Cardiovascular diseases remain the leading causes of illness and death in Switzerland as well. In turn, atherosclerosis is the most important cause of these diseases. It begins in adolescence or earlier and develops slowly throughout life. At the doctors’ training course in Davos in winter, there was news on prevention. Furthermore, a workshop went into more detail about the depressed patient in the family practice. “Always a case for an antidepressant?” was the suggestive question here.
“Already Rudolf Virchow defined arteriosclerosis as a chronic inflammation induced by cholesterol – this still holds true after more than 100 years” says Prof. Thomas F. Lüscher, MD, Clinic Director Cardiology, UniversitySpital Zurich. “Today’s research in this regard focuses mainly on cholesterol, i.e. LDL and HDL. This is not surprising, since humans are the only ‘animal’ in evolution to have very high LDL levels, and the only species to die of heart attacks. Correspondingly, atherosclerosis is a typical disease of humans and is already detectable in 5000-year-old mummies.”
What risk factors contribute to this circumstance? In addition to blood pressure, LDL cholesterol and diabetes, genetics and age play a central role. A novel cardiovascular risk factor is the intestinal microbiome metabolite TMAO. The microbiome is determined, among other things, by breast milk. With increased plasma TMAO levels, the risk of death (by 81% at seven years) and adverse major adverse cardiac events (MACE, by a factor of 6 at 30 days) increases in patients with acute coronary syndrome (ACS) [1]. Consequently, it is a prognostic marker.
Cardiovascular factors increase with age, and so do the incidences of corresponding diseases, but not all people age the same. An interesting cohort study on the topic comes from Christoffersen M et al. [2]: Independent of other well-established risk factors and chronologic age, the following three signs of aging, alone or in combination, were associated with increased risk of ischemic heart disease and myocardial infarction:
- Androgenetic alopecia
- (“receding hairline” and circular baldness)
- Diagonal earlobe fold
- Xanthelasma
- Arcus senilis.
The risk increased gradually as the number of such signs of aging increased.
Therapeutic options and innovations
“With regard to cholesterol and atherosclerosis, the lower the better. Statins lower both LDL cholesterol and circulatory risk in a dose-dependent manner. The dose must be adjusted to the risk,” the expert explained. “A good 85% of cholesterol is formed in the liver and only a small fraction is absorbed, so dietary measures have little effect.” Statins allow LDL lowering of about 20-55%. IMPROVE-IT [3] has shown that the addition of ezetimibe-an agent that reduces intestinal cholesterol reabsorption-is of little overall benefit or clinical benefit (composite cardiovascular endpoint) given a follow-up of seven years (32.7% vs. 34.7%, HR 0.936).
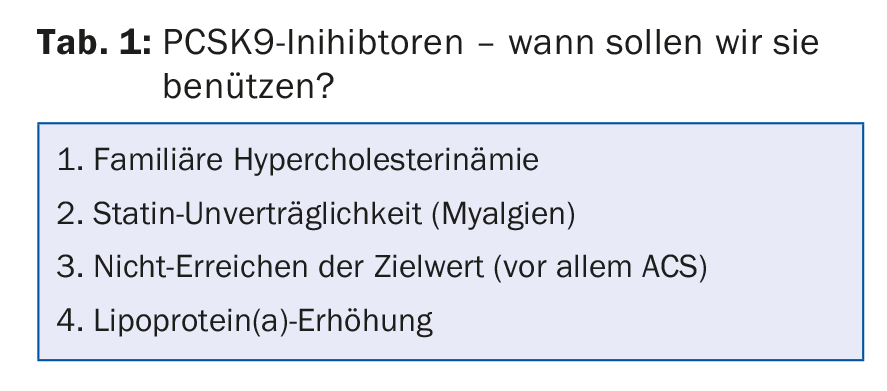
“In contrast, the PCSK9 inhibitors represent a much greater therapeutic advance – if you look at the current study situation,” said Prof. Lüscher. Given in addition to statins, they work significantly better than statins alone. After only one year, the cardiovascular event rate is already significantly reduced (the risk for such events is approximately halved, HR 0.47; p=0.003) [4], recent analyses suggest. Furthermore, regression of atherosclerotic plaques and a reduction in plaque volume, which is closely related to LDL, can apparently be achieved [5]. Furthermore, an emerging target for PCSK9 inhibitors is familial lipoprotein(a), which is an independent risk factor for cardiovascular disease [6]. Table 1 summarizes the evidence on PCSK9 inhibitors. “With these new agents, the target values are also becoming more important again. Currently, there is a transatlantic divide between the ESC and the US guidelines. The former advocate target values, the latter a dose-adapted approach,” the speaker explained.
Increase HDL?
Low HDL cholesterol is associated with increased cardiovascular risk despite intensive statin therapy [7]. Does increasing HDL cholesterol via pharmacotherapy therefore qualify as a treatment goal? The studies to date indicate that the event rate is not improved but, on the contrary, in some cases even worsened. This was illustrated, for example, by the AIM-HIGH study, which tested nicotinic acid in combination with a statin to increase HDL cholesterol levels. Or ILLUMINATE, where torcetrapib (in combination with a statin vs. statin alone) also greatly increased HDL while decreasing LDL in over 15,000 participants, but also significantly increased deaths and cardiovascular events (the trial was therefore stopped). The HDL mimetic CER-001 also shows no effect in coronary atherosclerosis according to the latest data. In contrast, there are promising findings with a Roux-en-Y gastric bypass – described in 2015 in Circulation [8].
Diabetes – a breakthrough at last
There is good news from the field of diabetes therapy: The SGLT2 inhibitor empagliflozin is the first drug available that convincingly and significantly improved cardiovascular endpoints (including mortality) in type 2 diabetics [9]. In turn, the LEADER study [10] showed a corresponding benefit with liraglutide, a GLP1 analog.
