Treatments for psoriasis have been handed down since ancient Greece. Well-tried treatment methods include occlusion, zinc glue dressings, balneotherapy as well as combination therapies with tea substances, dithranol, psoralen as well as light therapies.
Hardly in any other field of dermatology as in skin immunology has so much been developed in recent years. Knowledge of psoriasis has eventually led to a glut of new therapeutic agents. Thus, modern biologics are used to specifically inhibit signal transduction via cytokines (IL-12, IL-23, IL-17, TNFalpha, etc.). In addition, more and more clinical, phenotypic, epidemiological, internistic and psychosomatic aspects are coming into the limelight due to great involvement of clinics and pharmaceutical companies. But what about the tried and tested treatment options for psoriasis? After all, this disease has been treated since ancient Greece. It was mistakenly called leprosy in ancient times, but the stigma is still enormous even today.
Simple occlusion with or without active ingredients
If a psoriasis plaque were occluded with a household foil, it would disappear after four to six weeks. It is well known that local therapy by additional airtight occlusion is more effective, because the penetration of therapeutic substances is increased many times, but occlusion without active substances is also very effective and an independent factor [1]. Plates otherwise used for ulcer therapy, plastic films (Fig. 1), and even Gore-Tex succeed in bringing dry psoriasis lesions, including hyperkeratosis and redness, to healing. Some ingenuity is needed to apply durable films over the joints. If you cut into the edges, this grants some mobility. Certainly, foci in the flexures, weeping lesions, and pustular forms should be treated openly because of possible superinfections and heavy exudate accumulation; psoriatic foci could also become infected under occlusion in diabetic patients.

Zinc glue dressings
Straight moist zinc bandages can be applied well to the extremities (Fig. 2), are cuddly and slightly bendable like a soft plaster, cool and are astringent. They can usually be changed weekly by the patient himself, a steroid cream, for example, can be easily applied underneath; usually the desired result is achieved after four weeks. Follow-up treatments can be applied on a weekly basis as needed. The treatment is simple, perhaps not suitable for the warmest months of the year, but can well accompany other forms of therapy, as especially in the case of the lower leg and elbow outside the treatment successes are delayed.
Coal tar 2% to 20% in petroleum jelly
Magistral formulation with coal tar is an alternative to the use of steroid substances, which is highly effective in the treatment of inflammation as well as skin proliferation tendency. Tar is particularly suitable for the hands and feet, where it can also be applied occlusively for twelve hours at a time (Fig. 3), for example in cotton gloves. Apart from practicality (removal of tar is best done with cellulose wipes) and odor, tar preparations in addition to topical steroids can always be used to achieve improvement without the use of retinoids or immunosuppressants. For example, one should start with a serial treatment 4×12 per week, then reduce to one or two treatments per week as skin conditions improve. There is no carcinogenicity associated with palmoplantar use.

In cloth treatments
To intensify local therapy, after abundant application of ointments, patients can wrap themselves in sheets for 50-60 minutes. The action of the different substances is promoted, the refatting is improved and an adequate amount of local therapy can be applied.
Dithranol UVB narrow band therapy: this anthralin, an anthracene, is introduced in concentrations of 0.1-2% in a paste or cream and used in combination with UVB narrow band therapy. It should be started in low concentration to slowly train the light sensitivity. Also, it works with the time of exposure, which is initially only a minute before it is wiped away. It increases the effectiveness of light therapy enormously and was used extensively, especially in the past during in-patient treatments. There is absolutely nothing wrong with using this therapy in an outpatient setting. However, it should not be used on the face or genitals. Generally, tar derivatives are considered slower in efficacy than topical steroids; this depends on the increases in concentration. The most important and convincing features are the absence of a rebound phenomenon as observed two weeks after topical steroids. Cortisone side effects are notably avoided.
Göckermann therapy: this local tar preparation was first used together with light therapy in 1925 [2] and is based on the same principle of tar’s anti-inflammatory properties and increased sensitivity to UVA and UVB. Due to the higher concentration of 10-20%, coal tar is quite greasy, smelly and staining (the patients are wrapped in sheets for about an hour directly before the light treatment), which is why more and more people have switched to Dithranol – especially in inpatient psoriasis therapy, which lasts a good six weeks. But again, the healing phases last very long, up to a year at most, especially compared to climatic therapy (four weeks) and topical or (actually contraindicated) internal steroids (rebound after two weeks).
