Bariatric and metabolic surgery is not only one, but the most effective treatment option for overweight type 2 diabetic patients. For the most important procedures performed today (gastric bypass Y-Roux or sleeve gastrectomy), high-quality randomized studies are available that have demonstrated a clear advantage for surgical therapy. Numerous studies demonstrate that bariatric and metabolic surgery can lead to significant improvement in glycemic control through both weight-reduction-dependent and -independent mechanisms.
The number of people with diabetes mellitus is constantly growing. According to the Swiss Diabetes Association, nearly 50,000 patients in Switzerland are affected by diabetes mellitus, most of them with type 2 diabetes. Patients with overweight (obesity), defined as body mass index (BMI) >30 kg/m2, and/or increased abdominal circumference are particularly at risk. More and more new cases of type 2 diabetes are occurring, especially in older segments of the population. Recent studies also show that the number of undiagnosed type 2 diabetes cases is as high as 50% of the known cases [1–3]. According to the International Diabetes Federation (IDF), a global organization dedicated to the research and treatment of diabetes mellitus, the number of type 2 diabetics worldwide is expected to increase from 387 million to more than 592 million in the next 20 years, which is disproportionate to world population growth. One possible explanation for this rapid increase is that newly diagnosed type 2 diabetics are getting younger and younger, which has already led to an additional increase in new cases of type 2 diabetes with the increasing number of overweight children and adolescents now [1,3].
