Allergen-specific immunotherapy is established as an immunomodulatory therapy for inhalant and hymenopteran venom allergy. Both subcutaneous injection therapy and the sublingual form of therapy are considered safe, but allergic reactions can still occur – sometimes due to human error, as one case study shows.
A 20-year-old female patient presented for an allergic episode following a bee sting. The young woman also suffered from “blood injection type phobia.” Intradermal skin tests with bee venom were positive (0.1 µg/ml) and with wasp venom negative. Specific IgE and IgG were positive only for bee venom and were undetectable for wasp venom. There was no atopy or evidence of mastocytosis, write Prof. Dr. Andreas J. Bircher, University Hospital Basel, Dr. David Spoerl, University Hospital Geneva, and Kathrin Scherer Hofmeier, Kanstonsspital Aarau [1]. With the patient’s consent, immunotherapy with bee venom was started: After initial Ultrarush procedure, she received full dose of 100,000 SQU bee venom in monthly intervals. The injections were tolerated without problems, and no field stitches were suffered.
In the third year of immunotherapy, the woman was accidentally injected subcutaneously with 100,000 SQU of wasp venom instead of the bee venom. Since the patient had no evidence of pre-existing sensitization with wasp venom, she was monitored for one hour after the injection, after which serum was collected. Only a mild local reaction occurred, which is why medicinal measures were dispensed with. The patient was discharged with an emergency medication kit and instructions. Subsequently, immunotherapy with bee venom was continued as planned.
After several weeks, an increase in the initially negative wasp venom-specific IgE and IgG antibodies was documented. Thus, active sensitization by the high single dose of wasp venom must be assumed. Immunotherapy with bee venom was completed after the recommended duration of five years. Immunotherapy with wasp venom was not performed because there was no provable clinical relevance of the sensitization and the patient should not be exposed to additional stress.
|
New release In spring 2022, the volume “Errors and Mistakes in Dermatology and Allergology. Patient Safety and Quality Management” will be published by Thieme-Verlag. Casuistries are presented that are based on cases of the conciliation boards at the state medical associations in Germany, but also on civil court medical liability proceedings and expert opinions. All reports are divided into a case description, consequences for patients, interpretations from the court or reviewer’s perspective, recommendations for professional error management, and take-home messages on how to avoid the errors next time. The volume is primarily aimed at dermatologists, but also contains an extensive section on allergology in which nine case reports are presented, including, in addition to the one described here, failure to provide emergency treatment for acute allergic contact dermatitis, a severe anaphylactic reaction to skin testing with ceftriaxone, and tongue swelling after penicillin and negative allergy workup. Elsner P, Meyer J, Lehmann P, Bircher A, eds: Errors and Misconceptions in Dermatology and Allergology. 1st ed. Stuttgart: Thieme; 2022. |
Possible case of negligent physical injury
Since the manufacturer’s vials of bee and wasp venom look virtually identical, they were marked with different color labels. Thus, in This Case, there was likely a human error, i.e., switching an allergen vial that was intended for another patient, the authors write.
