Nail diseases can be very disturbing for the patient cosmetically, but also functionally. Before deciding on therapy, it is important to determine whether the nail change is due to a past or still ongoing pathology. Important causes of dry, crumbly, deformed or discolored nails are exogenous influences, infections including nail mycoses, psoriasis, eczema and tumors.
Fingernails contribute significantly to the appearance of the hands, which is why nail diseases are particularly limiting for patients. Before the question of suitable therapy options can be raised, a diagnosis must of course first be made. In the following, nail diseases are roughly divided according to the causes: exogenous influences including infections, endogenous inflammations and tumors.
The nail shows how influences have acted over time. For example, transverse grooves (Beau-Reil furrows) are the sign of a short-term generalized growth disorder, with the grooves growing out as they progress. Longitudinal ridges or canaliculi as signs of a focal, long-lasting increase or decrease in nail growth will persist as long as the causative process in the matrix area is not treated. Thus, before deciding on treatment, one will always have to take into account whether the pathogenic factor was a short-acting, recurrent one or whether the pathology is ongoing.
Exogenous influences
Exogenous influences often result in changes in the nail plate. In onychoschisis, splitting of the distal nail plate occurs as a result of desiccation, often also due to wet work or mechanical impact. In the clarification of brittle nails, the anamnesis with questions about corresponding pathogenic influences including occupational toxins (cement, thioglycolates, solvents, acids, alkalis, anilines, salt, sugar solution) and nail cosmetics or nail cosmetic procedures is of the greatest importance, laboratory chemical examinations play a rather subordinate role. Only the determination of ferritin may be useful, especially if there is hapalonychia with soft nails or koilonychia with concavely dented nails.
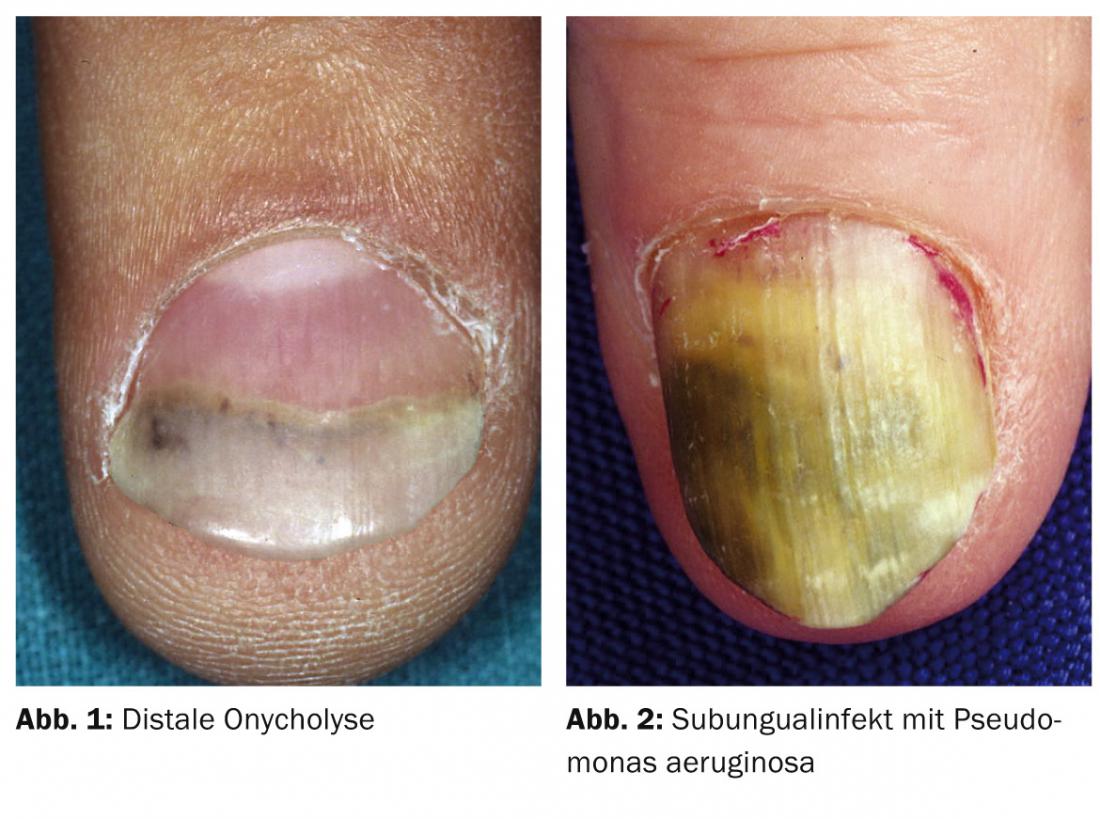
Distal onycholysis is often observed, especially with regular moist contacts (Fig. 1). This results in an inflammatory seam in the area of the hyponychium, which leads to detachment of the nail from the nail bed. The capillary action draws further moisture with dirt particles and bacteria into the resulting crevice space, perpetuating the process. The only remedy is consistent avoidance of moisture (wearing gloves) and cutting the nails short. Also caused by wet work are bacterial subungual infections (Fig. 2) and Candida paronychia. For subungual infections, the detached nail must be trimmed back to allow for careful brushing and disinfection. In Candida paronychia, in addition to systemic azole preparations, surgery with crescent-shaped ablation of the chronically infected nail wall is occasionally used. The most important measure is to avoid wet contact and repeated trauma. Since occasionally already repeated microtrauma such as work on keyboards, especially with long nails, can lead to impairment of nail growth, the nails must be shortened.
For dry, brittle nails, simple nourishing oils or creams (especially with phospholipids) are useful. The multitude of other advertised cosmetic nail care products usually lack scientific proof of efficacy.
Iron deficiency
If iron deficiency is proven, systemic iron substitution is performed. Taking biotin with food (millet) or a supplement may be helpful. In any case, the doctor and the patient must be patient enough, because changes in the nail plate and thus improvements of the same can be assessed only after the nail has grown back, i.e. after a period of 3 – 6 months.
Onychophagy
Therapy becomes more difficult if the patient causes the pathology himself, as for example in the case of onychophagia in the context of a disorder of impulse control (Fig. 3). Since this happens consciously and is usually also confirmed on demand, onychophagia is assigned to the paraartifacts. To change the behavior, the application of bitter-tasting externals may be helpful for deconditioning, e.g., with appropriate nail polishes or topical tetracyclines.

