Case Report: A six-month-old girl is referred for a circumscribed scarring skin lesion on the back of the head that has been present since birth. In addition, parents report persistent circular redness in this area. Pregnancy history was unremarkable and the baby was born by sectio on term.
Clinical picture: A solitary, sharply demarcated, oval-shaped, 5 mm measuring, pale erythematous is found at the occipital capillitium in the midline region. atrophic, hairless macula, aspectually corresponding to a thin, parchment-like membrane. The sharply demarcated area is surrounded by a narrow ring of dense, dark hair (Fig. 1). The child is otherwise healthy and thriving.
Quiz
Based on this information, what is the most likely diagnosis?
A Scar after birth trauma
B Aplasia cutis congenita
C wool hair nevus
D Nevus psiloliparus

Correct answer and diagnosis: The correct answer is B. The diagnosis is aplasia cutis congenita (ACC) with so-called “hair collar sign”.
Discussion: The presentation in the present case corresponds to a membranous ACC type 1 according to Frieden [1]. (“Scalp ACC without multiple anomalies”), which is the most common and is often surrounded by a narrow fringe of dense, dark hair (the so-called “hair collar sign”). Interestingly, a capillary malformation of the nevus simplex (stork bite) type is usually observed perifocally at the same site, as can be clearly seen in the images.
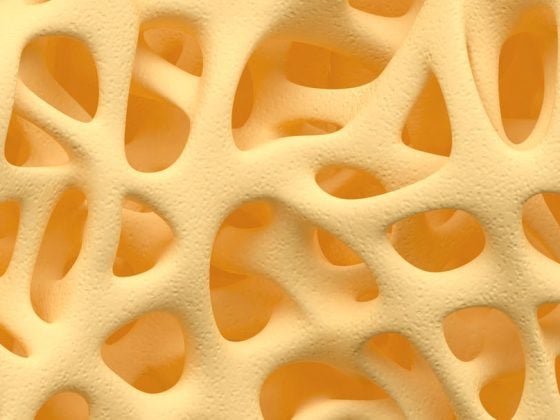
ACC is a skin defect, usually circumscribed, acquired intrauterine, characterized by the lack of attachment of the epidermis and dermis, and rarely deeper layers including the bone, dura, and meninges [1,2]. Genetic factors, intrauterine trauma, infections, amniotic defects, and teratogenic drugs are discussed as causes [1,3]. Following Frieden’s classification [1], nine different forms of ACC are distinguished. In about 80% of cases, ACC is localized to the scalp. The diagnosis of ACC is primarily made clinically. Rarely, ACC occurs in association with syndromal disorders (especially Adams Oliver syndrome and Goltz-Gorlin syndrome), ectodermal dysplasias, epidermal and organoid nevi, cranial dysraphia, fetus papyraceus, epidermolysis bullosa [1]. Mostly a sporadic occurrence is found, rarely an autosomal dominant inheritance. Depending on the subtype, the clinical presentation of ACC is variable. In isolated membranous type I ACC, the skin defects are usually max. 1-2 cm in size [4]. After re-epithelialization has occurred, which may occur in utero, an atrophic, pale hairless scar is found; occasionally multiple ACC sites are present adjacent to each other. At birth, sharply demarcated erosive or ulcerated areas or a circumscribed, hairless, velvety reddened skin defect covered by a thin, parchment-like membrane (membranous ACC) (Fig. 2) [1,3]. Membranous ACC, usually localized in the vertex area adjacent to the parietal hair vortex, represents the most common manifestation. The “hair collar sign” (Fig. 2) is considered by some authors to be a relatively specific marker for CNS dysraphism iS. of an underlying (rudimentary) encephalocele. However, it is the case that many small isolated membranous ACC are accompanied by a “hair collar sign” without finding underlying CNS defects. The risk for a corresponding malformation and thus the indication for specific imaging (sonography in very young infants and magnetic resonance imaging) is particularly present in the following situations:
- large, deep, irregular defect (possibly with crusts, granulation tissue, typically at the vertex)
- palpable osseous defect
- with very conspicuous hair collar sign and localization in the middle of the lower occiput and highoccipital (Fig. 2) as well as above the spine

In our patient, due to the overall discreet presentation and lack of the above criteria, we did not perform further imaging workup.
Treatment of small membranous ACC is not mandatory, but may be performed in the course for aesthetic reasons and consists of total excision of the finding. For deeper defects, surgical coverage with skin grafts is indicated to avoid complications [2].
Literature:
- Peace IJ. Aplasia cutis congenita: a clinical review and proposal for classification. J Am Acad Dermatol 1986; 14(4): 646-660.
- Maillet-Declerck M, Vinchon M, Guerreschi P et al. Aplasia cutis congenita: review of 29 cases and proposal of a therapeutic strategy. Eur J Pediatr Surg 2013; 23(2): 89-93.
- Browning JC. Aplasia cutis congenita: approach to evaluation and management. Dermatol Ther 2013; 26(6): 439-444.
- Mesrati H, Amouri M, Chaaben H, Masmoudi A, Boudaya S, Turki H. Aplasia cutis congenita: report of 22 cases. Int J Dermatol 2015; 54(12): 1370-1375.
DERMATOLOGIE PRAXIS 2016; 26(3): 26-27