Chronic hand eczema persists for more than three months and is considered a socially relevant condition. Risk factors include atopic skin diathesis and genetic predisposition. What forms are there and what are the treatment options?
Chronic hand eczema is a very common and socially relevant condition. Almost one fifth of all occupational diseases affect the skin, of which, in turn, about 90% are due to allergic and toxic-irritant contact eczema, predominantly on the hands and forearms, according to statistics from the Swiss Accident Insurance Fund (SUVA). The prevalence in the population is about 10%, but in certain occupational groups (hairdressers, bakers, nursing professions, etc.) it is significantly higher [1]. Both the quality of life and the patients’ ability to work are severely limited as a result. Risk factors include atopic skin diathesis and genetic factors. Contributing to the development and maintenance are exposures to workplace irritants such as water, detergents, dirt, or other allergens [2–4].
Definition
Acute and subacute hand eczema are defined as inflammatory, non-infectious skin lesions of the hands that last less than three months and occur no more frequently than once a year. Chronic hand eczema is defined as hand eczema that persists for more than three months or occurs at least three times a year despite adequate treatment and patient cooperation [1].
The chronic hand eczema – clinic
Chronic hand eczema manifests itself clinically in sometimes very different ways. The morphea may change in the course of the disease: In the acute stage, there is intense redness, swelling, vesicles and sometimes severe itching. As the disease progresses, typical chronic signs of inflammation such as erythema, hyperkeratosis, scaling, rhagades, lichenification and pruritus appear. The clinical symptoms are rarely clearly indicative of the cause. For example, dyshidrosiform hand eczema is described purely in terms of morphology, as the causes may be different.
Classification according to etiology
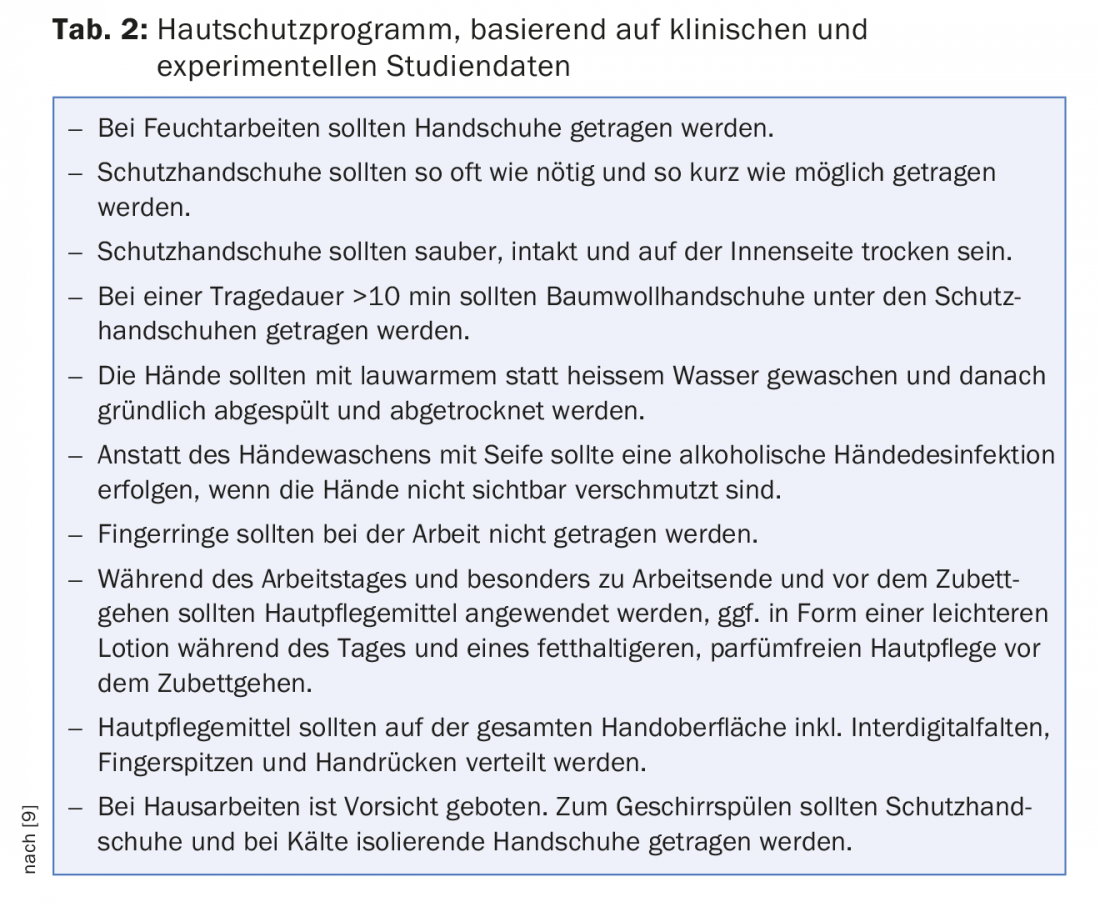
Moreover, chronic hand eczema is rarely caused monocausally, but mixed forms are usually present. A distinction is made between irritant (IHE), contact allergic (KHE) and atopic hand eczema (AHE) (Table 1).
