PD Dr. med. Dr. sc. Nat. Alexander Navarini, Department of Dermatology at the University Hospital Zurich, held a workshop on psoriasis at Medidays. Moderate to severe psoriasis can be very stressful for patients and significantly reduce their quality of life, which is why accurate diagnosis and comprehensive therapy are very important.
(ee) In the family doctor’s practice it is often not so easy to distinguish psoriasis from other skin diseases (neurodermatitis, eczema, mycosis, etc.). Typical signs of psoriatic plaque include sharply demarcated erythema, scaling, and elevation of the lesion. Psoriasis often occurs symmetrically. Predilection sites are elbows and knees, scalp, lower back, hands and feet. A distinction is made between the well known psoriasis vulgaris and psoriasis inversa, which occurs at flexion sites and in body folds (armpits, gluteal cleft) and often without scales. In erythrodermic psoriasis, more than 90% of the skin is affected.
Concomitant diseases in psoriasis
During the work-up, typical accompanying symptoms should be sought. These include map tongue, nail manifestations (yellowish patches, dimples, spotted nails), an infestation behind the ears, and psoriatic arthritis, which affects about 20% of psoriasis patients. Especially in moderate to severe psoriasis, patients are at increased risk for comorbidities such as hypertension, metabolic syndrome, coronary artery disease, and Crohn’s disease. Depression is also common, and 10% of severely affected patients become suicidal during the course of the disease.
Severity assessment
For the therapy decision, the severity of the psoriasis must first be assessed. Three scores are available for this purpose:
- Body Surface Area (BSA): If more than 10% of the skin surface is affected, the psoriasis is severe. One palm plus fingers corresponds to about 1% of the body surface.
- Psoriasis Area and Severity Index (PASI): Assesses the extent of erythema, infiltration and scaling on different parts of the body.
- Dermatology Life Quality Index (DLQI): Answering ten questions about quality of life related to skin disease.
For all three scores, a value above ten points means that severe psoriasis is present. This is also recognized by health insurers. If the severity is less than ten points, topical therapy is usually given.
Therapy of “mild” psoriasis
The local therapy of mild psoriasis consists of various cornerstones (Tab. 1) . As a rule, topical therapies do not cause severe side effects, but they are often time-consuming and inconvenient. Good skin care and refatting can help save steroids. Recommended is one warm bath per day followed by a re-fatting (re-fatting should be done a total of three times a day). Salicylic acid and urea are used to dissolve dandruff. However, salicylic acid is not suitable for the therapy of children and in case of infestation of >20% of the skin due to its toxic effects. Polidocanol (e.g. Optiderm®), antihistamines or menthol can be used to combat itching.
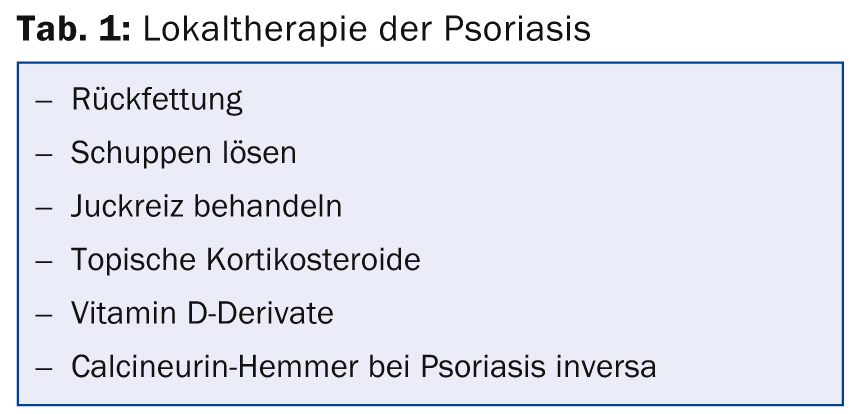
Topical steroids are divided into four classes. Treatment with a class IV steroid has a significant effect in about 80% of patients within three weeks. However, the steroids can cause side effects such as skin atrophy and redness. If a strong steroid is applied to the same skin site twice a day for two months, the skin atrophy is irreversible! The calcineurin inhibitors tacrolimus (Protopic®) and pimecrolimus (Elidel®) work very well in psoriasis inversa. They have little effect on typical psoriasis plaques.
Therapy of moderate to severe psoriasis
A PASI >10 or a BSA >10% and a DLQI >10 indicates moderate to severe psoriasis. Phototherapy and/or systemic therapy is indicated in these patients. Fumarates, methotrexate, retinoids (Neotigason®) and ciclosporin are used for classical system therapy. With ciclosporin therapy, 90% of patients experience at least 75% improvement in skin condition. However, ciclosporin is not suitable for long-term therapy because of its problematic side effects.
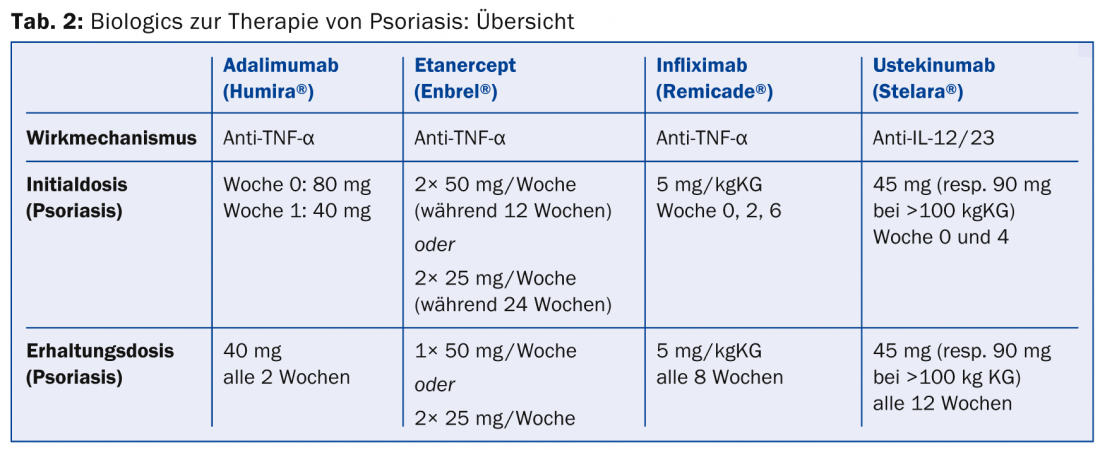
Relatively new on the market are the biologics (tab. 2) . For many patients for whom the “old” systemic therapeutics do not work or do not work sufficiently, the biologics are a blessing. “Patients describe the difference from before to after like night and day,” the speaker said. “With therapy, extensive plaques are gone all at once, which also has a huge impact on patients’ social lives.” The biologics also have very few side effects. However, treatment with biologics is very expensive (around CHF 30,000 per year).
Many patients are also interested in alternative therapies, for example, balneotherapy at the Dead Sea, dietary changes or the removal of skin scales by kangal fish. There is no evidence for these treatment approaches, but they may be helpful in individual cases.
Source: Medidays, Workshop “Psoriasis”, September 3, 2014, Zurich
DERMATOLOGIE PRAXIS 2014; 24(6): 44-45











