Sperm allergies are IgE-mediated reactions against components of seminal fluid. The main allergen is prostate specific antigen (PSA). Therapeutic measures include exposure prophylaxis by condoms or hyposensitization by exposures to seminal plasma. The desire to have children does not have to be abandoned because of a sperm allergy.
Intolerance reactions after contact with human semen can be of diverse nature and need not always be attributed to a true sensitization to allergens contained in seminal plasma [1,18]. Since symptoms usually occur after sexual intercourse or generally in the context of sexual activity, true semen allergies are sometimes difficult to distinguish from female allergic reactions to latex (condoms), spermicidal substances (vaginal contraceptives), local anesthetics (in some condoms), components of lubricants, or allergens that occur in semen after oral ingestion by the male (foods, drugs) if the history, findings, and diagnosis are not accurate. Discomfort following exposure to semen can also be triggered by prostaglandins, which cause uterine contractions in women [13].
IgE-mediated (type I) immediate-type allergic reactions to specific components of seminal plasma are rarely described but, with suspected under-reporting, are likely to be more common than reported. In the United States alone, approximately 40,000 affected women are thought to have localized or generalized reactions [16].
The first report on sperm allergy was published by Specken in 1958; the first publication in English was in 1967 [7]. More than 40 years ago, it was pointed out that the first diagnosis was more often made by the affected women than by the treating physicians [5].
Symptomatology
The clinical symptoms of sensitization to seminal plasma cover a wide spectrum, ranging from local reactions to anaphylactic shock. Subjective and objective symptoms occur immediately or within an hour of exposure to semen and, in rare cases, somewhat later. Systemic reactions usually begin immediately in patients, whereas local reactions begin with a shorter time delay [12]. Local reactions include itching, burning, erythema, and edema in the vulvar area (vulvovaginitis) or other sites of semen contact. In addition, the occurrence of pelvic pain has also been reported [7].
Systemic reactions due to sensitization to components of seminal plasma manifest as dyspnea, dysphagia, rhinoconjunctival symptoms, generalized urticaria (Fig. 1), angioedema, gastrointestinal symptoms with vomiting or diarrhea, exacerbation of preexisting atopic eczema, or anaphylactic shock.

In a review of casuistry from a total of 32 patients with reactions to their partners’ semen, Presti and Druce found reports of anaphylactic reactions and dyspnea in 22% of cases each, while pruritus, local pain, and edema were most common at 47-84% [12].
Most women with allergic reactions to seminal plasma components are between 20 and 30 years old [12].
Predisposing factors
In a high proportion of women (40-50%), symptoms of hypersensitivity to semen occur after the first sexual intercourse [12,16]. This may indicate that the antigens present in seminal plasma cross-react with other allergens or that patients have become sensitized by non-intravaginal sperm exposures even before the first sexual intercourse.
More than 50% of affected women also have other allergic symptoms such as allergic rhinoconjunctivitis or a positive family history of atopic diseases (hay fever, atopic eczema, bronchial asthma) [17].
The triggering allergen in seminal plasma
The site of origin of the allergen was suspected early on to be the prostate. Positive responses were noted after testing with prostate expressions and extractions from prostate tissue on skin [14]. Scratch and intradermal tests were also positive when seminal plasma from vasectomized men was used [9].
It is likely that several allergens are responsible for triggering IgE-mediated allergies to seminal plasma. A major allergen is the prostate specific antigen PSA [19]. Human PPE exhibits high cross-reactivity to the major allergen Can f 5, which is present in dog dander and other dander [2]. Therefore, sensitization to Can f 5 may lead to allergy to seminal plasma in humans.
Diagnostics
The central component of diagnostics is a careful anamnesis. Only through these can indications of sensitization to other antigens not found in seminal plasma (latex in condoms) be obtained in advance. Particular attention should also be paid to atopy history, time course and extent of symptoms after exposure to semen (onset and duration of symptoms, systemic or local only).
An important indication of an allergy to seminal plasma is the avoidance of symptoms by the use of condoms.
For diagnosis in vitro, the detection of specific IgE antibodies against seminal plasma in the serum of the patients is suitable. In addition, the determination of total IgE in serum is always recommended. The detection of specific antibodies against seminal plasma is not always successful despite appropriate clinical findings.
