In the evaluation of knee injuries, the next step after the clinical examination is the conventional X-ray in two planes. The aim is to detect any osseous lesions. Indications for MRI include hemarthrosis (acute effusion following trauma), clinical and subjective instability, and joint block. An MRI should then be performed as soon as possible. By no means every knee injury requires surgical treatment. Conservative therapy should be carried out with further controls and usually physiotherapeutic treatment. The goal of any reconstructive knee procedure is a stable, pain-free knee. Regular exercise and normal weight are the most important prognostic factors in the medium term to slow the development of gonarthrosis after a knee injury.
Acute injuries of the knee joint are among the most common clinical pictures in everyday sports traumatology. It is not always easy to make a correct and complete diagnosis initially. Patients are typically physically active and in mid-career. A possible loss of work and a long break from sport therefore meet with little acceptance. The goal should therefore be a rapid and streamlined diagnosis in order to guide the patient to effective therapy.
In recent years, the understanding of some injuries has changed, and so have treatment options. In addition, new methods are entering the market and some critical literature has been published. The purpose of this article is to provide guidance to the practitioner in the evaluation of acute knee injuries and to critically assess therapeutic options – to increase confidence in the evaluation and initiation of therapy for acute knee injuries.
Medical history
As always, everything starts with the anamnesis. The accident mechanism provides important clues to the pattern of injury. Most anterior cruciate ligament injuries occur without opponent contact and almost always involve a rotational component. In most cases, patients experience acute instability and also perceive the tear acoustically. Persistent instabilities are frequently described, especially when walking down stairs. In turn, posterior cruciate ligament injuries happen either by direct force on the tibial plateau when the knee is flexed or by hyperextension. Isolated ligament injuries often cause little initial discomfort, but over a few hours the leading symptom of hemarthrosis develops. Acute persistent or recurrent limitations of mobility are indicative of an unstable meniscus (basket handle tear) or cartilage injury. Any previous operations complement the medical history and provide important information.
Clinical examination
The patient’s gait pattern can be assessed as soon as he enters the consulting room; the restricted extension is particularly noticeable. The examination should always be performed on the unclothed leg and in lateral comparison. An acute effusion due to the leading symptom of hemarthrosis is usually already well visible through the obliterated joint contours. An injury to the cruciate ligaments is often not easy to recognize acutely. It is important that the patient’s muscular tone does not compete with the examination. The patient should be placed in a stable and relaxed position and it is recommended to distract him. Drawer tests and pivot test are poor to test in acute condition. For the anterior cruciate ligament, the Lachmann test is recommended, which can also be actively performed by quadriceps tensioning. In the case of a rupture of the posterior cruciate ligament, in addition to typical pretibial bruise marks, the head of the tibia can be seen to fall back due to gravity when the thigh is inferiorly positioned, which can also be found in a lateral comparison in acute injuries (Fig. 1).

Meniscal injuries in acute cases are usually apparent by a pressure dolence over the joint spaces and are thus to be differentiated from injuries of the collateral ligaments, which usually hurt over the osseous attachments. Classic meniscus tests such as Steinmann and Payr are also difficult to differentiate acutely. Alternatively, if the patient can bear weight, the Thessaly test can be used: The patient stands on the injured limb with slight flexion and is rotated by the examiner.
The collateral ligaments are to be tested in lateral comparison, in full extension and at 20-30° flexion. First-degree injuries are only painful, second-degree injuries are increasingly hinged in flexion, and third-degree injuries are also hinged in full extension – in this case, the central pillar is usually also affected and the knee is rotationally unstable. Ligament injuries can be clinically quantified as + (up to 5 mm), ++ (5-10 mm), and +++ (greater than 10 mm). After patellar dislocation, acute clinical signs include pressure dolence over the medial retinaculum with apprehension and pressure dolence over the lateral femoral condyle [1].
