The choice of therapeutic modalities for lung cancer depends on several factors. Accurate staging, assessment of operability, and knowledge of prognostic factors such as the number of affected lymph node stations and grading are critical. Standard treatment for early stages is primary surgery. For patients in advanced but still operable stages, neoadjuvant chemotherapy may improve resectability. To increase lung cancer survival rates, screening programs should be implemented in at-risk individuals.
Lung cancer remains a cancer with a very high mortality rate, with a current 5-year survival rate of 15.1%. Despite massive use of resources and improvement of all available therapeutic modalities – including state-of-the-art antibody therapies – mortality has remained unchanged for 30 years [1]. The reason for this unsatisfactory development is the fact that lung cancer is usually diagnosed only when the disease is already at an advanced stage.
Lung cancer could well be curable, especially thanks to surgical treatment options, but at diagnosis 75% of affected patients are already beyond curative treatment. This unfavorable starting position will only improve for patients if consistent screening of the risk group with low-dose CT were to be performed according to a precisely defined algorithm and if this screening were also paid for by the health insurance funds. Then, as has been impressively documented scientifically [2], the prognosis could indeed be improved, and the mortality from lung cancer would decrease continuously and significantly. The role of surgery will undergo a transformation as screening programs hopefully emerge, and minimally invasive surgical methods and limited resections will increase accordingly [3].
Staging
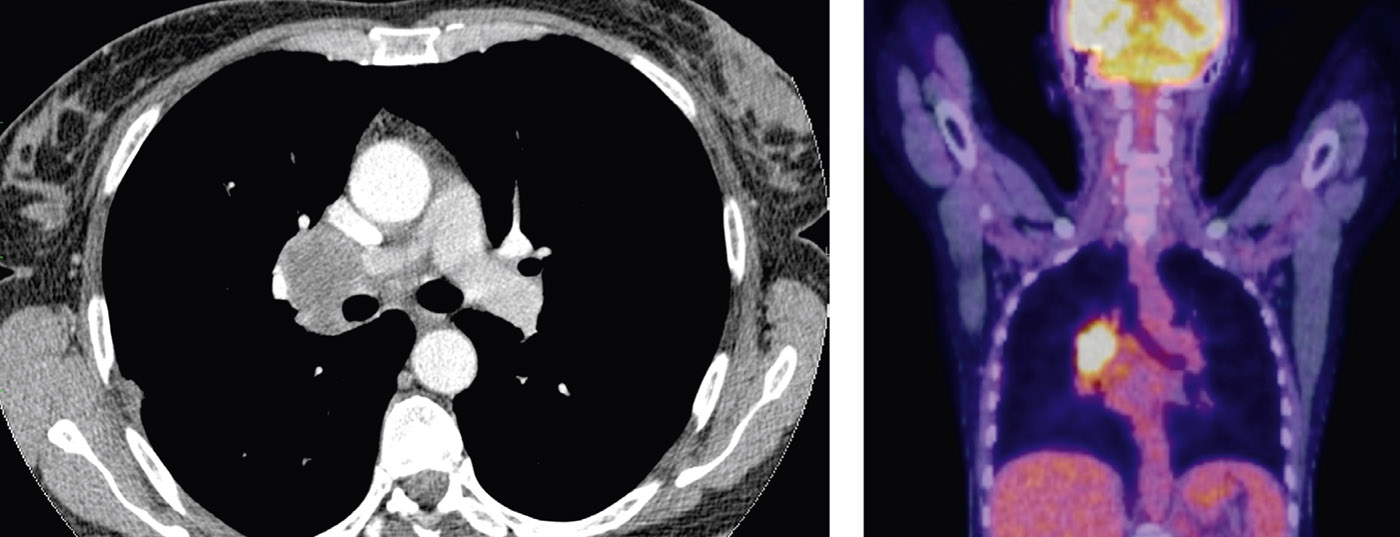
The staging of non-small cell lung cancer (NSCLC) is based on the TNM classification and AJCC clinical staging [4]. Staging follows staging and is very relevant for the selection of therapeutic modalities at the obligatory discussion in the interdisciplinary tumor board. Proper NSCLC staging includes bronchoscopy with biopsy, as well as CT and PET scanning. The determination of the exact lymph node stage (N stage) is very relevant for surgical therapy planning. PET carries great weight here, as it provides very reliable results in terms of negative predictive value (NPV). However, PET-positive lymph nodes in the mediastinum must always be documented histologically (e.g., with endobronchial ultrasound, transbronchial biopsy, or mediastinoscopy), because PET is insufficient with regard to positive predictive value (PPV). This also applies to the primary tumor site in the lung parenchyma. If no transbronchial histology or at least flush cytology documents malignancy, transthoracic puncture or thoracoscopic wedge resection is recommended for completion of staging [5–7].
