Psycho-cardiology makes it clear that mental and cardiovascular diseases are closely linked. Integrated treatment that addresses both aspects is crucial to improving the quality of life of those affected and optimizing the prognosis. Through interdisciplinary cooperation and innovative approaches, psycho-cardiology can make an important contribution to modern medicine.
(red) Cardiovascular disease (CVD) is one of the most common causes of illness and death worldwide. In parallel, depression and other mental disorders are an increasing health burden in modern societies. The link between these two disease areas is becoming increasingly clear, especially in psycho-cardiology, an interdisciplinary approach that studies the interactions between mental and cardiovascular diseases. This shows that depression is not only an independent risk factor for CVD, but can also significantly worsen its prognosis. Conversely, cardiovascular disease often worsens the mental state of those affected, which results in a reciprocal reinforcement of these health problems.
This article highlights the epidemiologic features, pathophysiologic mechanisms, diagnostic challenges and therapeutic approaches of psycho-cardiology. It also outlines future perspectives on how integrated treatment of these comorbidities can improve patients’ quality of life and prognosis.
Introduction to psycho-cardiology
Psycho-cardiology investigates the link between cardiovascular diseases and psychological factors such as depression, anxiety disorders and chronic stress. A well-known example is so-called white coat hypertension, in which blood pressure rises at the mere sight of a doctor in a white coat. Such reactions show how closely mental states and physical functions are linked.
However, this connection goes beyond situational phenomena. Patients with cardiovascular disease, particularly coronary heart disease (CHD), have an increased risk of mental illness. Conversely, psychological stress is a significant risk factor for the development and worsening of CHD. Symptoms such as chest pain, shortness of breath or palpitations are often exacerbated by psychological factors, which makes diagnosis more difficult. In addition, misdiagnosis or inadequate treatment often lead to an excessive burden on the healthcare system and patients.
The therapeutic models of psycho-cardiology pursue a holistic approach that integrates psychological and cardiovascular aspects in prevention, diagnosis and therapy. The aim is to optimize the treatment of both diseases and improve the quality of life of those affected.
Epidemiology: How common are psycho-cardiac diseases?
The link between depression and cardiovascular disease was first systematically described in 1988. Studies show that 25-40% of patients with CHD suffer from depression – a proportion that is significantly higher than in the general population. The role of depression as an independent risk factor is particularly alarming: it not only doubles the risk of coronary events, but also worsens the prognosis after an acute coronary syndrome.
An analysis by the American Heart Association (AHA) in 2014 showed that depression after a heart attack significantly increases the risk of all-cause and cardiovascular mortality. At the same time, the quality of life of these patients is often severely impaired, especially if they have a low socio-economic status and lack social support. Women are disproportionately affected: they show a higher prevalence of stress-induced myocardial ischemia, which may be due to gender-specific differences in coronary structure and hormonal regulation.
Pathophysiological mechanisms of comorbidity
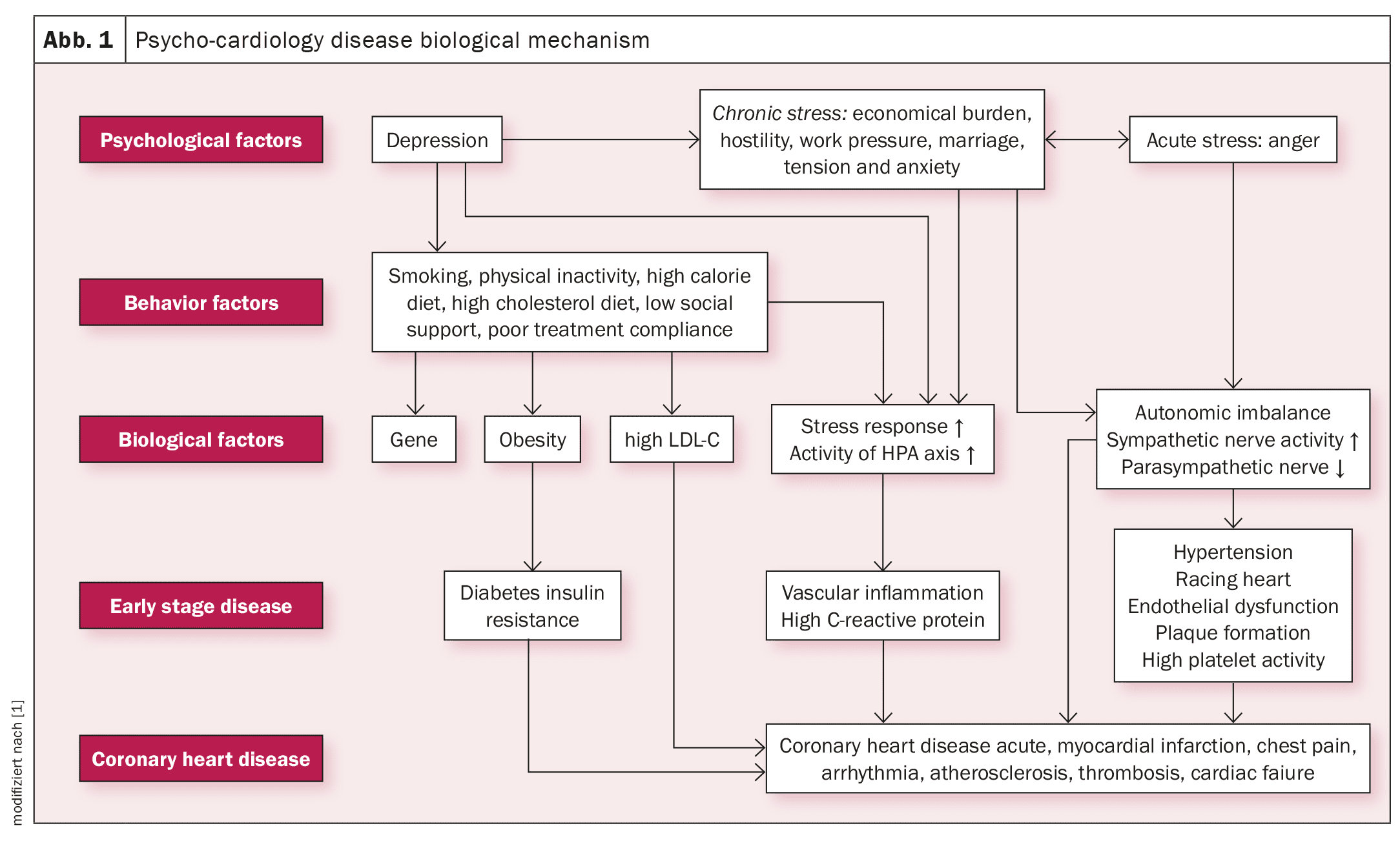
The relationship between mental illness and HKE is based on a complex interaction of different biological and psychological mechanisms:
