Patients with diabetes mellitus and obesity are at high risk for developing cardiovascular diseases such as myocardial infarction, stroke, and heart failure. An interdisciplinary management of the cardiometabolic risk patient therefore addresses cardiovascular risk reduction in patients with CKD, provides an update on heart failure therapy, and focuses in detail on fatty liver and its importance as a risk marker or target for therapeutic intervention for cardiovascular risk reduction.
Chronic kidney disease (CKD) has been moving in a negative direction in recent decades with respect to mortality. Out of 24th place among the leading causes, CKD is currently ranked 16th – with an estimated trend to 5th place in 2040. “Thus, cardio-renal prognosis will be the decisive factor for survival probability in the future,” reported Prof. Roland Schmieder, MD, Erlangen (D). Cardiovascular risk of CKD is determined by albuminuria and glomerular filtration rate (eGFR) using serum creatinine determination. Both factors are predictors of cardiovascular mortality and all-cause mortality. In patients with type 2 diabetes, there is increased excess mortality when renal disease is added (4.1% vs. 47% at 10 years). According to the KIDIGO guidelines, therapy management in patients with diabetes and CKD should therefore reduce both the risk of CKD progression and cardiovascular disease. For this, an HbA1c value between 6.5% and 8.0% and a blood pressure <140/80 mmHg are recommended. For this purpose, the blockade of the RAS system has been established. Several studies have demonstrated both cardioprotection and specific nephroprotection. RAS therapy should be continued even if eGFR <is 30 mL/min/1.73m2, a recent study has shown.
In a further step, SGLT2 inhibitors may also improve cardio-renal prognosis. In the meantime, several studies have shown not only a reduction in the risk of cardiovascular death in patients with type 2 diabetes, but also nephroprotection independent of diabetes status. Most recently, a prespecified exploratory pooled analysis with finerenone versus placebo demonstrated that in patients with type 2 diabetes and stage 1-4 CKD with moderate to severe albuminuria, well-controlled blood pressure and HbA1c, without the presence of symptomatic HFrEF, and treated with optimized RAS inhibitors, the risk of cardiovascular mortality was reduced by 14% and that of CKD progression by 23%.
New approaches in the therapy of heart failure
Just in the past year, a lot has happened in the therapy management of heart failure (HF), explained PD Katharina Schütt, MD, Aachen (D). Most importantly, a new universal definition of heart failure has been established. According to the study, anyone with symptoms or signs of heart failure who also has either an elevated Nt proBNP or signs of cardiac congestion is suffering from heart failure. HF is classified based on left ventricular ejection fraction (LVEF) (Table 1) .
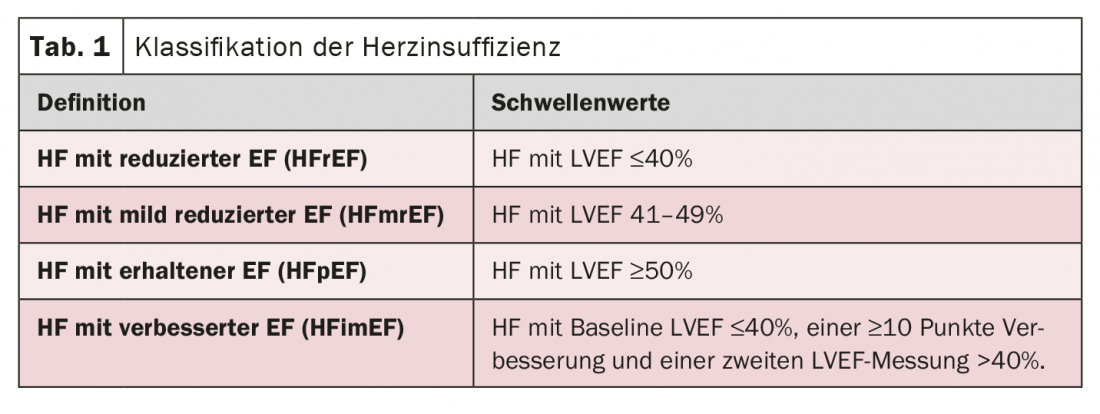
With the new ESC guideline, HFrEF patients will now no longer be treated in a staged regimen. Rather, all four substance groups (ACE-I/ARNI, beta blockers, MRA, and SGLT-2 inhibitors) should be used equally and in combination. The patient population of HFmrEF is very heterogeneous. However, in many cases they resemble HFrEF patients. In this case, diuretics are usually recommended for therapy. However, because there is also a potential benefit of treatment management of HFrEF patients for HFmrEF, this approach may also be considered. In patients with preserved pump function (HFpEF), it should not be ignored that their mortality risk is as high as in HFrEF patients, the expert cautioned. To date, however, no convincing data have been collected for a reduction in morbidity and mortality. The focus in this clientele is therefore on the management of comorbidities. Only the results of the EMPEROR-Preserved study give hope. Empagliflozin was the first compound to reduce the primary endpoint of cardiovascular death by 21% in patients with HFmrEF and HFpEF. The risk of hospitalization due to HF was also reduced by 27%. At the same time, renal function was stabilized.
