Adequate wound care is an essential component of preventive and post-interventional measures. Wound dressings play an important role in the prophylaxis and therapy of pressure ulcers as recent evaluation studies show.
Decubital ulcers are associated with an increased risk of systemic infections and can lead to significant impairment of well-being. In the currently available spectrum of intervention measures, in addition to debridement and antibiotic measures (in case of infection), the adequate selection of the wound dressing, among other things, is crucial [1]. A Cochrane review and a secondary analysis published in the International Wound Journal stated a few years ago that there is a need for further research on the evaluation of wound dressings [2,3]. Two randomized-controlled trials, with data published in 2019 and 2018, provided informative results in this regard, which may help optimize wound management.
Chronic wounds: painful and prone to infection
Painful pressure ulcers in immobile patients are one cause of chronic wounds. Patients with limited mobility (e.g., post-traumatic, post-operative) are particularly at risk for pressure ulcers. Patients with reduced sensitivity due to polyneuropathy or a disease of the central nervous system are also at increased risk. Early detection of a pressure ulcer can have a positive effect on the chances of recovery. Wound care depends on the type and severity of the disease. For small and dry wounds, a sterile dressing may be sufficient. Wet wounds should first be cleansed with sterile saline or wound irrigation solution. Suitable dressing materials include foam wound dressings or (silicone-coated) foam dressings, which are designed to keep the wound moist underneath without causing the tissue to stick to the dressing to promote wound healing. If the pressure ulcer is already more advanced with dead tissue in the wound, manual removal may be necessary.
Wound dressings as an important therapy component
The range of prevention and treatment options has expanded with modern wound dressings. The selection of the appropriate dressing form for the respective wound plays an important role. As a basis for adequate wound care, classification is crucial (e.g., according to criteria of the international classification system NPUAP/EPUAP) [4,5]. A decubitus diagnosis and the differential diagnosis can be confirmed by a high interrater reliability [4]. A description of the extent and nature of tissue damage and differentiation from other types of wounds that have similar characteristics to pressure ulcers is critical (e.g., venous ulcer, neuropathic ulcer, incontinence-related dermatitis, intertrigo) [4,5].