Consequences of type 2 diabetes
Type 2 diabetes is defined as HbA1c of >6.0% and/or by the need for antidiabetic therapy [3]. Untreated or poorly controlled type 2 diabetes sooner or later leads to microvascular and macrovascular complications such as myocardial infarction, cerebral stroke, peripheral arterial disease (PAVD) or impaired renal function, including renal failure [1,3,4].
An overweight type 2 diabetic’s risk of death from stroke or myocardial infarction is increased by a factor of 3-5 compared with normal-weight people of the same age [3–5].
Type 2 diabetes in overweight people
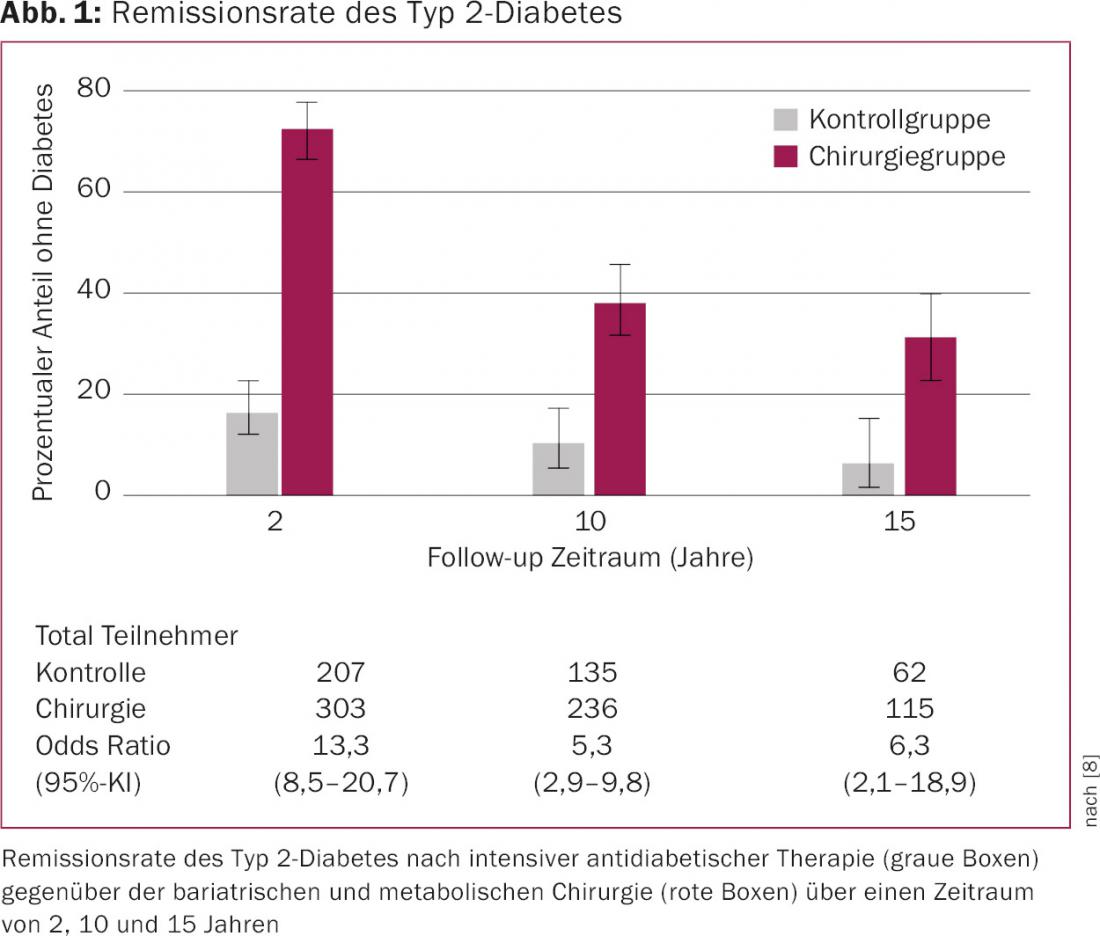
Recent studies show that type 2 diabetes in obese patients could be prevented in up to 50% of cases by timely lifestyle changes (balanced diet, appropriate exercise program, and medication) [4,5]. In contrast, the chance that an overweight type 2 diabetic will make his or her diabetes disappear with this multimodal therapeutic approach is small or only temporary. In the recently published study by Sjöström et al. the remission rate of type 2 diabetes after a period of 15 years with conventional methods was less than 6%, whereas bariatric and metabolic surgery achieved a much greater long-term therapeutic success of over 30% (Fig. 1) [6–8].