Operability
The majority of patients with NSCLC are active or former smokers with associated pulmonary and cardiac comorbidity (COPD, emphysema, etc.). A so-called functional staging is therefore an important component prior to the indication for surgical intervention. The key investigations for this are pulmonary function tests, ergometry and, in critical cases, spiroergometry in combination with perfusion scintigraphy. It is recommended that the ESMO guidelines be followed in this regard [8]. For practical purposes, a good guide is still the FEV1, which should be a minimum of about 1 liter after surgery.
Prognostic factors for indication
The planning of a surgical intervention in NSCLC is very complex due to the wide range of tumor appearance and requires detailed knowledge. There are clear methodological rules for the indication and the aim is to provide the patient with the most tailored or appropriate treatment. offer individualized surgical therapy. While for early stages (T1-2, N0, M0, or AJCC IA-IB) the focus is on parenchyma-sparing, minimally invasive treatment approaches including staging lymphadenectomy, for advanced stages that can still be treated surgically (T1-4, N1-2, M0, or AJCC IIA-IIIB) the focus is on optimizing multimodality oncologic, radiotherapeutic, and surgical therapies. The surgeon must have a detailed knowledge of the important prognostic factors and be able to adjust therapy even intraoperatively, by using rapid histopathologic diagnostics as frequently as possible. Based on current knowledge, the following factors are independent prognostic factors for surgical treatment of NSCLC, weighted by importance [9–12]:
- Number of affected lymph node stations
- Grading and histological differentiation
- Lymphangioinvasion in definitive histology
- Total number of affected lymph nodes
- Response to neoadjuvant therapy
- Sex and age of the patient
- Tumor size
Surgical therapy of the early stages
Tumors of stages T1-T2 without lymph node involvement are referred to as early stages and have a correspondingly good prognosis (Fig. 1) .
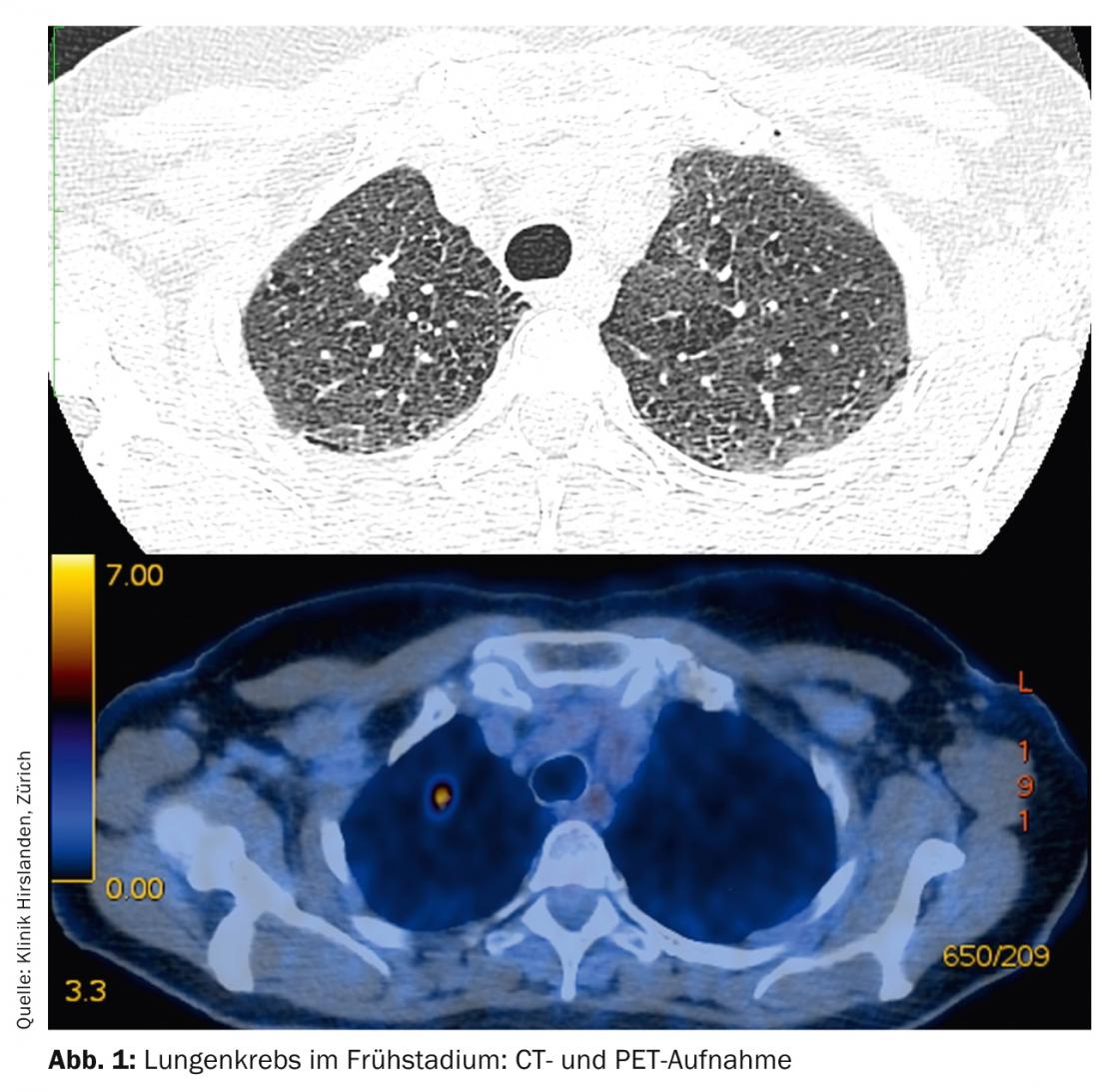
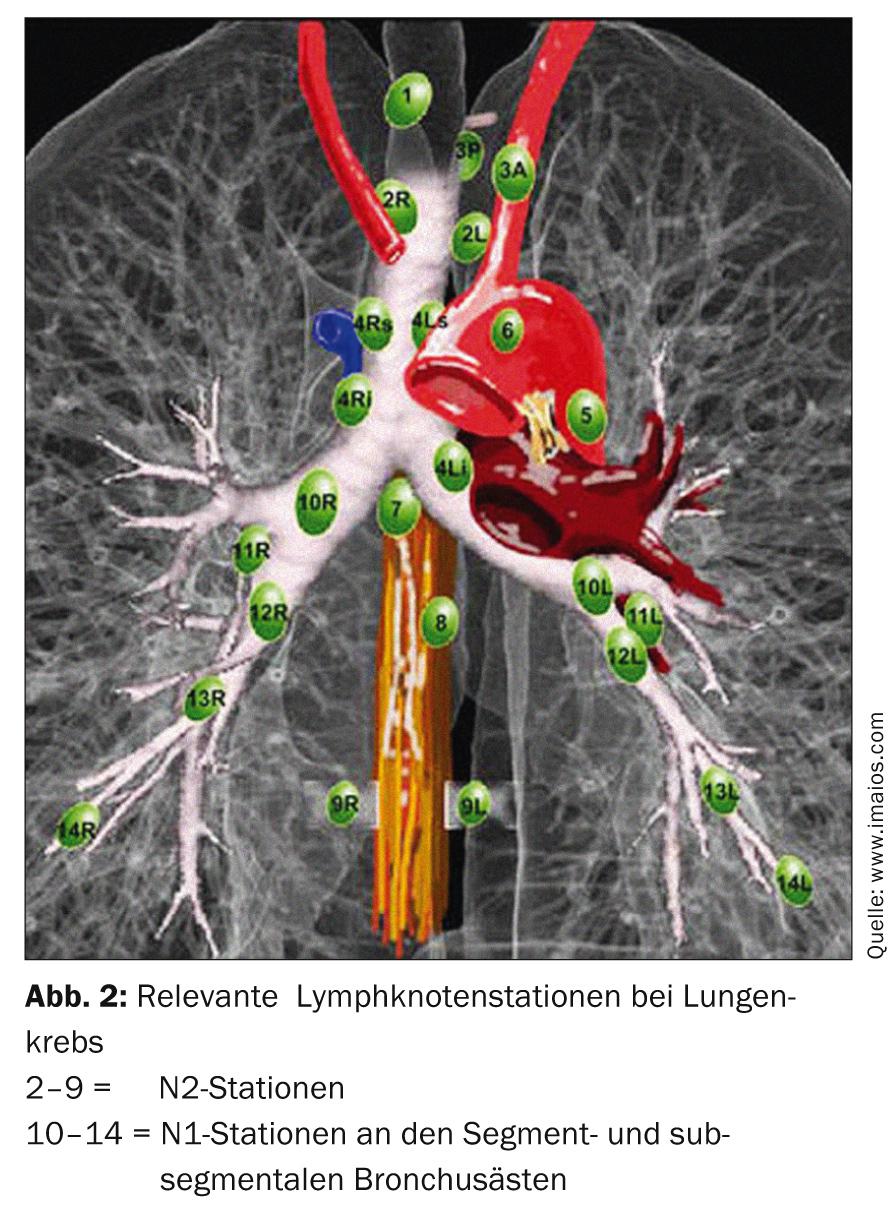
The standard treatment is primary surgical therapy. Depending on the location of the tumor in the lung lobe, either segmental resection or lobectomy may be necessary. Verification of the N0 stage by systematic sampling of the lymph nodes in the mediastinum is obligatory (Fig. 2). In case of intraoperative change of stage (surprising N1 or N2 involvement), immediate adjustment of surgical therapy with radical lymphadenectomy and completion lobectomy is necessary. The age and performance status of the patient must also be included in this decision as essential criteria. If a patient has undergone segment resection and is found postoperatively to have many prognostic risk factors (lymphangioinvasion, subsegmental lymph node involvement, poor grading, male adenocarcinoma, etc.), a completion lobectomy in the sense of a second procedure is necessary and additive chemotherapy should be discussed in the tumor board [13].