Risk factors for pressure ulcers vary interindividually, which should be taken into account when choosing the appropriate wound dressing. Foam dressings are made of polyurethane or silicone foam. They are characterized by their ability to absorb large amounts of exudate. With this type of dressing, routine evaluation of the skin condition does not require replacement of the dressing and no skin lesions are induced at the site of adhesion. Other advantages of silicone- or polyurethane-containing foam dressings: well-suited for medium to heavy exudation, as wound filler without film backing, also available with film backing, with adhesive edge (for occlusion), non-adherent with wound base (wound conditioning).
Evidence-based efficacy of foam dressings containing silicone or polyurethane
Recent study findings confirm that foam dressings as an add-on to standard wound prevention and treatment have been shown to be effective in reducing the incidence of pressure ulcers and erythema:
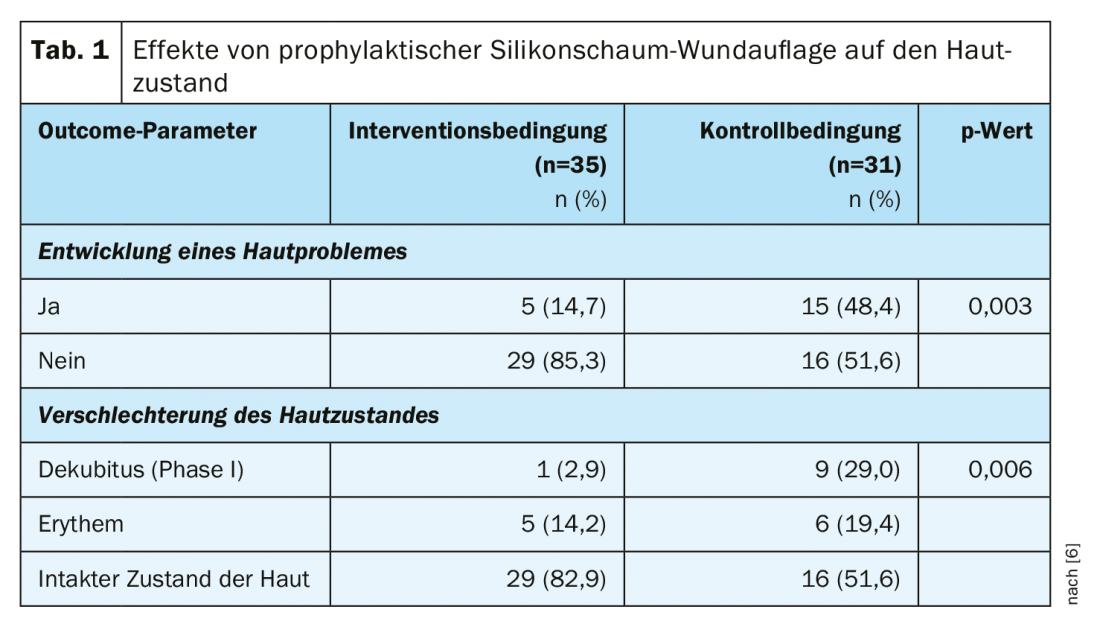
- In a randomized-controlled study published in 2019, a prophylactically applied highly absorbent and gently adherent polyurethane foam dressing with silicone coating (Allevyn™ Gentle Border) [9] was shown to have a positive effect on the skin condition of ICU patients (mean age 61.03 y) (Table 1) [6]. Subjects were randomly assigned to the intervention condition (standard therapy plus polyurethane foam dressing in the sacral region) or the control condition (standard therapy only). Monitoring of the wound was performed every three days. The incidence of pressure ulcers was significantly lower in the experimental group (n=35) than in the control group (n=31): 2.9% vs. 29% (p<0.006). In addition, erythema occurred significantly less frequently (14.2% vs. 19.4%).
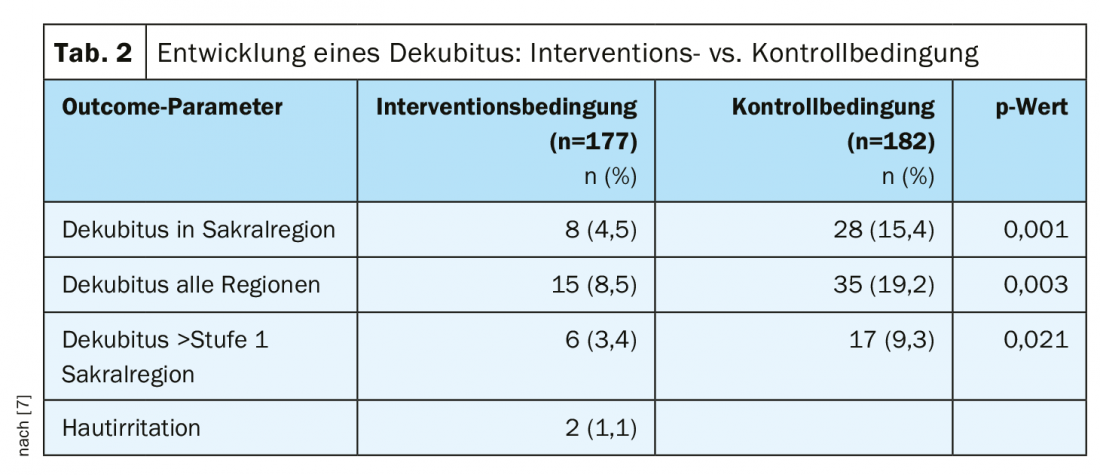
- In a randomized-controlled trial published in 2018 by Forni et al. [7], demonstrated a reduction in pressure ulcers in hospitalized elderly patients (≥65 yrs) after hip fracture (Table 2). The sample consisted of patients with hip fracture (experimental group: n=177, control group: n=182). In the intervention condition, a gently adherent, highly absorbent silicone foam dressing (Allevyn™ Life) [10] was applied as an add-on to standard prevention. In the control condition, only standard prophylactic measures were performed. The incidence for pressure ulcers was 4.5% in the experimental group vs. 15.4% in the control group (p=0.001). The relative risk of pressure ulcer proved to be significantly lower in the intervention condition (RR 0.29; 95% CI 0.14-0.61). The number needed to treat was 9 (95% CI 6-21). In those cases in the experimental group in which pressure ulcers occurred, this did not occur until day 6 (vs. day 4 in the control group).