Further clarifications
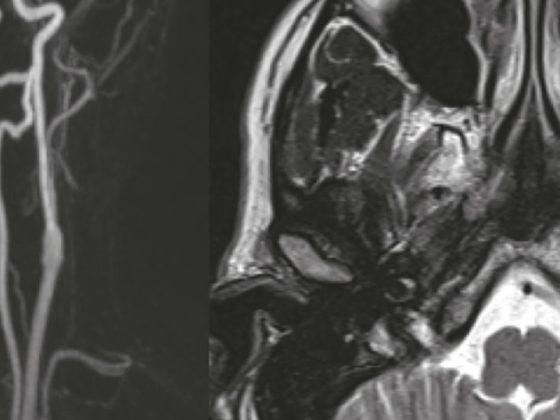
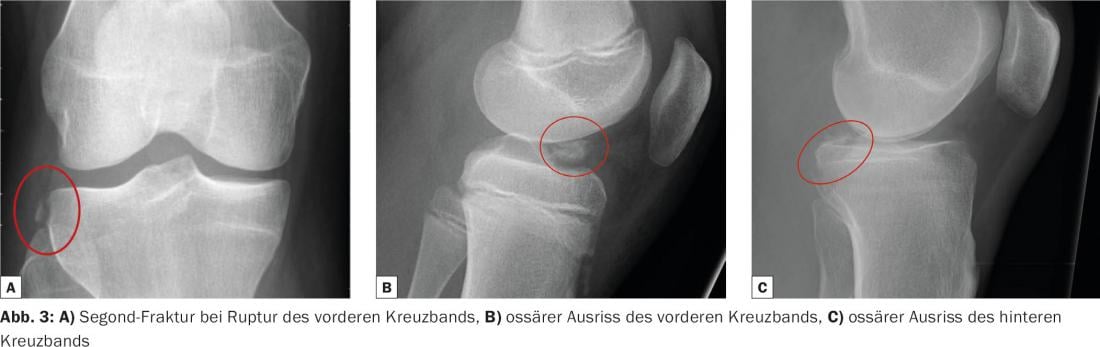
As imaging, conventional X-ray in two planes is the next step. The aim here is to detect any osseous lesions. Liphemarthrosis, which appears as a mirror in the lateral images, is an indirect indication of a significant osseous injury and should be further clarified by CT (Fig. 2). Osseous avulsion of the anterior and posterior cruciate ligaments and osseous capsular avulsion such as the Segond fracture are also important clues (Fig. 3).

MRI is considered the gold standard for evaluating internal knee lesions. Primary indications are hemarthrosis (acute effusion after trauma), clinical and subjective instabilities, and joint blocks. A contrast agent is not necessary. We recommend that this examination be performed quickly in cases of clinical suspicion, since a corresponding correlate can be shown on MRI in up to 100% of cases with appropriate clinical indications. Frequently, there are additional concomitant injuries that require prompt reconstructive procedures [2].
Primary treatment
The PECH scheme has proven successful: rest, ice (cooling), compression (e.g. Voltaren bandage), elevation. Walking sticks are more helpful than a bandage in restoring the ability to walk. Orthoses are only useful in cases of higher-grade instability. Prolonged immobilization should be avoided. Even without a specific diagnosis, physiotherapeutic measures to relieve congestion, reduce effusion and maintain range of motion are useful. This is achieved with a lot of exercise and little stress. If loading is not possible, thromboembolism prophylaxis with a low molecular weight heparin is indicated. NSAIDs are commonly used for pain management.
By no means every knee injury requires surgical treatment. However, conservative therapy should be performed with further controls and usually physiotherapeutic exercise.
Injuries of the anterior cruciate ligament
In acute knee injuries with hemarthrosis, the anterior cruciate ligament (ACL) is involved in more than two thirds (depending on the collective). Conservative treatment is possible in so-called adapters and copers: a part of those successfully treated conservatively avoids a corresponding strain by adjusting their lifestyle (adapters) and a small part returns to a good function with similar strains (copers). Unfortunately, there are no reliable predictors of successful conservative therapy. Good indications for a conservative therapy trial are isolated cruciate ligament injuries in less demanding injured patients.
Patients with combined injuries and high demands, especially children, have worse cards. Meniscal injuries that can be reconstructed in particular should be addressed early and require a ligament-stable knee to heal. Rotationally unstable knees, i.e., with higher grade collateral ligament instabilities, also frequently do not heal adequately with conservative therapy and should be operated on within the first 14 days.