If one looks at late complications such as the incidence rate of myocardial infarction or cerebral strokes in overweight type 2 diabetics who managed to reduce their weight by conservative means, it becomes obvious that the risk of complications remains unchanged and thus the desired metabolic effect does not occur [4,5]. This suggests that much more should be invested in prevention or early detection of type 2 diabetes. The direct and indirect health care costs associated with the treatment of type 2 diabetes currently amount to 5.4 billion Swiss francs in Switzerland and are increasing annually [2].
Bariatric and metabolic surgery
The proportion of patients with impaired glucose tolerance or type 2 diabetes is about one-third among bariatric patients undergoing surgery. Rapid improvement in blood glucose metabolism occurs in some cases within the first few days after surgery, which is related to incretin hormones (e.g., glucagon-like peptide [GLP] 1). Weight reduction after bariatric and metabolic surgery alone cannot explain this improvement. Incretins are formed especially in the lower small intestine. If these intestinal segments are transplanted into the upper gastrointestinal tract or if the transit time of the food pulp is shortened, this results in a faster and stronger release of incretin hormones. This leads to an improvement in glucose metabolism [6,7]. Metabolic surgery is fundamentally aimed at specifically targeting this hormonal mechanism for the treatment of type 2 diabetes. Thus, metabolic surgery is not primarily aimed at inducing weight loss, but at improving metabolism.
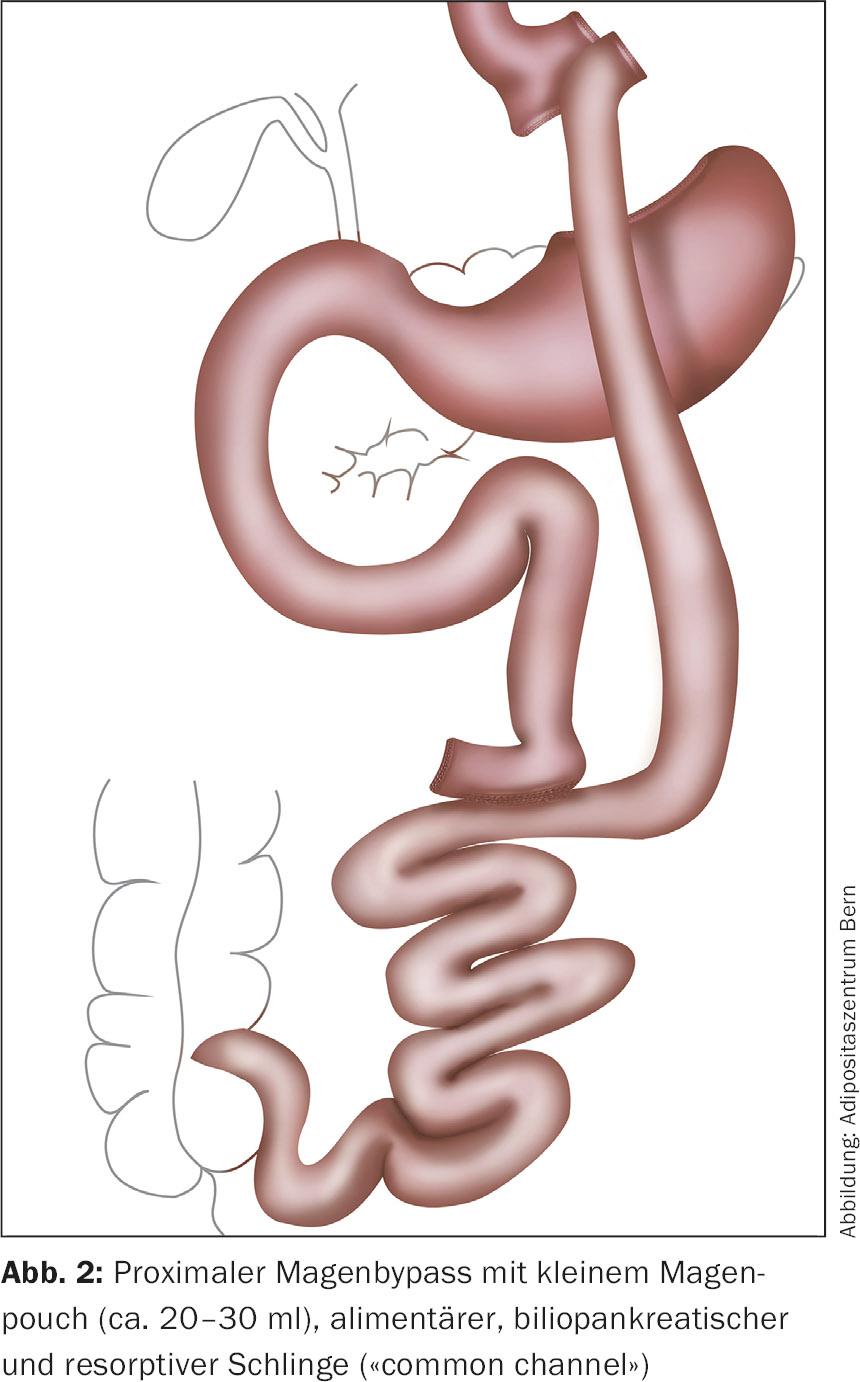
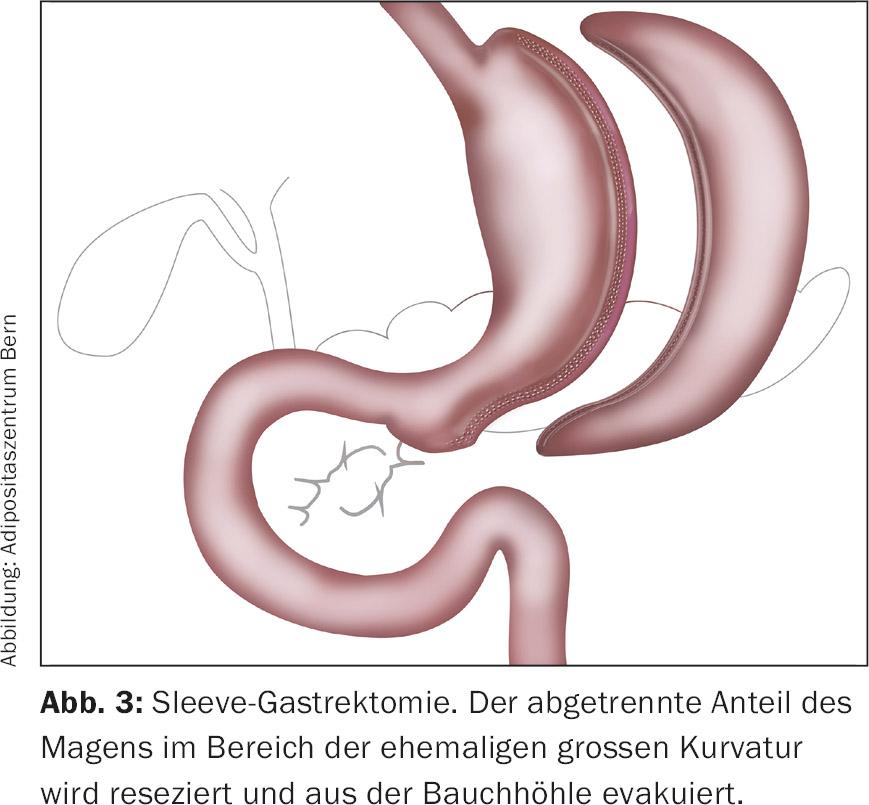
The Y-Roux proximal gastric bypass and sleeve gastrectomy are among the most commonly performed bariatric and metabolic surgeries today [9].