Onychomycoses
Crumbly nail dystrophy indicates onychomycosis. However, the fingernails are less frequently affected in this respect than the toenails. However, at baseline, only discrete changes may be present (Fig. 4), causing differential diagnostic difficulties. Before therapy, the detection of mycosis is mandatory.

The collection of nail material for mycological diagnosis is performed from subungual. The most sensitive method for detecting onychomycosis is histologic workup of cut nail material with PAS staining; this method may be used in unclear cases. If proven, onychomycosis must be treated systemically, with terbinafine 250 mg/day being the gold standard. Azoles are also effective or the treatment of choice for Candida infection. Therapy of onychomycosis usually lasts for several months, but it is not necessary to treat until the discolored or deformed parts of the nail grow out completely. The use of nail polishes containing amorolfine alone does not usually result in healing, but in combination with systemic therapy may reduce the recurrence rate.
Endogenous inflammation: Psoriasis, eczema, lichen ruber
Psoriasis is the most common skin disease involving nails. In this case, when the matrix is affected, dimples, leukonychia, lunular erythema and onychodystrophy are found in particular. (Fig. 5), if the nail bed is affected, especially oil spots, onycholysis, subungual keratosis and splinter hemorrhages (Fig. 6). If nail psoriasis is suspected, complete examination of the skin is essential for diagnosis, as psoriasis is isolated to the nails in only 1-5% of patients and thus further changes can be expected. At the same time, nail psoriasis may indicate psoriatic arthropathy, as up to 80% of patients with psoriatic arthropathy also have nail changes. Accordingly, early dermatologic and rheumatologic evaluation and therapy should occur.

