complications, a lot has happened in the past 20 years,” said the speaker [3]. However, this does not apply to measures to prevent the progression of renal failure in diabetic patients, where until recently only ACE inhibitors and angiotensin receptor agonists were available for this purpose. However, recent progress has been made in this regard, with representatives of the SGLT2 inhibitor and GLP1 agonist classes of oral antidiabetic agents receiving marketing approval.
High risk reduction of renal events
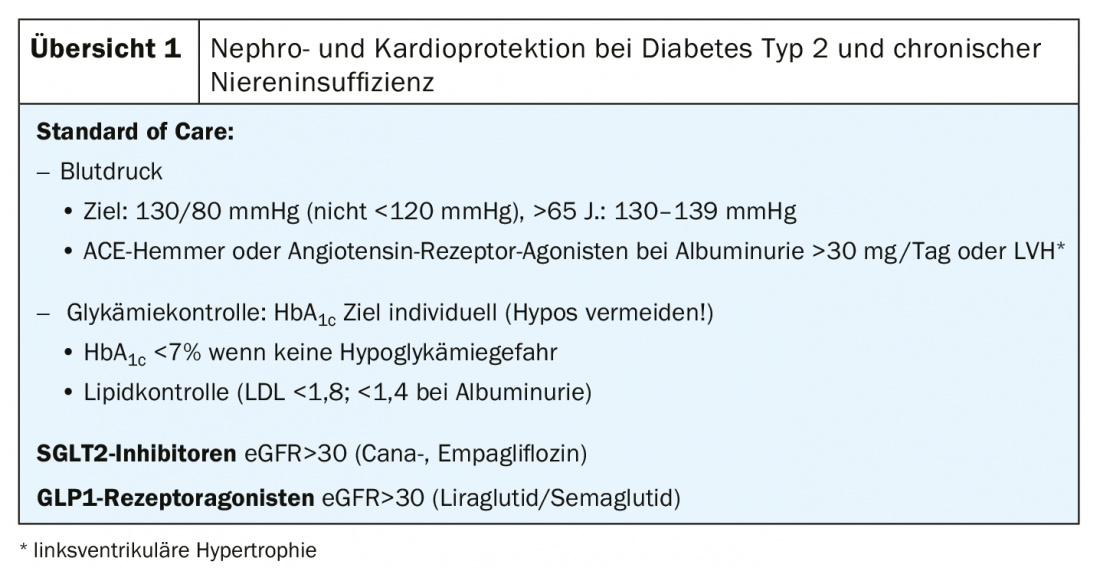
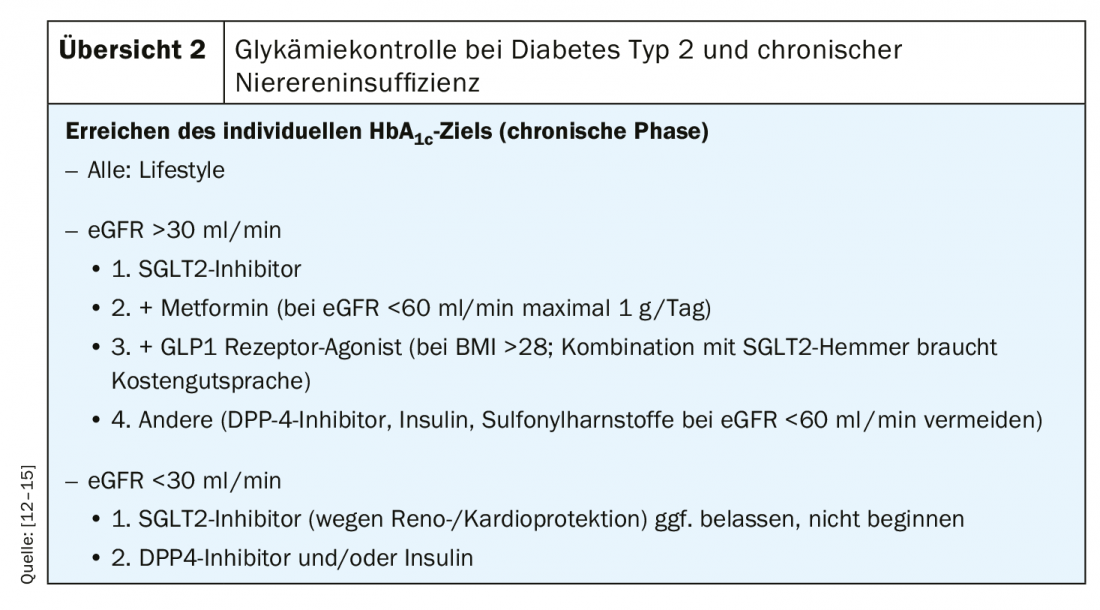
The therapy of type 2 diabetic patients with CKD is based on two pillars [3]: 1) Nephro- and cardiovascular protection, 2) Glycemic control [12,13] (Overview 1 and 2). In the double-blind randomized study CREDENCE. [10] demonstrated that the SGLT2 inhibitor canaglifozin met the primary renal endpoint in patients with diabetic nephropathy (eGFR=30-90 ml/min/1.73 m2; albimunirie 300-5000 mg/g) reduced by 30% compared to placebo (combined endpoint: terminal renal failure=ESKD, doubling creatinine, renal or cardiovascular mortality) (HR 0.70; 95% CI 0.59-0.82; p=0.00001). [11]. Hard renal endpoints in patients with diabetic nephropathy reduced by 30% within 2.6 years [11]. As it turned out, the stabilizing effect of the sodium glucose co-transporter 2 (SGLT2) inhibitor canaglifozin on eGFR in CKD was independent of a reduction in HbA1c [11]. It is the first substance since ACE inhibitors and angiotensin receptor agonists to reduce the risk of progression of chronic kidney failure (CKD). In addition, treatment with canagliflozin results in a 31% reduction in cardiovascular endpoints (cardiovascular mortality, hospitalization for heart failure) (HR 0.69; 95% CI 0.57-0.83; p<0.001) [11]. Furthermore, canagliflozin causes stabilization of eGFR in CKD independent of HbA1c reduction [11]. For successful therapy with SGLT inhibitors, the following points should be considered [3]: In the relevant studies, canagliflozin and empagliflozin were used in patients with eGFR in the range 30-90 ml/min. Dapaglifozine is not approved at eGFR <60 ml/min. The patient should be informed that treatment with SGLT2 inhibitors should be interrupted in case of acute illness (infection, diarrhea/vomiting). The same applies to fasting (e.g., prior to surgery) due to an increased risk of ketoacidosis. If genital mycoses develop, topical therapy is recommended. If loop diuretics are prescribed concomitantly with SGLT2 inhibitor therapy, the dose should be halved before starting SGLT-2 inhibitor treatment.