- Chronic stress and autonomic dysfunction: Chronic stress and depression lead to a permanent activation of the sympathetic nervous system. This increases heart rate, blood pressure and the release of stress hormones such as adrenaline, which can increase oxidative stress and myocardial damage. At the same time, heart rate variability is often reduced in depressed patients, which is associated with a poorer prognosis.
- Inflammation and immune dysfunction: Depression promotes the release of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α). These inflammatory processes are not only involved in the development of arteriosclerosis, but also worsen cardiovascular function.
- HPA axis dysregulation: The hypothalamic-pituitary-adrenal (HPA) axis plays a central role in stress regulation. In depression, the HPA axis is often overactive, which leads to dysregulation of glucose and lipid metabolism, hyperlipidemia and insulin resistance – all of which are risk factors for HD.
- Endothelial dysfunction and platelet activation: Depression impairs endothelial function and increases platelet activity, which increases the risk of arteriosclerotic plaque rupture and thrombosis.
These mechanisms illustrate that depression and cardiovascular disease are not only linked by external factors, but also by common biological pathways.
Challenges in diagnosis
The diagnosis of cardiovascular comorbidities with mental illness is often difficult. The symptoms often overlap: patients with depression report fatigue, chest pain or shortness of breath – symptoms that also occur with cardiovascular disease.
Screening approaches
A staged approach is recommended in order to recognize mental disorders at an early stage:
- Screening questions: Initial assessments such as the “three-question method” help to identify possible psychological stress.
- Psychometric tests: Questionnaires such as the PHQ-9 or the Hospital Anxiety and Depression Scale (HADS ) provide in-depth insights into mental health.
- Multimodal diagnostics: The combination of cardiological tests (e.g. echocardiography) and psychometric analyses enables a differentiated assessment.
Therapeutic approaches
- Psychotherapy: Cognitive behavioral therapy has proven to be effective in treating depression in CHD patients. It helps to recognize negative thought patterns and develop strategies for coping with stress. The therapy should be an integral part of the cardiac rehabilitation program.
- Physical activity: Regular exercise is one of the most effective interventions. Studies show that aerobic exercise reduces depressive symptoms and improves heart function. Even moderate improvements in cardiac fitness can significantly reduce the risk of mortality.
- Pharmacotherapy: Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) are the preferred choice for moderate to severe depression. Drugs such as sertraline have been shown to be safe and effective for patients with CHD. However, potential cardiovascular side effects, such as QT prolongation, must be carefully monitored.
- Interdisciplinary care: A holistic approach that integrates mental and cardiovascular aspects is essential. Interdisciplinary teams of cardiologists, psychiatrists and psychologists should work closely together to optimize care.
Future prospects
Psycho-cardiology is faced with the task of developing innovative treatment approaches. Future research should focus on personalized therapies based on biomarkers and artificial intelligence. In addition, digital health solutions such as telemedicine could help to close the gaps in care and improve aftercare.
Source: Ren Y, Tang H, Zhang L, et al: Exploration of therapeutic models for psycho-cardiology: From cardiac to psychological rehabilitation. Heliyon 2024 Mar 15;10(6): e27484. doi: 10.1016/j.heliyon.2024.e27484. PMID: 38524561; PMCID: PMC10958220.
CARDIOVASC 2024; 23(4): 22-23