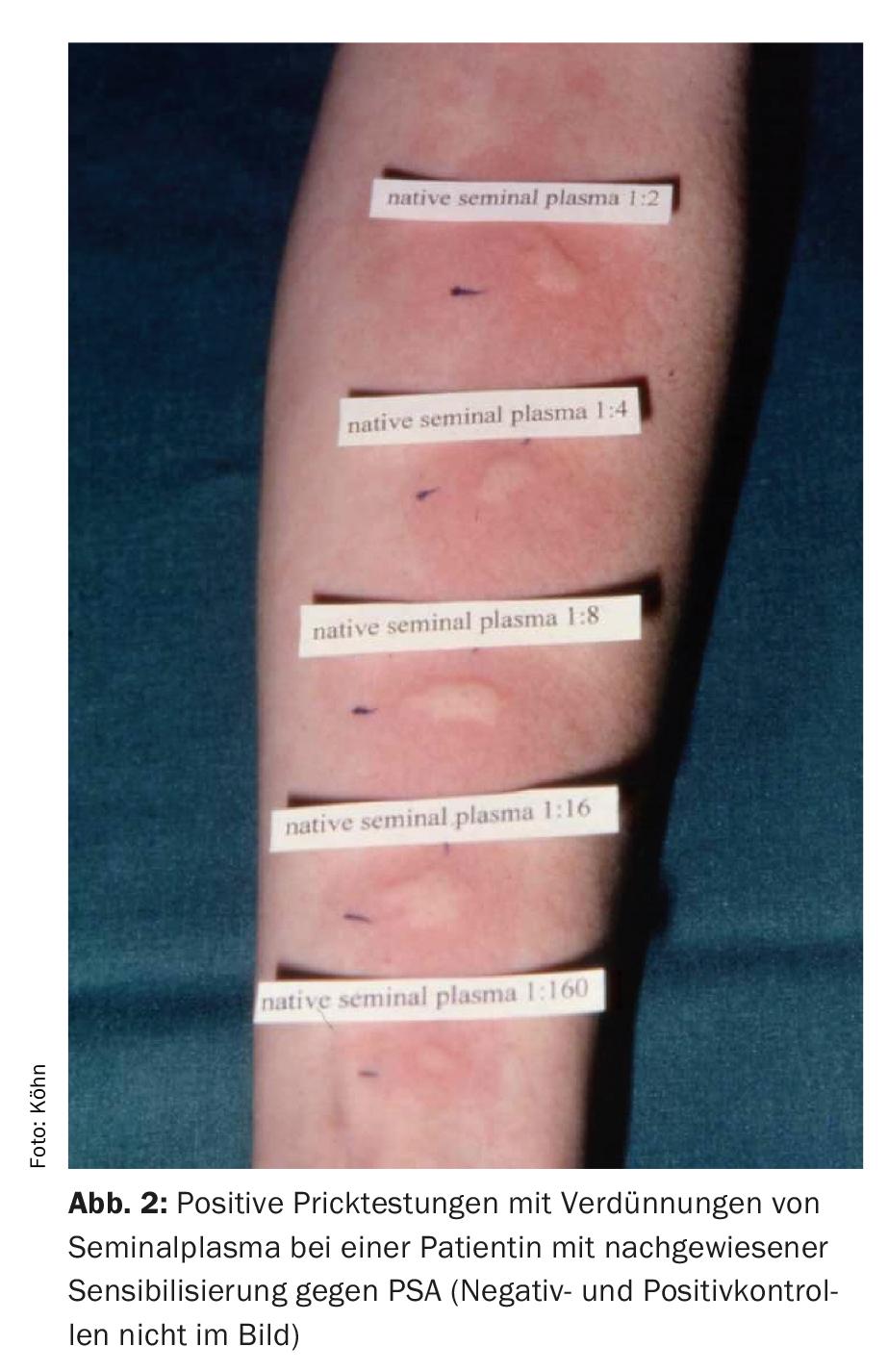
Prick and intradermal tests are of great importance in the allergological diagnosis of sperm allergies (Fig. 2) . Depending on the extent of sensitization, skin testing may have to be performed under emergency medical standby. Prior to this, sperm and seminal plasma are separated by centrifugation. As a rule, testing is also performed with the spermatozoa pellet. However, reactions are only expected against seminal plasma in various dilutions.
Even if the sexual partner’s ejaculate is used, a possible risk of infection must be minimized by prior serological (HIV, hepatitis, lues) and microbiological examinations of the ejaculate and the consent of the partner must be obtained. Skin testing is positive in the vast majority of cases [12].
Therapeutic options
The first immediate recommendation is exposure prophylaxis. Sexual intercourse should be performed only with the use of condoms. Among these, symptoms may regress and prick tests may become negative with long allergen abstinence [8]. In rare cases, sensitization to seminal plasma and latex may occur simultaneously [20]. In this case, latex-free condoms must be recommended.
If the medical history indicates a high degree of sensitization with generalized and threatening reactions (drop in blood pressure, shortness of breath), the patient should already be prescribed an “emergency kit” during the initial consultation.
Antihistamines, when taken before sexual intercourse, may improve symptoms in some patients [4].
In addition to exposure prophylaxis, various targeted exposures to seminal plasma have been attempted, which are referred to as “hyposensitizations” but actually result in the development of tolerance through continuous allergen exposure. The first successful report was by Blair and Parish, who injected diluted seminal plasma in increasing concentrations twice weekly for six months [3].