System PUVA
System PUVA is the core of outpatient combination therapy. In systemic PUVA therapy, the photosensitizer 8-methoxypsoralen (8-MOP) is administered orally two hours before irradiation. In combination with retinoids, this is the so-called Re-PUVA therapy, which can be used successfully, especially for severely hyperkeratotic foci. A major difficulty is the sensitivity of the eyes to light when taking psoralen, which is why the intake and irradiations are done in the evening, as the patient has to wear sunglasses during daylight, which limits the quality of life.
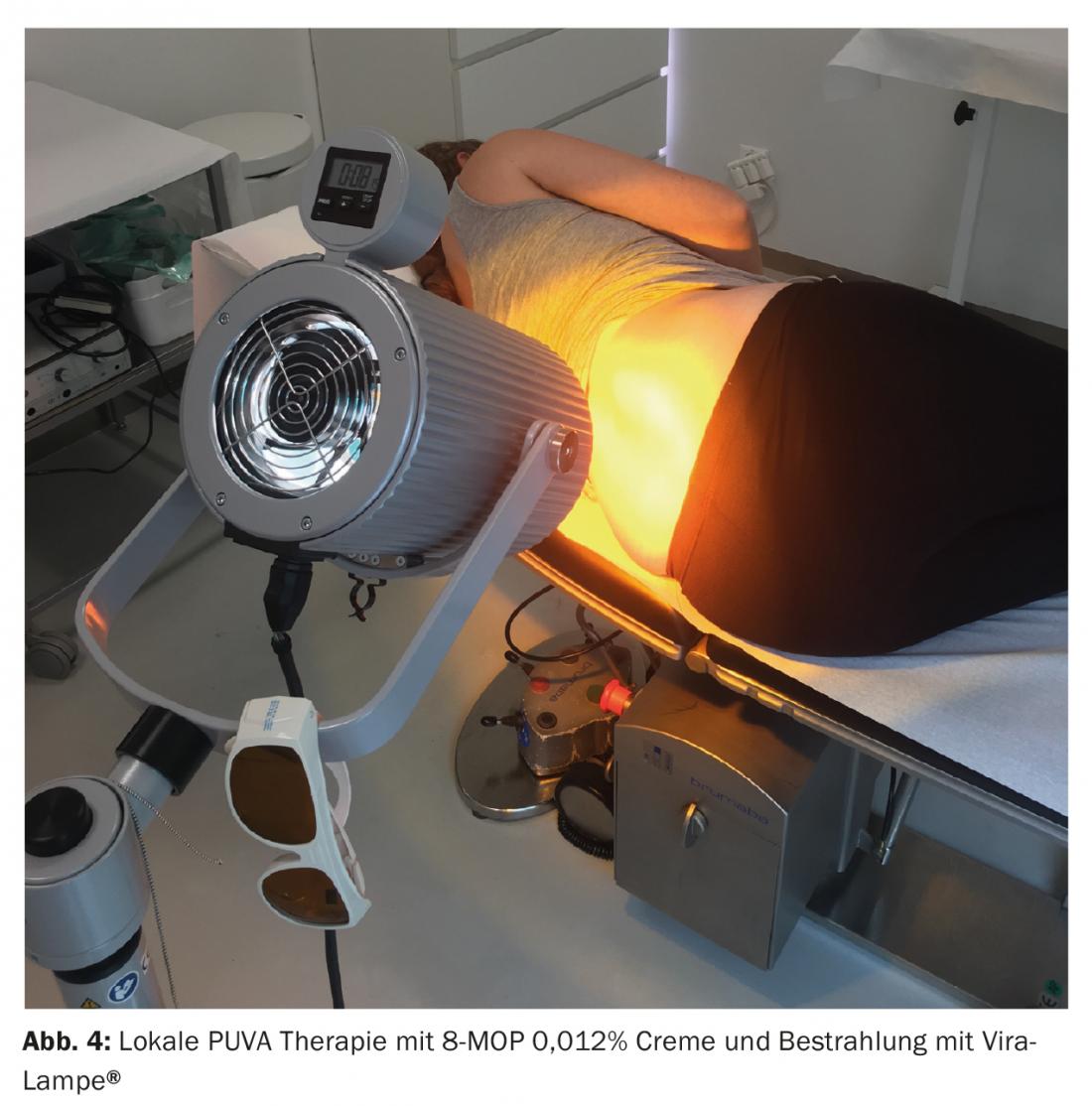
Local PUVA/Cream PUVA
This acts by preparing the skin 30 minutes before irradiation with psoralen as an amplifier of light therapy and its immunosuppression of the skin. The prior bath with psoralen or cream application is done at a concentration of 8-methoxy psoralen 0.009-0.012% [3]. These treatments are particularly suitable for infestation of the hands and feet or other isolated areas that can be treated with a linear UVA radiator (Fig. 4) . The disadvantage is the longer irradiation time of 10-20 minutes. Of advantage, on the other hand, is that it is a natural therapy that can also be combined with retinoids or coal tar; if the response is good, it can be reduced to maintenance therapy with one session weekly or the condition can be maintained with other simple therapies.