The again propagated cruciate ligament sutures (Ligamys, Internal Brace) are currently not paid by the insurers due to the insufficient literature in Switzerland. However, the dynamic Ligamys system in particular has shown promising results so far. The operation must then be performed as early as possible, certainly within the first 14 days. The standard procedure is currently arthroscopically assisted, single-bundle arthroplasty using an anatomic technique with a semitendinosus tendon [3]. We place a high value on preserving as much original tissue as possible because this helps to reduce the rerupture rate [4].
Follow-up treatment (after conservative or surgical treatment) is carried out on walking sticks until a safe gait is achieved. This requires good control of the quadriceps and training accordingly. Relief or splint treatment is not necessary. There is no consensus regarding post-treatment – it is recommended to perform it gradually until the return to athletic exertion. As soon as range of motion allows, ergometer training/velo, crawl or backstroke can be started. Running training is possible as soon as the knee is free of effusion. The practice of knee-loading sports (with rackets, balls, boards and opponents) will be released at the earliest after six months with an irritation-free, stable knee and successful functional testing. Most amateur athletes, however, need rather nine months until they are physiologically ready – psychologically, there are often blockages for even longer.
Injuries of the posterior cruciate ligament
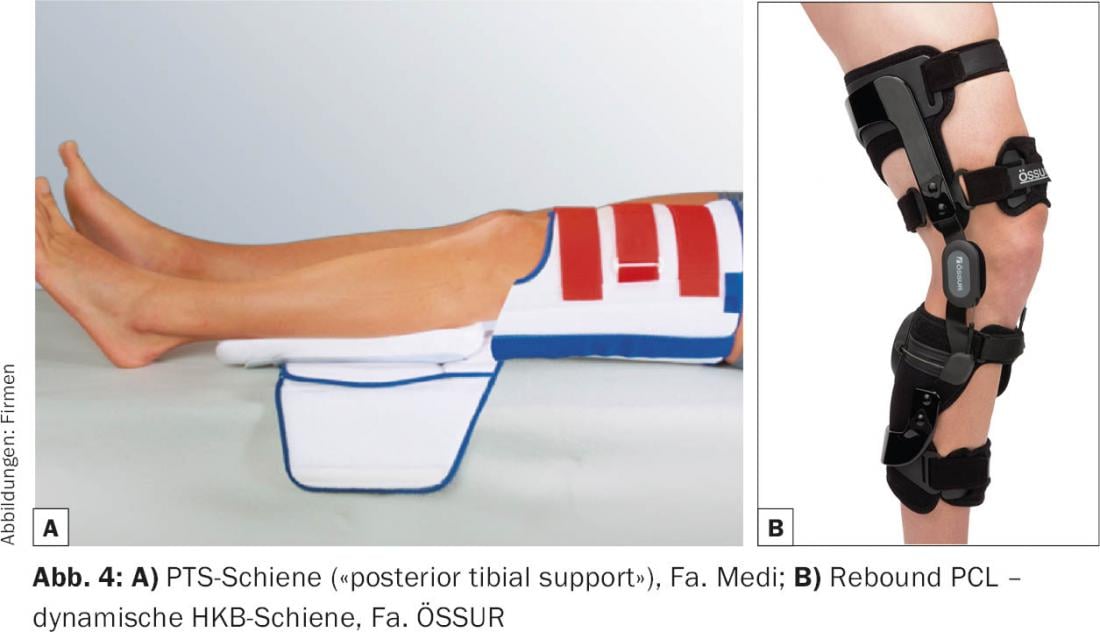
Injuries to the posterior cruciate ligament (ACL), which is the most stable ligament in the knee, are less common and easily overlooked. Often the history is typical with a fall on the flexed knee or hyperextension. Clinical findings are usually much more discrete, and even MRI can be deceiving. Clinically, a bruise mark over the tibial tuberosity or a hematoma in the popliteal fossa is often seen. In lateral comparison, it is visible that with the knee bent, the tibia sags slightly backwards or, respectively. the a.p. translation is increased in the side comparison, where it can be difficult to distinguish between anterior and posterior drawer. Typical concomitant injuries are posterolateral corner injuries, look for them. Functional images under stress in lateral comparison (telos) are evidence of BUA injuries. Conservative therapy of fresh (>14 days), isolated ACL injuries is usually successful because of the pronounced synovial covering, but needs very good compliance and an experienced physiotherapist. The goal is to abolish posterior translation by gravity and avoid hamstrings activity. This is achieved with special splints (PTS Brace, Medi) or dynamically with special orthoses (PCL Jack Brace, Albrecht; Rebound PCL, Össur) (Fig. 4). These must be worn consistently for three months, usually initially for six weeks statically. The physiotherapeutic exercise is initially performed strictly in the prone position. As with any knee injury, it is important to have very good quadriceps control, which should be trained at least isometrically from the beginning. As soon as full control of the extensor apparatus is established, increasing loads may also be applied.