Gastric bypass Y-Roux
In the Y-Roux gastric bypass (Fig. 2), the formation of a small (approx. 20-30 ml) gastric pouch, which is separated from the rest of the stomach and connected to a jejunal loop eliminated after Roux-Y (gastrojejunostomy). This completely excludes the duodenum from the food pulp, which also leads to increased secretion of GLP-1. Footpoint anastomosis is usually performed 50-100 cm distal to the ligamentum Treitz and 150 cm distal to the gastrojejunostomy. In Y-Roux gastric bypass, the length of the resorptive small bowel segment is usually much longer than 200 cm as a result [9].
Sleeve gastrectomy
In sleeve gastrectomy (Fig. 3) , more than half of the stomach is resected on the large-curvature side, which leads on the one hand to food restriction and on the other hand to hormonal changes similar to those in Y-Roux gastric bypass due to the accelerated transit of the food pulp. The essential dissection step of sleeve gastrectomy is the complete dissection of the large gastric curvature close to the stomach wall with transection of the gastrocolic and gastrosplenic ligaments including the vasa gastricae breves. After completion of the dissection to the left diaphragmatic thigh, stapler resection begins approximately 4-6 cm orally of the pylorus with appropriate calibration with a probe (32-40 French). Salvage of the gastric resectate is performed via extension of a trocar incision [9].
Results in relation to type 2 diabetes
Schauer et al. reported that bariatric and metabolic surgery along with intensive antidiabetic therapy produced complete remission of type 2 diabetes after three years in 38% (Y-Roux gastric bypass) and 24% (sleeve gastrectomy) of patients. This was clearly statistically better than intensive antidiabetic therapy alone, which provided remission in only 5% [6,10]. In addition, weight loss, use of antidiabetic medication, and quality of life were also significantly better in the group of patients who underwent surgery.
In a recent study by Mingrone et al. demonstrated the sustained effect of bariatric and metabolic surgery on the remission rate of type 2 diabetes [7]. The patients on intensive antidiabetic therapy alone all had type 2 diabetes again after five years, whereas 50% of the patients who had surgery no longer needed to take antidiabetic drugs. This study highlights the sustainability of bariatric and metabolic surgery versus intensive antidiabetic therapy in relation to type 2 diabetes.