Contact Allergic Hand Eczema: Contact allergic hand eczema is localized at the site of exposure to the contact allergen. However, scattering phenomena may also occur. Clinically, it initially presents with redness, edema, vesicles, and severe pruritus. In the later course, lichenification, hyperkeratosis, rhagades and chronic pruritus occur. The most common triggers are the following contact allergens: nickel, fragrances, perubalsam, cobalt, potassium dichromate, hairdressing substances, rubber ingredients, preservatives, and epoxy resins (Fig. 1) [6].

Irritant/cumulative subtoxic hand eczema: Irritant hand eczema usually begins on the backs of the hands and fingers and, as it progresses, also affects the palms. No scattering phenomena occur. Clinically, the initial stage shows rough, dry and scaly skin, followed by lichenification, redness, hyperkeratosis, rhagades and pruritus. Triggers are wet work, frequent hand washing, irritating substances (e.g. solvents, chemicals, coolants/lubricants, soaps, cleaning agents) or prolonged wearing of rubber or plastic gloves (Fig. 2).

Atopic hand eczema: In atopic hand eczema, the backs and palms of the hands, wrists, lateral finger areas, interdigital spaces and occasionally the fingertips are affected in the form of pulpitis sicca. Initially, there is vesiculation, as well as dryness, redness and scaling, and severe pruritus; later, there is infiltration, redness, hyperkeratosis, rhagades, and lichenification. Other manifestations of atopic dermatitis may occur at other sites (Figs. 3 and 4).


Dyshidrotic hand eczema: There is redness, dyshidrotic vesicles, papules, edema, and partial scaling, especially palmar and on the lateral edges of the fingers (Fig. 5).

Diagnostics
A careful history should be taken as well as a clinical status survey of localization and morphology. It is particularly important to ask about occupational activities (skin contact with certain contact substances, wearing gloves, moist activities), domestic exposure and hobbies (DIY activities). In addition, the course during non-working time/vacation should be ascertained, as this can provide information about the occupational context. A detailed history of other skin diseases (especially atopic eczema, psoriasis) and a careful examination of the rest of the integument are also important.
In addition, patients with hand eczema who persist for more than three months and/or show a recurrent course should undergo epicutaneous testing to clarify the role of possible contact allergens. The standard series as well as – depending on the surveyed exposure – further selected test series should be performed [7]. If the result is positive, a ROAT (Repeated Open Application Test) can also be used to assess relevance. Prick testing and, depending on the history, determination of specific IgEs may be useful in assessing an atopic diathesis. Histological confirmation of the diagnosis may be performed to exclude certain differential diagnoses. However, histologic differentiation, e.g., from psoriasis palmaris, is often very difficult [8]. A mycological examination should rule out a fungal infection at the very beginning of the diagnostic process.
Differential diagnoses
The most important differential diagnoses of chronic hand eczema include psoriasis palmaris, psoriasis pustulosa, tinea manuum, palmoplantar keratoses, lichen planus, and epithelial neoplasms such as actinic keratoses or Bowen’s disease. Artifacts due to manipulation of the skin should also be considered. Furthermore, there are rare differential diagnoses such as scabies, the secondary stage of syphilis or paraneoplastic acrodermatitis psoriasiformis (also known as basex syndrome).