Depression – supply problems
“Depression often goes unrecognized. Those affected do not identify their own illness, diffuse physical complaints mask the actual depression or there is generally uncertainty about symptoms and diagnostic criteria. Which patients should we screen and how? These are questions that can arise in family practice,” said Prof. Dr. Birgit Watzke, Clinical Psychology with a focus on psychotherapy research, University of Zurich, by way of introduction. “This leads to the fact that depression is also inadequately treated.” On the one hand, there are diffuse fears and fears of stigmatization on the part of those affected about placing themselves in specialist (psychiatric) hands; on the other hand, the differentiated treatment recommendations according to severity or type of illness and patient preference require a “close look”. Monitoring is critical to the success of therapy. Further, there should be the best possible access to evidence-based psychotherapy.

The course of depression can be divided into different forms (Fig. 1) . Dysthymia with mild depressive symptoms over at least two years is particularly difficult to identify and less successful to treat than depressive episodes. Classification by severity (mild, moderate and severe) is also essential. According to ICD-10, there are main and additional symptoms. The former include:
- Depressed, depressive mood
- Loss of interest, joylessness
- Lack of drive, increased fatigability
Additional symptoms include:
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Feelings of guilt and worthlessness
- Negative and pessimistic outlook for the future
- Suicidal thoughts/actions
- Sleep disorders
- Decreased appetite
If two of the three main symptoms and two additional symptoms are present for at least two weeks, a diagnosis of “mild” depressive episode is made; if two main symptoms and three to four additional symptoms are present, a diagnosis of “moderate” is made; and if three main symptoms and more than four additional symptoms are present, a diagnosis of “major” depressive episode is made. The depressive episode can then be further divided into monophasic, recurrent, and bipolar forms.
Before ICD diagnosis according to severity, short screening tests can also be helpful: Two-question test (Tab. 2), screening questionnaire such as PHQ-9 if necessary.

Evidence-based practice
“What is often forgotten: Evidence-based action means not only incorporating the current state of knowledge from research into one’s practice, but also one’s own expertise and experience as well as patient preference (wishes, knowledge, and concerns),” Prof. Watzke emphasized. Basically, active observational support (for mild depression), psychotherapy, and antidepressants (combined for severe and equivalent alone for moderate depressive episode) are available for guideline-compliant therapy. “It is becoming apparent that antidepressants are currently used too frequently for mild depressive episodes. Here, a very critical use of these agents or a careful weighing of the risk-benefit ratio is recommended. Evidence is more supportive of efficacy in acute moderate episodes-where psychotherapy is equivalent and both treatment options may be considered as monotherapy. For acute major depressive episodes (and also chronic depression), combination is preferable to monotherapy. Unfortunately, there are still many individuals in this group who receive no therapy at all.”
After four weeks of unsuccessful treatment with antidepressants (after six in elderly patients), the therapeutic approach should be reviewed. In addition, there is continuous monitoring of side effects. This is because if the patient has side effects, he or she may stop taking the drug (poor compliance) and the lack of effect is self-explanatory. So again, patient preference and sensitivity is an important part of decision making.
The long duration of relapse prophylaxis is sometimes difficult to convey to the patient: Antidepressants should be taken for at least four to nine months beyond the remission of a depressive episode at the same dosage as in the acute phase and, in the case of recurrent episodes (≥2, with significant functional limitations), even longer – at least two years.
Low-threshold services for mild-grade episode
In the case of mild episodes, for example, low-threshold services or self-help, some of which draw on knowledge of psychotherapy, can come into play. These include:
- Bibliotherapy/self help book
- Internet-based self-help (especially promising for young people, but support from treatment providers is key)
- Psychotherapy telephone support.
Source: 56th Continuing Medical Education Course, February 2-4, 2017, Davos.
Literature:
- Li XS, et al: Gut microbiota-dependent trimethylamine N-oxide in acute coronary syndromes: a prognostic marker for incident cardiovascular events beyond traditional risk factors. Eur Heart J 2017 Jan 11. pii: ehw582. DOI: 10.1093/eurheartj/ehw582 [Epub ahead of print].
- Christoffersen M, et al: Visible age-related signs and risk of ischemic heart disease in the general population: a prospective cohort study. Circulation 2014 Mar 4; 129(9): 990-998.
- Cannon CP, et al: Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med 2015; 372: 2387-2397.
- Sabatine MS, et al: Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med 2015 Apr 16; 372(16): 1500-1509.
- Nicholls SJ, et al: Effect of Evolocumab on Progression of Coronary Disease in Statin-Treated Patients: The GLAGOV Randomized Clinical Trial. JAMA 2016 Dec 13; 316(22): 2373-2384.
- Gaudet D, et al: Effect of alirocumab, a monoclonal proprotein convertase subtilisin/kexin 9 antibody, on lipoprotein(a) concentrations (a pooled analysis of 150 mg every two weeks dosing from phase 2 trials). Am J Cardiol 2014 Sep 1; 114(5): 711-715.
- Barter P, et al: HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med 2007 Sep 27; 357(13): 1301-1310.
- Osto E, et al: Rapid and body weight-independent improvement of endothelial and high-density lipoprotein function after Roux-en-Y gastric bypass: role of glucagon-like peptide-1. Circulation 2015 Mar 10; 131(10): 871-881.
- Zinman B, et al: Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 2015 Nov 26; 373(22): 2117-2128.
- Marso SP, et al: Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 2016; 375: 311-322.
HAUSARZT PRAXIS 2017; 12(3): 33-36