Fatty liver risk marker?
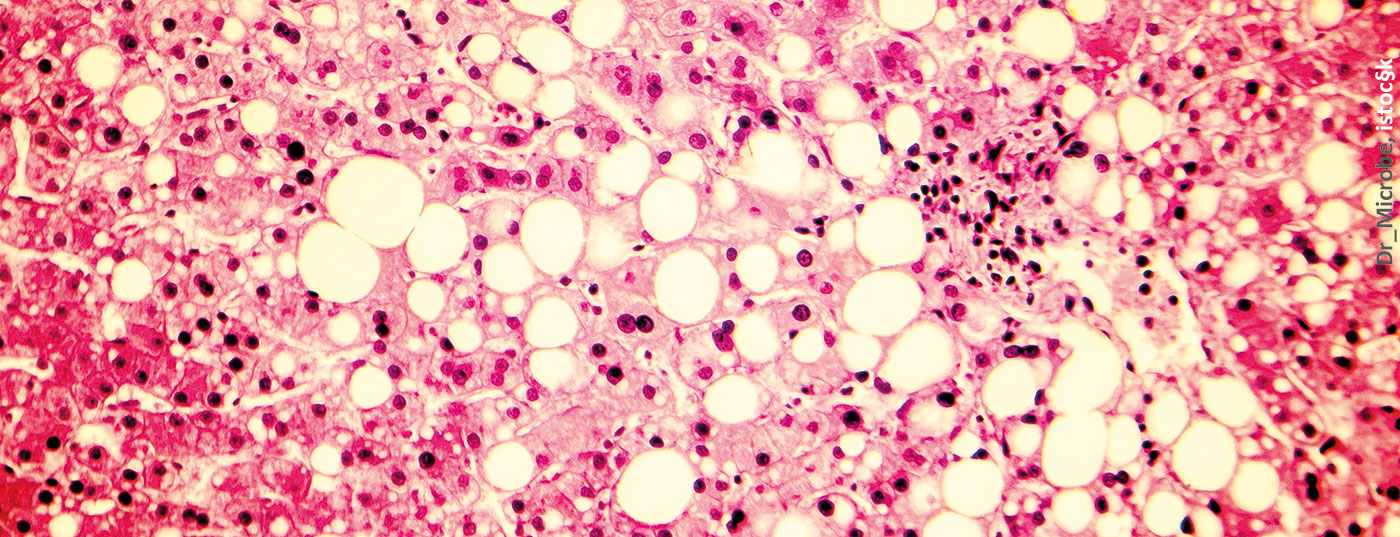
Dr. Sabine Kahl, Düsseldorf (D), addressed the third complex, fatty liver. Non-alcoholic fatty liver (NAFLD) is said to occur when the liver fat content is ≥5.56% and the percentage of hepatocytes with lipid storage is >5%, and other diseases can be excluded. It is estimated that about 25% of the world’s population is affected by this disease. But NAFLD is closely associated with type 2 diabetes. Thus, 70-80% of diabetic patients also present with NAFLD – with an increased risk of progression to fibrosis, cirrhosis, or liver cancer. In addition, NAFLD is a risk factor also for diabetes-related complications, such as cardiovascular disease, CKD, or retinopathy. In fact, the leading causes of death in NAFLD patients include cardiovascular disease (43%), extra-hepatic malignancies (19%), and liver cancer (5%) and cirrhosis (4%).
There is no approved medication for the indication of fatty liver disease yet. Treatment approaches in NAFLD sufferers with type 2 diabetes and obesity include lifestyle interventions, pharmacotherapy, and metabolic surgery. A weight loss of 5-10% of body weight should be targeted. However, only 10% of those affected achieve this through lifestyle interventions, the expert said. Pharmacological interventions do not currently exist. Numerous drugs have failed Phase III clinical trials. Fortunately, in the area of diabetes, antidiabetic medication can be used to try to affect NAFLD as well. In NASH, improvement in histology was demonstrated for pioglitazone as well as liraglutide and semaglutide, but nothing in fibrosis stage. SGLT2 inhibitors have also been investigated for their use in NAFLD. This showed good effects on liver fat content. Consideration is given to whether a combination of SGLT2i and GLP-1-RA might have synergistic effects with respect to blood glucose, weight reduction, cardiovascular risk, CKD risk, and also NAFLD.
The expert summarized that NAFLD is not only a risk marker, but should also be targeted for treatment. Currently, the basis of treatment is still lifestyle modification with the goal of weight reduction. Combined administration of GLP-1-RA and SGLT2i may be an effective therapeutic strategy in the future for patients with additional type 2 diabetes.
Source: Interdisciplinary Management of the Cardio-Metabolic Risk Patient – Update 2022. 27.05.2022, 16:00-17:30, Room 8
Congress: 56th Annual Meeting of the German Diabetes Society (DDG)
CARDIOVASC 2022; 21(2): 32-33