Prevention through skin protection and care
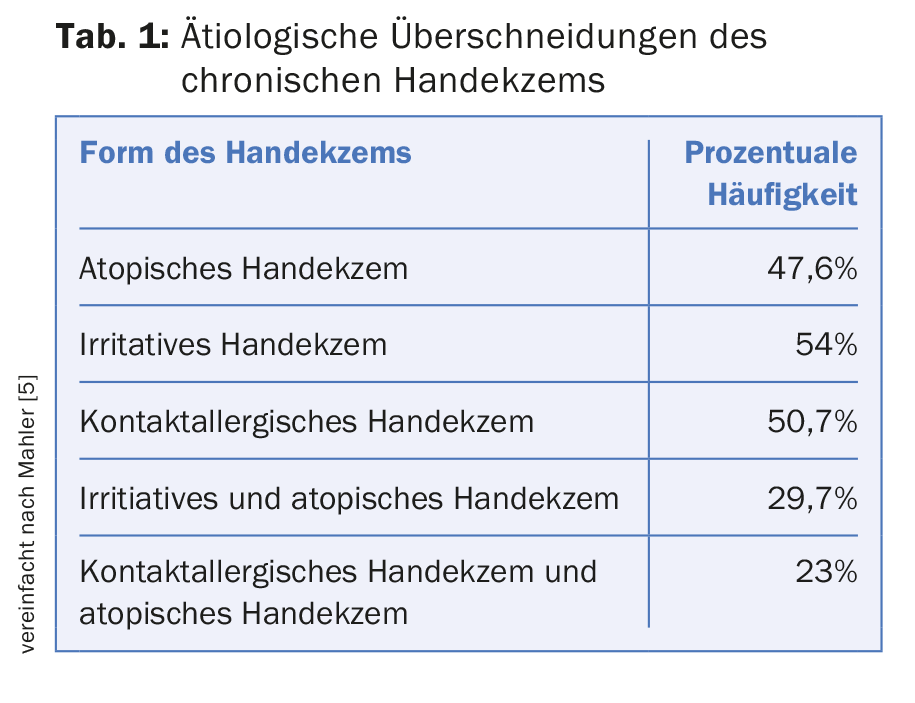
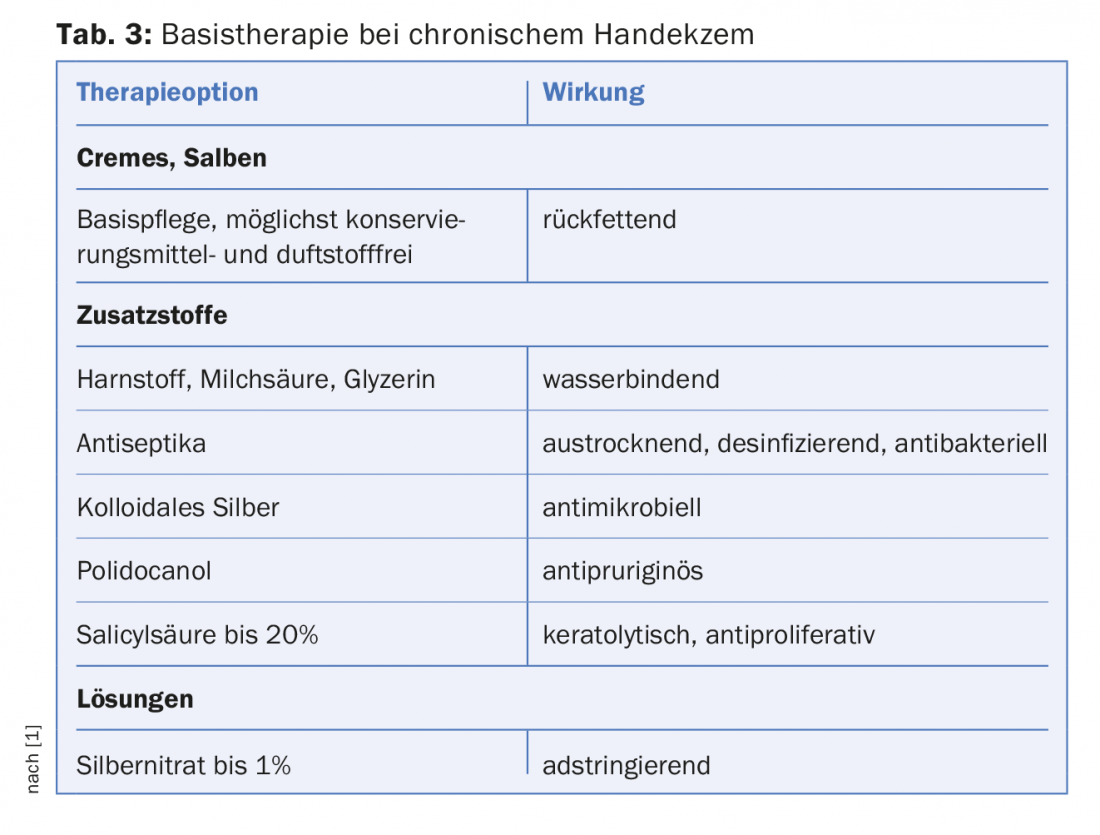
Primary prevention measures are recommended to reduce the incidence of hand eczema. This includes training on skin protection and care (see also www.suva.ch/hautschutz). For minimal lesions, secondary prevention strategies should be implemented early, especially patient education, education on the proper use of skin protection measures (Table 2), and avoidance of contact allergens [7]. Skin care products are recommended for all patients with hand eczema (Table 3).