Surgical therapy of advanced stages
All T stages with N1 or N2 involvement are advanced but still operable stages (IIA-IIIB). In this group of patients, very different morphologies are present, and surgical treatment planning is correspondingly complex. There are two critical issues for setting the course for available therapeutic approaches:
- Is there a large tumor bulk or lymph node bulk centrally resp. Near the main bronchus division or near other mediastinal organs (aorta, heart)?
- Are multiple N2 lymph node stations affected? And if so, which ones in relation to the tumor-affected lobe?
If one of these questions must be answered “yes,” the question of neoadjuvant pretreatment arises. If both questions can be answered in the negative, the patient is treated primarily with surgery. The goal of neoadjuvant pretreatment is to improve resectability and elicit patients with an intact prognosis. After usually three cycles of chemotherapy (e.g., with cisplatin and docetaxel), restaging is performed. If the response is good, surgery is the next step. In the absence of response or even disease progression, the patient does not qualify for surgical therapy; he will continue to receive chemotherapy or radiotherapy with palliative intent [14,15].
Case report 1: Stage IIIA, non-extended (non-bulky), T3 N1
In the affected patient, imaging reveals an adenocarcinoma originating from the lingula with N1 lymph node involvement and two tumors in the lobe (T3) (Fig. 3).

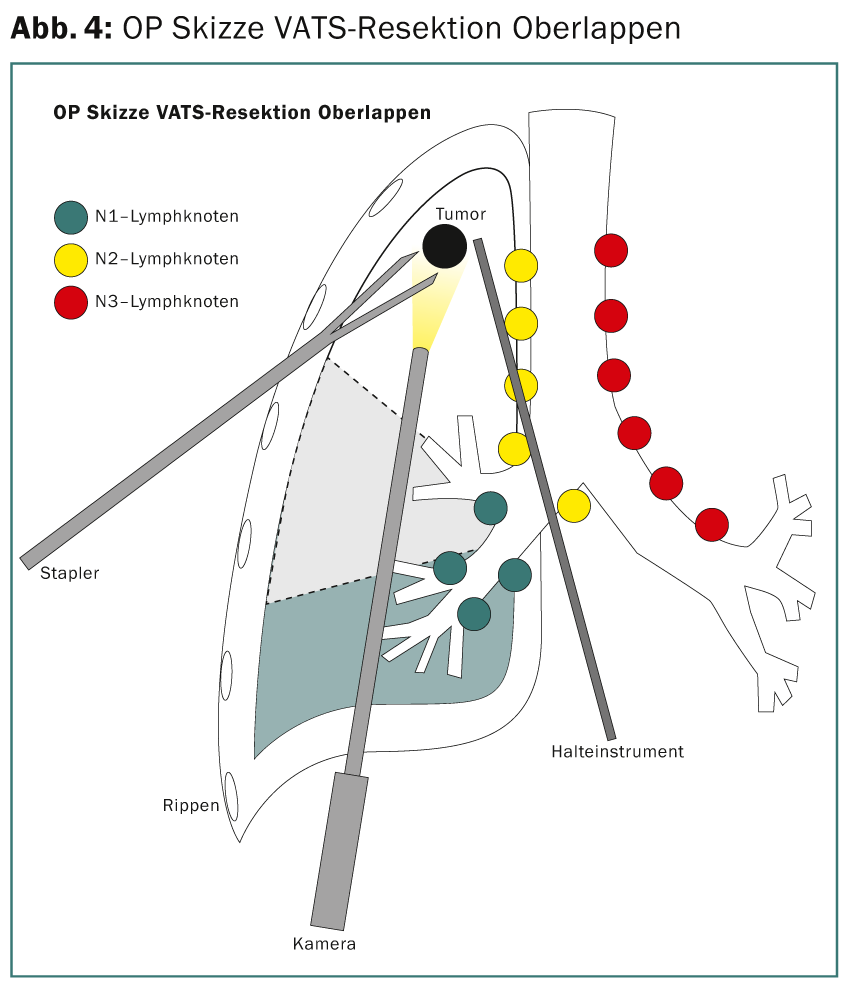
Preoperative staging with PET and endobrachial ultrasound (EBUS) of the N2 stations reveals no tumor evidence. Thus, the patient qualifies for direct surgical therapy. A thoracoscopic upper lobectomy (minimally invasive VATS lobectomy [VATS thoracic surgery]) (Fig. 4) with extensive mediastinal lymphadenectomy is performed. Intraoperatively, R0 resection is confirmed by rapid histopathologic diagnosis of the resection margins and N2 lymph nodes. The definitive tumor stage TNM of pathology is pT3, pN1 (3 of 34), L1, V1, Pn0, R0. Adjuvant chemotherapy is recommended due to the lymph node situation.
Case report 2: Stage IIIA, extended (bulky), T2 N2
Imaging reveals adenocarcinoma originating in the right upper lobe with N2 group 4R lymph node involvement (Fig. 5).
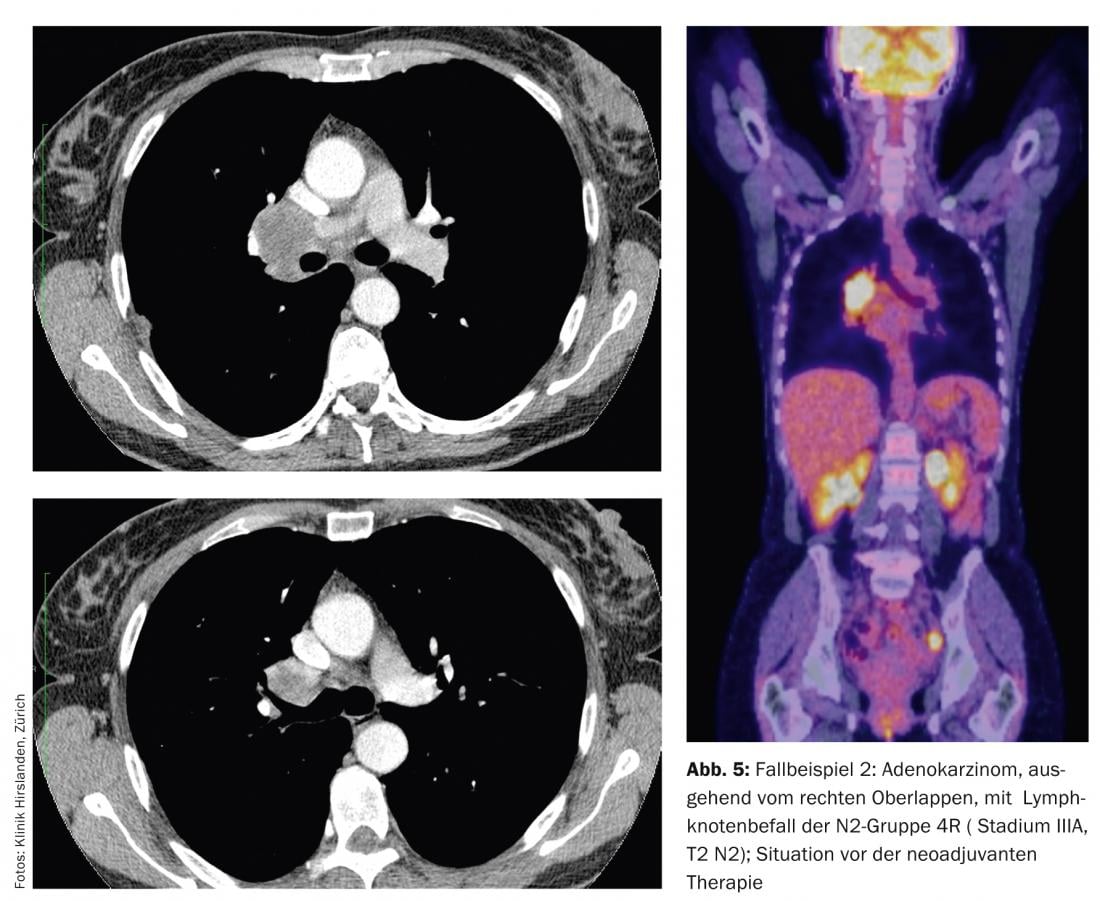
This infestation is very voluminous and extends to or beyond the main carina. Primary radical surgery cannot be performed in this area. The primary tumor is not bulky and is T2 stage at approximately 5 cm. Preoperative staging with PET and EBUS of N2 stations reveals no tumor evidence in other N2 or contralateral N3 stations. Nevertheless, this patient is a candidate for neoadjuvant pretreatment to reduce the extensive findings and select the patient for surgery. After three cycles of chemotherapy, repeat CT shows a very good response (down staging) and no new tumor manifestation in terms of new lymph node enlargements, round foci, or metastases (Fig. 6) .