Standard measures of wound prophylaxis and treatment included adjustment of mattresses depending on the “Braden score”, skin cleansing and care, hydration, and regular mobilization of the patient.
Conclusion
The positive effect of prophylactic application of wound dressings from previous studies [2,3] has been confirmed in recent studies [6,7]. Specifically, wound dressings with good adhesion and silicone coating as an add-on measure to standard treatment led to a reduction in pressure ulcers and erythema [6,7]. Prevention of erythema due to ischemic tissue changes is an important factor in reducing pressure ulcers. Thus, these wound dressings are an effective prophylactic strategy, which proved to be most effective when combined with standard preventive measures. Subepidermal moisture (“SEM”) proved to be an indicator for the diagnosis of a pressure ulcer at an early stage [6]. Pressure ulcers after a hip fracture are common and have a negative effect on the patient’s condition and course. It has been shown that pressure ulcers in the sacral region were reduced in a wound dressing with polyurethane foam and silicone coating [7].
Due to the good adhesion of these wound dressings, it is a cost-effective method. In addition, no skin lesions are induced upon removal and regular evaluation of the skin condition without changing the dressing is unproblematic.
Literature:
- Boyko TV, et al: Review of the Current Management of Pressure Ulcers. Adv Wound Care (New Rochelle). 2018 Feb 1; 7(2): 57-67.
- Clark M, Black J, Alves P, et al. Systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. Int Wound J. 2014;11: 460-471.
- Moore ZEH, Webster J. Dressing and topical agents for preventing pressure ulcers. Cochrane Database Syst Rev. 2013;8:CD009362.
- EPUAP (European Pressure Ulcer Advisory Panel): Prevention and Treatment of Pressure Ulcers: Quick Reference Guide, www.epuap.org/wp-content/uploads/2016/10/quick-reference-guide-digital-npuap-epuap-pppia-jan2016.pdf
- NPUAP (National Pressure Ulcer Advisory Panel): Prevention and Treatment of Pressure Ulcers: Clinical Practice Guidelines, www.internationalguideline.com/static/pdfs/NPUAP-EPUAP-PPPIA-CPG-2017.pdf
- Lee Y, Kim JY, Shin WY, Yeon YH: Use of prophylactic silicone adhesive dressings for maintaining skin integrity in intensive care unit patients: A randomized controlled trial. Int Wound J. 2019;16(Suppl. 1): 36-42.
- Forni C, et al: Effectiveness of using a new polyurethane foam multi-layer dressing in the sacral area to prevent the onset of pressure ulcer in the elderly with hip fractures: A pragmatic randomized controlled trial. Int Wound J 2018; 1-8. DOI: 10.1111/iwj.12875.
- Brindle CT. Wound-product selection and innovations: Identifying high-risk ICU patients use of an absorbent soft silicone self-adherent bordered foam dressing to decrease pressure ulcers in the surgical trauma ICU patient. J Wound Ostomy Continence Nurs 2009; 36: 27.
- Allevyn™ Gentle Border, Smith & Nephew GmbH, www.smith-nephew.com/deutschland/fachgebiete/wundmanagement/schaumverbande/sanft-haftend-liste/allevyn-gentle-border/
- Allevyn™ Life, Smith & Nephew GmbH, www.smith-nephew.com/deutschland/fachgebiete/wundmanagement/schaumverbande/allevyn-life/
DERMATOLOGIE PRAXIS 2019; 29(5): 44-46