Therapy
In general, rapid and consistent therapy of acute hand eczema is advised to avoid the development of chronic hand eczema.
Topical glucocorticosteroids play an important role in the treatment of hand eczema. Because their efficacy is evidence-based [10], they are recommended as first-line therapy. They are very effective in acute therapy. It should, for a rapid therapeutic effect, be used with min. Starch class 2 can be started. The time horizon of therapy depends on the potency of the drug, but should not exceed six weeks of continuous therapy. For long-term therapy, interval therapy with two to three days of treatment and four to five days off can be used. Evidence of the efficacy of long-term intermittent therapy with mometasone furoate cream has been demonstrated in clinical trials [11]. However, long-term use may lead to disruption of barrier function and skin atrophy. Contact allergies to topical glucocorticosteroids or ingredients of topical preparations may also occur in rare cases [1].
The topical calcineurin inhibitors takrolimus and pimekrolimus are approved for the treatment of atopic eczema. Takrolimus has been shown to be as effective as mometasone furoate (glucocorticoid), while pimecrolimus appears to be noninferior to a weakly effective topical corticosteroid [12,13]. They are suitable as an adjunct or follow-up therapy to topical glucocorticosteroids and are immunomodulatory and without atrophogenic potential.
UV light therapy: If chronic recurrent hand eczema occurs in adult patients despite first-line therapy with topical glucocorticosteroids, phototherapy can be performed. Clinical studies demonstrate improvement of chronic hand eczema with UVB phototherapy within ten weeks [14]. PUVA therapy was found to be superior in some, but not all, studies. However, long-term use of phototherapy may increase the risk of cutaneous malignancies [15]. In the case of light therapy, the availability as well as the effort for the patient play a major role.
Radiotherapy: In cases of very severe hand eczema unresponsive to topicals and light therapy, treatment with soft X-ray radiation may be considered. However, the long-term side effects of this treatment incl. of the development of cutaneous neoplasms, so that such treatment is not recommended after a risk-benefit analysis [7].
Alitretinoin (Toctino®) is an evidence-based systemic therapy approved for the treatment of severe chronic hand eczema that has been present for more than three months and has persisted for at least three months. four weeks does not respond or responds inadequately to topical glucocorticosteroids. It is considered a second-line therapy. Alitretinoin has anti-inflammatory and immunomodulatory effects and has a regulatory effect on keratinocyte hyperproliferation. The standard dosage is 30 mg/day, and the duration of therapy is three to six months. Early use of therapy achieves more rapid success. The typical side effects of retinoids, especially teratogenicity, must be strictly observed. The duration of continuation of contraception after discontinuation is one month.
Acitretin is a retinoid approved in Switzerland for the treatment of severe cornification disorders, but not for hand eczema. The evidence base for effectiveness is low. It may be considered in hyperkeratotic palmar eczema for patients who require long-term therapy and for whom first- or second-line therapy is not sufficiently effective or is contraindicated [7]. Important with acitretin is strict contraception for another two years after the end of therapy.
Systemic glucocorticosteroids can be used for short-term acute therapy of severe hand eczema. However, they are not suitable for long-term therapy because of the known long-term side effects such as osteoporosis, glaucoma, etc.
