Eczematous skin lesions and itching can have a significant negative impact on quality of life. Pathophysiologically, an immunological dysregulation and a disturbed skin barrier are central factors of this multifactorial disease. Restoration of impaired barrier function is essential in the therapeutic management of atopic dermatitis and is an important guideline-based therapeutic pillar.
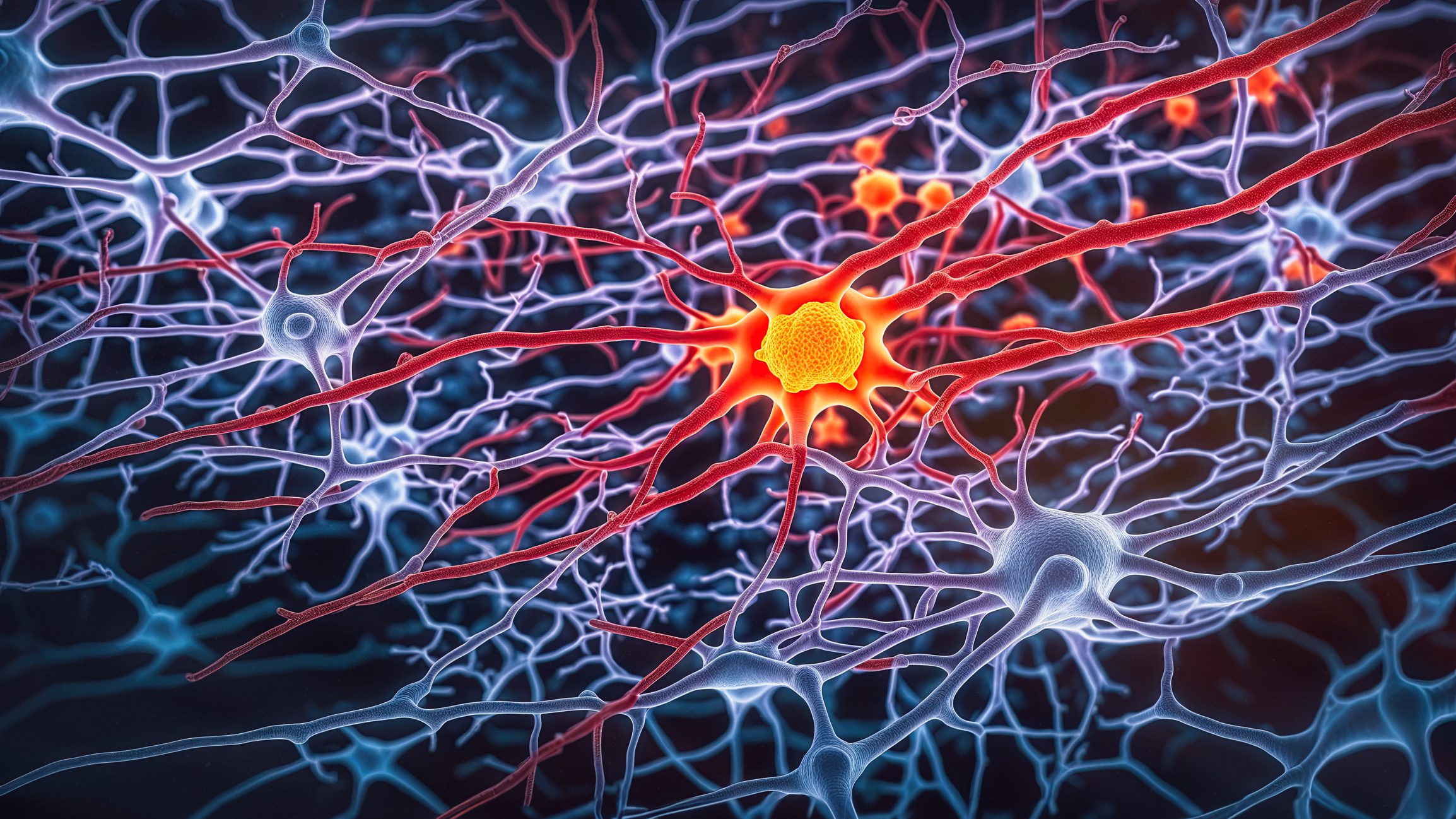
Atopic dermatitis is a common multifactorial chronic inflammatory skin disease. The prevalence is 10-15% in children and approximately 3% in adults [1,2]. The interaction of genetic predisposition, exogenous trigger factors (e.g., irritants, allergens, etc.) and endogenous factors (e.g., stress, hormones, etc.) plays an important role in the initial manifestation and chronification [2]. A defective epidermal skin barrier is characteristic of atopic dermatitis and, as a consequence, microbial, irritant, allergenic, or nonspecific trigger factors can initiate or exacerbate a cutaneous inflammatory response [3–5]. The interaction structure is extremely complex; dysregulated immunological reactions are significantly involved in inflammatory processes. “Pathophysiologically essential aspects are the disturbed skin barrier and the genetic disposition – in interaction this leads to an activation of the immune system”, Prof. Dr. med. Margitta Worm, Charité Universitätsmedizin Berlin (D), summarizes the multifactorial process [6]. At the immunological level, Th2-mediated cytokine release, among other factors, plays a central role in atopic inflammatory processes.
Filaggrin deficiency as an essential aspect of impaired barrier function.