Mittman et al. initiated rapid hyposensitization (two days) with chromatographically separated seminal plasma fractions in a 24-year-old woman with anaphylactic reactions after exposure to semen [10]. Subcutaneous injections of the allergologically relevant fractions were then given three times a week for four months. Sexual intercourse could be performed without symptoms after the end of hyposensitization. The couple was instructed to perform unprotected intercourse every 2-3 days to maintain immunity. No further symptoms occurred during the following six months.
A different form of tolerance development was chosen by Park et al. [11]. They exposed the vaginal mucosa to 2 ml of the husband’s seminal plasma diluted by a factor of 10-5 and increased the exposures at 45-minute intervals with gradual decreases in dilution by a factor of 10. Thereafter, the couple performed sexual intercourse at 2-3-day intervals without symptoms. Prolongation of the interval to five days resulted in mild localized itching and swelling of the vulva. After six months, spontaneous pregnancy occurred.
For the future, specific hyposensitization against the relevant allergen PSA is desirable.
Sperm allergy and infertility
If unprotected sexual intercourse is not possible due to the symptomatology with an existing desire to have children, pregnancies can occur after intrauterine inseminations with washed spermatozoa [6]. Alternatively, there is also the possibility of assisted reproduction.
Take-Home Messages
- Reactions to seminal plasma are not always specific allergies to components of seminal plasma.
- True semen allergies are IgE-mediated reactions against typical components of seminal fluid.
- The essential allergen is the prostate specific antigen (PSA). PSA exhibits high cross-reactivity to the major allergen Can f 5 in dog dander.
- The first line of therapy is exposure prophylaxis through condoms. Hyposensitization by exposures to seminal plasma is possible.
- The realization of a child’s wish is possible even with proven sperm allergy.
Literature:
- Allam JP, et al: Sperm allergy. Dermatologist 2015; 66: 919-923.
- Basagaña M, et al: Involvement of Can f 5 in a case of human seminal plasma allergy. Int Arch Allergy Immunol 2012; 159: 143-146.
- Blair H, et al: Asthma and urticaria induced by seminal plasma in a woman with IgE antibody and T-lymphocyte responsiveness to a seminal plasma antigen. Clin Allergy 1985; 15: 117-130.
- Chang TW: Familial allergic seminal vulvovaginitis. Am J Obstet Gynecol 1976; 126: 442-444.
- Frankland AW, et al: Anaphylactic sensitivity to human seminal fluid. Clin Allergy 1974; 4: 249-253.
- Frapsauce C, et al: Successful pregnancy by insemination of spermatozoa in a woman with a human seminal plasma allergy: should in vitro fertilization be considered first? Fertil Steril 2010; 94: 753.e1-3.
- Halpern BN, et al: Clinical and immunological study of an exceptional case of reaginic type sensitization to human seminal fluid. Immunology 1967; 12: 247-258.
- Kroon S: Allergy to human seminal plasma: a presentation of six cases. Acta Derm Venereol 1980; 60: 436-439.
- Levine BB, et al: Allergy to human seminal plasma. N Engl J Med 1973; 288: 894-896.
- Mittman RJ, et al: Selective desensitization to seminal plasma protein fractions after immunotherapy for postcoital anaphylaxis. J Allergy Clin Immunol 1990; 86: 954-960.
- Park JW, et al: Seminal plasma anaphylaxis: successful pregnancy after intravaginal desensitization and immunodetection of allergens. Allergy 1999; 54: 990-993.
- Presti ME, et al: Hypersensitivity reactions to human seminal plasma. Ann Allergy 1989; 63: 477-481.
- Sahmay S, et al: The effect of intrauterine insemination on uterine activity. Int J Fertil 1990; 35: 310-314.
- Siraganian RP, et al: Immunologic studies of a patient with seminal plasma allergy. Clin Immunol Immunopath 1975; 4: 59-66.
- Specken JLH: Een merkwaardig geval van allergie in de gynecologie. Ned Tijdschr Verloskunde 1958; 380: 314-319.
- Sublett JW, et al: Seminal plasma hypersensitivity reactions: an updated review. Mt Sinai J Med 2011; 78: 803-809.
- Sublett JW, et al: Characterization of patients with suspected seminal plasma hypersensitivity. Allergy Asthma Proc 2011; 32: 467-471.
- Weidinger S, et al: IgE-mediated allergy against human seminal plasma. Chem Immunol Allergy 2005; 88: 128-138.
- Weidinger S, et al: Prostate-specific antigen as allergen in human seminal plasma allergy. J Allergy Clin Immunol 2006; 117: 213-215.
- Yocum MW, et al: Concurrent sensitization to natural rubber latex and human seminal fluid. J Allergy Clin Immunol 1996; 98: 1135-1136.
DERMATOLOGIE PRAXIS 2018; 28(3): 23-26