Trachyonchia (Fig. 7) with roughening of the entire nail plate is observed in so-called “twenty-nail-dystrophy”, but also in lichen ruber planus, eczema or alopecia areata.
Inflammatory diseases of the nail are difficult to treat with local therapeutics, since the active substances can hardly be introduced into the matrix area and the nail bed. Topical steroids are primarily used, in the matrix area as a cream or ointment, and in the subungual area as a solution. In psoriasis, vitamin D analogues can also be used as monotherapy or combination therapy. Intralesional steroid injections with crystal suspension are an effective but painful therapeutic option. The application site must include both the matrix and the nail bed, according to the infestation pattern. Therefore, two injections each, performed from the side, into the matrix area and under the nail bed are usually necessary. Systemic retinoids may also be used for pronounced changes associated with eczema or lichen ruber. In psoriasis, there is the possibility of systemic therapy with TNF-alpha inhibitors, especially in the presence of psoriatic arthritis.
Tumors
Tumors are usually excised, so this is more of a diagnostic problem than a therapeutic one. First and foremost, it is important to differentiate malignant from benign changes. In this context, it is mainly melanocytic changes that repeatedly raise diagnostic questions (Fig. 8) . Subungual hematomas appear rather blue-red at the beginning, especially in the marginal area, later green. Green discoloration can also be observed in nail bed infections caused by Pseudomonas.

Newly developed melanonychia strata in adults always requires clarification, especially if it is wider than 5 mm and proximally wider than distally (i.e., growing), encroaches on the nail wall (Hutchinson’s sign), or the nail becomes dystrophic.
Tumors under the nail plate also change the shape of the nail as they progress. Processes located above the matrix lead to an impression of the nail plate due to pressure, while an upturned nail plate indicates a subungual tumor. Malignant processes such as Bowen’s disease or malignant melanoma can lead to changes in the nail plate up to complete destruction (Fig. 9).

If a biopsy is necessary, it can be performed in the nail bed area by punching through the nail with removal of a smaller punch from the nail bed. The resulting defect in the nail plate grows out. In the matrix area, a punch biopsy up to a maximum diameter of 3 mm is also possible without provoking a permanently split nail.
Melanomas in the nail area do not have a worse prognosis than melanomas of comparable thickness in other locations. However, the delay in diagnosis is on average two years. For in situ or minimally invasive melanomas, excision of the nail unit with an appropriate safety margin followed by coverage with a full-thickness skin graft may be sufficient without worsening the prognosis. Amputation is not mandatory in such a situation. Preservation of the beam can be of fundamental importance to the patient, especially on the thumb and even more so on the leading hand.
Further reading:
- Dehesa L, Tosti A: Treatment of inflammatory nail disorders. Dermatol Ther 2012; 25: 525-534.
- Tan ES, Chong WS, Tey HL: Nail psoriasis: a review. Am J Clin Dermatol 2012; 13: 375-388.
- Radtke Ma, Beikert FC, Augustin M: Nail psoriasis – a therapeutic challenge in clinic and practice. JDDG 2013; 11: 203-221.
- Nenoff P, Paasch U, Handrich W: Infections of finger and toe nails caused by fungi and bacteria. Dermatologist 2014; 65: 337-348.
- Löser C, Mayser PA: Dark nail. Clinic, diagnosis and therapy of melanonychia. Dermatologist 2014; 65: 327-336.
- Haneke E: Malignant tumors of the nail organ. Dermatologist 2014; 65: 312-320.
CONCLUSION FOR PRACTICE
- In the clarification of brittle nails, the anamnesis with questions about pathogenic influences is in the foreground.
- Crumbly nail dystrophy indicates onychomycosis. Before therapy, the detection of mycosis is mandatory.
- Psoriasis is the most common skin disease affecting nails. In affected patients, dermatological and rheumatological clarification and therapy should take place at an early stage.
- Dark, stripe-like discolorations of the nails (melanonychia strata) are always worthy of clarification, as malignant melanoma is suspected.
DERMATOLOGIE PRAXIS 2014; 24(6): 12-15