In particular, the top layer of the epidermis, the stratum corneum, has an important protective function with regard to penetration of irritants and allergens and reduces water loss through the skin [7]. Keratinocytes reach the stratum corneum after proliferating from the stratum basale through the stratum spinosum. In the stratum corneum, they are transformed into nucleated corneocytes and finally shed as skin scales. In patients with atopic dermatitis, the structure of the epidermal skin barrier exhibits specific alterations at different levels. First, altered expression of filaggrin is characteristic, which is due to genetic mutations, exogenous influences, and inflammation-related cytokines [8]. Furthermore, empirical studies have found an altered composition of epidermal lipids with a reduction in ceramides [9].
By aggregating keratin filaments into tightly packed bundles and attaching them to a protein structure surrounding the corneocytes, to which lipids in the intracellular matrix bind covalently, filaggrin plays a crucial role in the epidermal skin barrier [7]. In addition, this structural protein has an important function in the regulation of skin hydration by cleaving into amino acids in the stratum corneum, which act as natural moisturizing factors (NMF) to hydrate the cornea and reduce transepidermal water loss (TEWL) through their water-retaining effect. [10] (Fig. 1). Reduced production of filaggrin, typical of atopic skin, is associated with increased moisture loss, among other factors. “The skin is less moist, has a lower buffer capacity, the ph value increases and associated with this, bacteria can multiply. Overall, this results in increased sensitivity of the skin,” explains Prof. Worm. The causes of filaggrin deficiency are thought to be loss-of-function mutations in the filaggrin gene, as well as exposure to irritant factors and inflammatory processes [7].

Basic therapy as a guideline-based therapy pillar
“Positive family history, chronic recurrent course of skin symptoms in the area of predilection sites and the central symptom of itching are the main criteria of atopic dermatitis,” she said. In addition, there are various secondary criteria (e.g., ichthyosis vulgaris, keratosis follicularis, cheilitis, periorbital shadowing). Therapy of atopic dermatitis is stage-adapted, with basic therapy being an important treatment pillar for all four stages (dry skin, mild eczema, moderate eczema, persistent, severe eczema) [11]. At level 1, basic care is sufficient; from level 2, the combination with topical interval therapy (levels 2 and 3) or systemic treatment (level 4) proposed [11]. A consistent basic therapy is an essential factor for the regeneration of the disturbed barrier function, as well as for the reduction of xerosis and itching [5]. Furthermore, adequate baseline therapy was shown to reduce the need for topical steroids in acute eczema episodes, and a prolonged relapse-free interval was observed in long-term management. “Consistent topical base therapy with lipid-replenishing topicals is extremely important,” summarizes Prof. Worm. The selection of care products should be adapted to individual patient characteristics and symptom manifestations.

This also corresponds to the core statement of the current s2k guideline, which recommends a basic therapy adapted to the skin condition, appropriate skin cleansing and baths (with subsequent refatting treatment) [11]. An important note in the guideline is to use basic therapeutics without adding contact allergenic substances. Products containing certain fragrances or preservatives can lead to contact allergy if used for a long time, the speaker explained. Suitable ingredients of refatting topical preparations are urea, glycerin and ceramides. Their efficacy on relevant clinical parameters has been scientifically proven (table 1). For urea and glycerol, there is an explicit recommendation in the s2k guideline, but it is not recommended for infants because it can lead to burning [11]. Agents that may be considered as adjuvant antipruritic treatment, although no evidence-based treatment recommendation is made, are polidocanol and tannins. These two substances reduce itching, but do not represent an actual anti-inflammatory treatment, but can be used as add-ons. Based on general clinical experience, zinc is recommended as a basic therapeutic agent.
Source: FomF (D) Dermatology and Allergology 2020
Literature:
- Schnopp C, Mempel M: Atopic eczema in children – Current aspects. Dermatologist 2015; 66: 245-251.
- Weidinger S, Novak N: Atopic dermatitis. The Lancet 2016; 387: 1109-1122.
- Volz T, et al: On the role of the innate immune system in atopic dermatitis. Dermatologist 2015; 66: 90-95.
- Biedermann T, et al: Regulation of T Cell Immunity in Atopic Dermatitis by Microbes: The Yin and Yang of Cutaneous Inflammation. Front Immunol 2015; 6: 353.
- Chylla R, Schnopp C, Volz T: Basic therapy in atopic dermatitis – new and proven. JDDG 2018; 16 (8): 976-980.
- Worm M: Atopic eczema 2020. Prof. Dr. med. Margitta Worm, Dermatology and Allergology Refresher, FomF.de, Hofheim (D), 12.09.2020.
- Engebretsen KA, Thyssen JP: Skin barrier function and allergens. Karger Compass Dermatol 2017; 5: 7-13.
- Thyssen JP, Kezic S: Causes of epidermal filaggrin reduction and their role in the pathogenesis of atopic dermatitis. J Allergy Clin Immunol 2014; 134: 792-799.
- Jungersted J, et al: Stratum corneum lipids, skin barrier function and filaggrin mutations in patients with atopic eczema. Allergy 2010; 65: 911-918.
- Peter M: Atopic dermatitis emollients – still a central element of basic therapy, DERMATOLOGIE PRAXIS 2020; 30(2): 20.
- AWMF: Guideline Neurodermatitis, Register number 013 – 027, ClassificationS2k Status: 31.03.2015. www.awmf.org
- Levin J, et al: Atopic dermatitis and the stratum corneum: part 1: the role of filaggrin in the stratum corneum barrier and atopic skin. J Clin Aesthet Dermatol 2013; 6(10): 16-22.
DERMATOLOGIE PRAXIS 2020; 30(5): 24-26 (published 8/10/20, ahead of print).