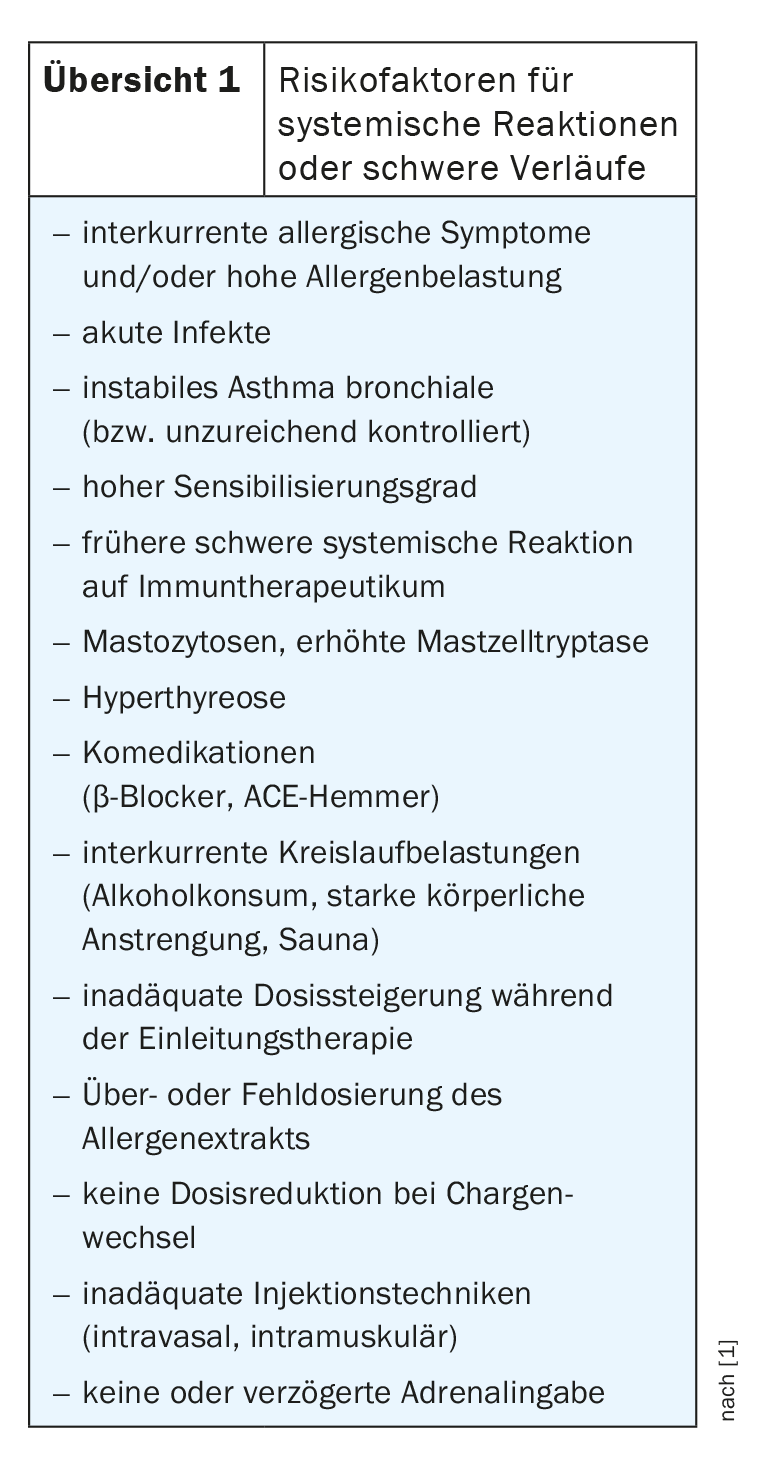
Errors of this type are officially rare (approx. 0.1-0.2% of all injections), but an estimated number of unreported cases must be expected. A survey of American allergists showed that within five years, three quarters of them had given a majority of 1-3, in some cases up to 10 incorrect injections. Patients were given the wrong doses as well as the wrong allergen. Particularly in the case of incorrect dosing, in addition to patient-related risk factors such as asthma, comedication with beta-blockers and injections during exacerbations or infections (overview 1), allergic reactions can occur.
The induction of a new sensitization is to be considered as clearly more serious than a too high allergen dose or the disregard of intercurrent risk factors. Although the patient in the case study did not suffer any immediate serious side effects, permanent “damage” was set in this case as a result of medical malpractice, the authors explain. Legally, this could possibly be negligent bodily injury. However, in this case, the young woman refrained from taking legal action against those treating her.
Literature:
- Bircher A, Spoerl D, Scherer Hofmeier K: Wasp instead of bee – accidental neusensitization to wasp venom under immunotherapy with bee venom. In: Elsner P, Meyer J, Lehmann P, Bircher A, eds: Errors and misconceptions in dermatology and allergology. 1st edition. Stuttgart: Thieme; 2022.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(2): 20
HAUSARZT PRAXIS 2022; 17(8): 38