Source: FOMF Zurich
Literature:
- Zelnicker TA, et al: SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 2019; 393 (10166): 31-39.
- Zelnicker TA, et al: Comparison of the Effects of Glucagon-Like Peptide Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors for Prevention of Major Adverse Cardiovascular and Renal Outcomes in Type 2 Diabetes Mellitus. Circulation 2019; 139 (17): 2022-2031.
- Seeger H: Slide presentation PD Dr. med. Harald Seeger, University Hospital Zurich. Cardio-renal complications in diabetes mellitus type 2. Symposium Mundipharma, FOMF Internal Medicine – Update Refresher, 03.12.2019, Zurich.
- NCD-Risk Factor Collaboration: Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016; 387: 1513-1530.
- Kirchhoff S.: Medicare coverage of end-stage renal disease (ESRD). https://fas.org, last accessed Dec. 17, 2019.
- Webster AC, et al: Chronic Kidney Disease. Lancet 2017; 389: 1238-1523.
- Liyanage T, et al: Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 2015; 385: 1975-1982.
- http://diabetesatlas.org/resources/2017-atlas.html, last accessed Dec. 17, 2019.
- Fox C, et al: Association of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 2012; 380(9854): 1662-1673.
- Jardine MJ, et al: The Canagliflozin and Renal Endpoints in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) Study Rationale, Design, and Baseline Characteristics. Am J Nephrol 2017; 46(6): 462-472.
- Perkovic V, et al: Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med 2019; 13: 380(24): 2295-2306.
- Cosentino N, et al: Rationale, Experimental Data, and Emerging Clinical Evidence on Early and Preventive Use of Levosimendan in Patients with Ventricular Dysfunction. Eur Heart J Cardiovasc Pharmacother. 2019 Nov 5. pii: pvz065.
- Sarafidis P, et al.: SGLT-2 inhibitors and GLP-1 receptor agonists for nephroprotection and cardioprotection in patients with diabetes mellitus and chronic kidney disease. A consensus statement by the EURECA-m and the DIABESITY working groups of the ERA-EDTA. Nephrol Dial Transplant 2019; 34(2): 208-230.
- ADA Standards of Medical Care in Diabetes. Diabetes Care 2018; 41st Supp.
- Davies MJ, et al: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2018; 61(12): 2461-2498.
HAUSARZT PRAXIS 2020; 15(1): 37-38 (published 1/25/20, ahead of print).