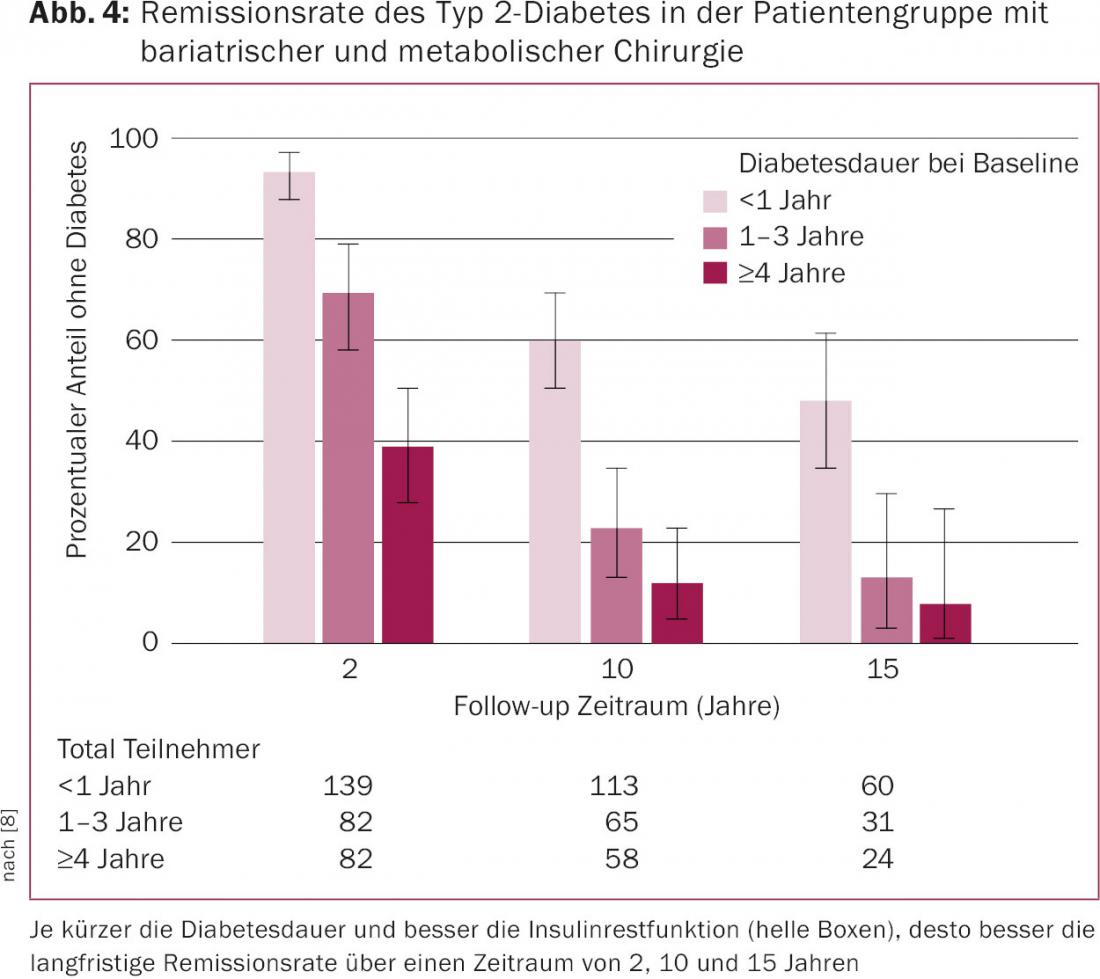
In the Swedish Obesity Study (SOS) by Sjöström et al. the above results could also be reproduced on a time horizon of 15 years [8]. Interestingly, however, significant differences were seen with respect to diabetes duration and residual insulin function. Thus, patients with a shorter duration of diabetes performed significantly better than long-term patients with installed insulin therapy (Fig. 4).
Who is suitable for surgery?
The most important criteria for surgical intervention are the patient’s willingness to change his or her lifestyle and accept the intervention as an aid, and the shortest possible duration of diabetes. Patients with a diabetes duration of less than five years and sufficient insulin residual function (as indicated by a relatively low need for antidiabetic therapy) are primarily eligible. Patients with many years of insulin therapy are much less suitable for bariatric surgery from a diabetological point of view, because the probability of remission is only low.
Follow-up of bariatric and metabolic surgery patients is of immense importance for treatment success and patient satisfaction. Therefore, patient compliance plays an important role in preoperative evaluation.
Literature:
- Maruthur NM: The growing prevalence of type 2 diabetes: increased incidence or improved survival? Curr Diab Rep 2013; 13(6): 786-794.
- Swiss Diabetes Society SDG-ASD, www.diabetesgesellschaft.ch
- Kerner W, Bruckel J: Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes 2014 Jul; 122(7): 384-386.
- Yamaoka K, Tango T: Efficacy of lifestyle education to prevent type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetes Care 2005; 28(11): 2780-2786.
- Wing RR, et al: Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013; 369(2): 145-154.
- Schauer PR, et al: Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012; 366(17): 1567-1576.
- Mingrone G, et al: Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 2015 Sep 5; 386(9997): 964-973.
- Sjöström L, et al: Association of Bariatric Surgery With Long-term Remission of Type 2 Diabetes and With Microvascular and Macrovascular Complications. JAMA 2014 Jun 11; 311(22): 2297-2304.
- Nett PC: Bariatric and metabolic surgery. Ther Umsch 2013 Feb; 70(2): 119-122.
- Schauer PR, et al: Bariatric surgery versus intensive medical therapy for diabetes-3-year outcomes. N Engl J Med 2014 May 22; 370(21): 2002-2013.
CARDIOVASC 2015; 14(6): 26-29