Thus, the patient now qualifies for secondary surgical therapy. Open upper lobe resection with en bloc resection of the main bronchus and bronchoplastic reconstruction (Fig. 7) results in R0 resection with intraoperative confirmation by rapid histopathologic diagnosis of the incision margins and radically cleared mediastinal lymph nodes. The definitive tumor stage TNM of pathology is ypT1a, ypN0 (0 of 29), L0, V0, Pn0, R0 (“y” indicates stage after neoadjuvant pretreatment). Because of the primarily very extensive peribronchial extension, consolidative irradiation of the mediastinum is recommended in this case to complete the multimodal therapy concept.

Prospects
The treatment of advanced stages of NSCLC is an interdisciplinary and surgically technical challenge. The average 5-year survival prognosis ranges from 23% to a maximum of 55% in affected patients. The probability of survival is really good for early-stage tumors. The International early lung cancer action program (IELCAP) cohort shows survival curves for screened patients with early stages of more than 90% (10-year survival!). Currently, the overall prognosis for lung cancer is only 15.1% 5-year survival for all stages, incl. inoperable. All efforts to improve this number must be focused on improved prevention in young people and on consistent screening in high-risk groups (active or former smokers, age 50+, more than 20 pack-years). Then, today’s poor situation with only just 15.1% 5-year survival can be significantly improved.
Take-home-messages
- Only a quarter of patients with lung cancer can be given surgical therapy and thus a potential cure.
- Screening of the at-risk group is needed to detect the early stages; a screening program with low-dose CT screening significantly reduces mortality.
- The at-risk group is active or former smokers over 50 years of age with more than 20 pack-years.
- Profound knowledge of individual and general prognostic factors determines the tailored therapy concept, especially for cases requiring surgical treatment.
Prof. Dr. med. Othmar Schöb
Literature:
- Ferlay J, et al: Eur J of Cancer 2013; 49: 1374-1403.
- The national lung screening trial research team: Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med 2011; 365: 395-409.
- Altorki NK, et al: J Thor Cardiovasc Surg 2014; 147(2): 754-764.
- American Joint Committee on cancer. 7th Edition.
- Sahiner I, et al: Quant Imaging Med Surg 2014; 4(3): 195-206.
- Shingyoji M, et al: Ann Thorac Surg 2014, Aug 19. pii: S0003-4975(14)01277-6. doi: 10.1016/j.athoracsur.2014. 05.078. [Epub ahead of print].
- Teran MD, et al: J Thorac Dis 2014; 6(3): 230-236.
- Vansteenkiste J, et al: Ann Onc 2014; 25: 1462-1474.
- Riquet M, et al: Ann Thorac Surg 2014; 98: 224-231.
- Ichinose J, et al: Chest 2014; 146;(3); 644-649.
- Kuo SW, et al: J Thorac Cardiovesc Surg 2014; 148(4): 1200-1207.
- Ito M, et al: Lungcan 2014; 85: 270-275.
- Mediratta N, et al: Cardio-Thoracic Surgery 2014; 46: 267-273.
- Jaklitsch MT, et al: J Surg Oncol 2006: 94(7): 599-606.
- Trodella L, et al: Ann Oncol 2014; 15: 389-398.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(1): 13-17.