Immunosuppressants: cyclosporin is used in refractory, severe chronic hand eczema. Careful monitoring of potential severe side effects including nephrotoxicity, malignancy, hypertension, and increased risk of infection must be observed. It is approved for the treatment of atopic eczema. Azathioprine, methotrexate (MTX), mycophenolate mofetil, and TNF-alpha antagonists are occasionally used off-label. Improvement in findings with azathioprine in atopic eczema and pompholyx (dyshidrotic eczema) has been reported [16]. In case reports, there was evidence of improvement or healing of hand eczema with low-dose MTX, besides reducing the need for systemic glucocorticosteroids [17]. With all these immunosuppressive system therapies, the necessary examinations, especially laboratory chemical parameters, must be performed.
Summary
Chronic hand eczema is a common and socially and occupationally dermatologically relevant condition. They occur more frequently in certain occupational groups and often develop in the course of a person’s professional life. There are different forms of hand eczema, and combinations are often present, so that an exact classification is difficult. An exact anamnesis and diagnostics are elementary. Training on prevention is also important and should be more widely implemented. Various options are available for therapy, depending on the type of hand eczema, its severity, and the patient’s individual wishes and comorbidities.
Take-Home Messages
- Hand eczema is common and has a high social relevance.
- They are differentiated according to etiology, morphology, and time course.
- Elementary are skin protection and care, which form the basis of the therapy.
- Procedures such as prick testing and epicutaneous testing as well as mycological exclusion diagnostics are part of the diagnosis of chronic hand eczema.
- Topical as well as systemic therapy options are available for the early and intensive treatment of hand eczema.
Literature:
- Ballmer-Weber BK, et al: Management of chronic hand eczema: Swiss consensus. Derm Hel 2012; 24: 28-36.
- Apfelbacher CJ, et al: Determinants of current hand eczema: results from case-control studies nested in the PACO follow-up study (PACO II). Contact Dermatitis 2010; 62(6): 363-370.
- Molin S, et al: Filaggrin mutations may confer susceptibility to chronic hand eczema characterized by combined allergic and irritant contact dermatitis. Br J Dermatol 2009; 161(4): 801-807.
- Josefson A, et al: Nickel allergy as risk factor for hand eczema: a population-based study. Br J Dermatol 2009; 160(4): 828-834.
- Mahler V: Skin protection in the healthcare setting. Curr Probl Dermatol 2007; 34: 120-132.
- Janach M, et al: Changing delayed-type sensitizations to the baseline series allergens over a decade at the Zurich University Hospital. Contact Dermatitis 2010; 63(1): 42-48.
- Diepgen TL, et al: Guideline for the diagnosis, prevention and treatment of hand eczema – abridged version. JDDG 2015; 13(1): 77-85.
- Aydin O, et al: Non-pustular palmoplantar psoriasis: is histologic differentiation from eczematous dermatitis possible? J Cutan Pathol 2008; 35(2): 169-173.
- Agner T, Held E: Skin protection programmes. Contact Dermatitis 2002; 47(5): 253-256.
- Coenraads PJ, et al: Interventions for hand eczema. Cochrane Database, resubmitted to the Cochrane Database of Systematic Reviews June 2014.
- Veien NK, et al: Longterm, intermittent, treatment of chronic hand eczema with mometasone furoate. Br J Dermatol 1999; 140(5): 882-886.
- Krejci-Manwaring J, et al: Topical tacrolimus 0.1% improves symptoms of hand dermatitis in patients treated with a prednisone taper. J Drugs Dermatol 2008; 7(7): 643-646.
- Belsito DV, et al: Pimecrolimus cream 1%: a potential new treatment for chronic hand dermatitis. Cutis 2004; 73(1): 31-38.
- Sjovall P, Christensen OB: Treatment of chronic hand eczema with UV-B Handylux in the clinic and at home. Contact Dermatitis 1994; 31(1): 5-8.
- Nijsten TE, Stern RS: The increased risk of skin cancer is persistent after discontinuation of psoralen plus ultraviolet A: a cohort study. J Invest Dermatol 2003; 121(2): 252-258.
- Scerri L: Azathioprine in dermatological practice. An overview with special emphasis on its use in non-bullous inflammatory dermatoses. Adv Exp Med Biol 1999; 455: 343-348.
- Egan CA, et al: Low-dose oral methotrexate treatment for recalcitrant palmoplantar pompholyx. J Am Acad Dermatol 1999; 40(4): 612-614.
DERMATOLOGIE PRAXIS 2018; 28(3): 9-13