Balneotherapy
Unfortunately, balneotherapy has been almost completely abandoned. In inpatient stays, a bathtub is not always available, it is time-consuming and personnel-intensive. There is also a lack of recent studies on the effectiveness of bath therapies. However, the way it works is obvious. In a short time the skin can be desquamated, the water has an astringent effect, if not too warm; it has an antiseptic and antipruritic effect. We have seen miraculous healings after one week of balneotherapy in severely superinfected psoriasis lesions.
What factors play a role here? The fact that many psoriatics have a genetic autostimulated disease is only half the truth; the germ load of the skin should not be neglected either, since these stimulate the disease as so-called superantigens [4]. Staphylococci and Candida in particular have been named as stimulating skin germs. And, of course, internal infections with streptococci are well known as the primary trigger of psoriasis. The latter should be actively sought and treated in any extensive psoriasis. A feeling of relaxation, enjoyment sometimes reduction of itching due to bathing are important factors that contribute to the improvement of this disease.
The additions in balneotherapy vary greatly and are somewhat dependent on public currents. Probably the best known is brine bath therapy, which simulates a sea bath [5]. Other additives are surfactants that clean the skin, antiseptics (e.g.soaps containing triclosan) that also remove the flora of the skin. To relieve itching, wheat bran can be added to the bath. Bath therapy is very good to combine with light therapy.
Climatherapy
In the past, stays at the seaside may have been paid for by supplementary insurance. Undoubtedly, such a stay is effective. Brine baths, heliotherapy, Mediterranean cuisine with plenty of fish oil and at most the possibility of in-cloth treatment with different ointments containing polidocanol (against itching), tar substances (dithranol, coal tar 2%), steroids and/or vitamin D effectively contribute to the healing process. However, healing is often characterized by recurrence after four weeks – when the patient is back home and therapy is not continued.
These services are no longer covered by insurance companies because they are too little controlled, standardized and too costly. Nevertheless, these therapies are recommended.
Nutrition
The recommendations for an appropriate diet that supposedly supports the healing process are anecdotal rather than scientifically based; for example, the addition of vitamin E or D, which are said to be helpful, has been described as exemplary rather than statistically proven. Intake of omega-3 fatty acids (cod liver oil, fish), a low-carbohydrate and low-alcohol diet, and reduction of animal fats are recommended. At least this makes cardiovascular sense.
Take-Home Messages
- Well-tried treatment methods, which often improve the quality of life and have a favorable effect on concomitant diseases, have partly fallen into oblivion.
- Especially accompanying factors like itching and bacterial colonization can be solved very well by balneotherapy.
- Occlusion therapies are simple and can be performed by the patient.
- Combination therapies with tar substances, dithranol and psoralen with or without light therapy can be used in polymorbid patients. They are natural, inexpensive, risk-free – even compared to system therapies.
Literature:
- Vleuten CJ, Vlijmen-Willems IM, et al: Clobetasol-17 propionate lotion under hydrocolloid dressing (Duoderm ET) once weekly versus unoccluded clobetasol-17-propionate ointment twice daily in psoriasis: an immunohistochemical study on remission and relapse. Arch Dermatol Res 1999; 291(7-8): 390-395.
- Petrozzi JW: Goeckerman regimen for psoriatic patients refractory to biologic therapy. J Am Acad Dermatol 2014; 71(1): 195.
- Steinmeyer K, Grundmann-Kollmann M, et al: Treatment of plaque-type psoriasis with cream-PUVA therapy. Dermatologist 2001; 52(10): 885-887.
- Balci DD, Duran N, et al: High prevalence of Staphylococcus aureus cultivation and superantigen production in patients with psoriasis. Eur J Dermatol 2009; 19(3): 238-242.
- Gambichler T, Demetriou C, et al: The impact of salt water soaks on biophysical and molecular parameters in psoriatic epidermis equivalents. Dermatology. 2011; 223(3): 230-238.
DERMATOLOGIE PRAXIS 2017; 27(5): 13-17