Persistent symptomatic instabilities and also combined injuries (meniscus, posterolateral corner) should be treated surgically, today mostly in the form of a replacement plasty using autologous hamstring grafts. Follow-up treatment is carefully analogous to conservative therapy. Unfortunately, the results are more disappointing than after ACL replacements because the grafts often loosen [5].
Injuries of the collateral ligaments
Isolated collateral ligament injuries are rare. Low-grade injuries can be treated conservatively with functional therapy. In principle, lateral collateral ligament injuries heal worse than medial ones, and avulsion injuries in particular lend themselves to surgical treatment. Grade II injuries (increased opening in 20-30° flexion in a lateral comparison) should be clarified by MRI, but can usually be treated with a soft orthosis for six weeks and physiotherapy. For grade III injuries, a surgical indication must be evaluated; if necessary, these injuries can also be treated in a hard frame orthosis, at least medial injuries without avulsion or stener lesion (overturned stump). In the acute phase, refixation is often possible, while secondary procedures generally require reconstruction with a tendon graft. Post-treatment is performed by means of an orthosis for six weeks under partial weight bearing on walking sticks to protect the grafts.
Meniscus injuries
The treatment of meniscal lesions has been the focus of criticism in recent years [6]. However, there is consensus that an acutely injured meniscus should be preserved to delay the onset of osteoarthritis. Meniscus injuries often occur in combination with cruciate ligament injuries. The best results are expected in the young patient with acutely treated meniscal lesion. Today, meniscal injuries are sutured arthroscopically and often with special suture systems. Since menisci are composed of bradytrophic tissue, safe healing cannot be taken for granted. Various surgical-technical approaches (e.g. microfracturing) help to optimize the biological conditions for healing somewhat. Meniscus replacement using allograft or partial replacement using artificial menisci is currently not researched enough to be widely applied. Meniscus replacement, however, can be successful for chronic conditions.
Post-treatment depends on crack shape, localization and suture technique. In most cases, partial loading and some restriction of range of motion occur. Stress forces on the suture should be avoided at all costs, so we prohibit loaded flexion (deep squat) for three months. Conservative treatment – which is the initial therapy for degenerative damage – includes exercise (physiotherapy), analgesia using NSAIDs, and, if necessary, nutritional supplementation with chondroitin and glucosamine. As shown in studies, the conservative approach is not always successful, especially patients with blockage symptoms and nocturnal entrapment often benefit from a surgical approach. However, one cannot expect a positive influence on osteoarthritis, which by definition is progressive.
Cartilage injuries
We see acute cartilage injuries most often after patellar dislocations and cruciate ligament tears. Purely cartilaginous injuries can only be detected on MRI. If the injuries are in the stress zone, it is recommended that the cartilage be refixed promptly, since cartilage-stimulating measures and even cartilage transplants do not produce tissue of equivalent quality. Depending on the location, the refixation is usually performed via a small arthrotomy. Follow-up treatment depends on the localization and usually consists of a gradual build-up of range of motion under partial weight-bearing for six weeks [7]. Supplementation with chondroitin and glucosamine is also possible.
Patellar luxation
Adolescents in particular suffer this injury with an uncontrolled twisting motion and an almost completely extended leg, usually without contact with an opponent. Often reduction occurs spontaneously, otherwise stretching the knee joint is sufficient for reduction. Luxations of the patella are favored by specific anatomical conditions. In most cases, the abutment to the patella on the lateral femoral condyle is only slightly pronounced due to hypoplasia of the medial condyle (trochlear dysplasia). Other predisposing factors include relative elevation of the patella and axial or rotational deviations. Neuromuscular deficits, together with instability of the leg axes, favor the tendency to deviate into functional valgus and thus to dislocate.
For clarification, the most perfect possible knee images laterally, ap and patella tangentially are required for the initial dislocation. An MRI should be performed to rule out a cartilage lesion at the medial patellar facet or lateral femoral condyle, which is common after all. In the case of loose cartilage components, primary surgery for cartilage refixation is indicated. A first-time dislocation without a cartilage lesion can be treated conservatively. It is recommended to use walking sticks until gait stability and good quadriceps control are achieved. The effect of bandages has not been proven, but patients often find them comfortable; taping is an alternative. Physiotherapeutic training to stabilize the leg axes and prevent functional valgus is often sufficient, but it is not possible to stabilize the patella purely muscularly. Depending on the severity of the accompanying anatomic circumstances and the patient’s claim, reluxations are unfortunately not uncommon [8].
A newer surgical reconstructive procedure is soft tissue reconstruction of the major extensor static stabilizer of the medial patellofemoral ligament. Bony measures such as trochleaplasty, tuberosity distalization, or osteotomies may be necessary in addition. Measures such as lateral release (increases instability) or tuberosity medialization (increases pressure in the patellofemoral joint) are becoming less important [9].
Forecast
Most knee injuries result in varying degrees of articular cartilage affection, increasing the risk for gonarthrosis. The development of osteoarthritis is triggered by the initial trauma [10]. Reconstructive surgery of the knee can restore anatomy, preventing secondary damage that accelerates the path to osteoarthritis. A stable, pain-free knee is the goal of any reconstructive knee procedure. Good function maintains quality of life and, at best, sports ability.
Not every patient comes back to sports. After anterior cruciate ligament injuries, only a good 80% of patients return to sports, and only about 50% achieve the same level of performance. The reasons for this are multifactorial and, in addition to the quality of care and follow-up, also depend significantly on psychosocial factors [11]. Regular exercise and normal weight are the most important prognostic factors for slowing down osteoarthritis in the medium term.
Literature:
- Zacher J: Clinical examination of the knee joint. Orthop Trauma Chir up2date 2006.
- Abbasi D, et al: MRI findings in adolescent patients with acute traumatic knee hemarthrosis. J Pediatr Orthop 2012; 32(8): 760-764.
- Petersen W, et al: The anatomic replacement anterior cruciate ligament in single bundle technique. Oper Orthop Traumatol 2013; 25(2): 185-204.
- Takazawa Y, et al: ACL Reconstruction Preserving the ACL Remnant Achieves Good Clinical Outcomes and Can Reduce Subsequent Graft Rupture. Orthopaedic Journal of Sports Medicine 2013; 1(4): 2325967113505076.
- LaPrade CM, et al: Emerging Updates on the Posterior Cruciate Ligament: A Review of the Current Literature. Am J Sports Med 2015 [Epub ahead of print].
- Mordecai SC, et al: Treatment of meniscal tears: An evidence based approach. World J Orthop 2014; 5(3): 233-241.
- Kühle J, et al: Osteochondral fractures of the knee joint. Trauma Surgeon 2015; 118(7): 621-634.
- Balcarek P, et al: Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 2014; 22(10): 2308-2314
- Schmeling A: Current aspects of patellofemoral instability. SFA Arthroscopy Aktuell 23 2010; 23.
- Simon D, et al: The Relationship between Anterior Cruciate Ligament Injury and Osteoarthritis of the Knee. Adv Orthop 2015; 2015: 928301.
- Ardern CL, et al: Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014; 48(21): 1543-1552.
HAUSARZT PRAXIS 2015; 10(9): 21-26